Introduction
Low linear energy transfer (LET)-radiation,
including X-rays and electron beams from linear accelerators, is
used worldwide for clinical radiotherapy. However, the therapeutic
effect of radiotherapy using linear accelerators for relatively
large tumors of more than several centimeters in diameter,
decreases to one third than that for smaller tumors due to the
presence of numerous hypoxic tumor cells and an abundance of
anti-oxidative enzymes including peroxidase and catalase (1). This reduction occurs because
approximately two thirds of the therapeutic effect of linear
accelerators is due to the indirect effects of X-rays and/or
electrons, which are mainly caused by radical formations such as
hydroxyl radicals in the cytoplasm produced by radiation
degradation of the intrabody and intracellular water molecules
(1). Therefore, in the absence of
oxygen in the tumor tissues, the effect of the X-rays and electrons
decreases to one third of standard efficacy. In these situations,
the use of a low concentration of hydrogen peroxide for low
LET-radioresistant neoplasms causes anti-oxidative enzymes in the
tumor tissues, including peroxidase and catalase, to be inactivated
and, concomitantly, oxygen is produced by the degradation of
hydrogen peroxide, thereby resulting in the hypoxic tumor tissue
being reoxygenated.
Strong radiosensitizing effects of hydrogen peroxide
have been demonstrated in this experimental study using the low
LET-radioresistant osteosarcoma cell line HS-Os-1 (2–4) and a
radioresistant prostatic cancer cell line (5). On the basis of these experimental
results, a novel enzyme-targeting radiosensitization treatment
termed Kochi Oxydol-Radiation Therapy for Unresectable Carcinomas
(KORTUC) was developed. In KORTUC I, which uses a hydrogen peroxide
solution (Oxydol)-soaked gauze bolus, notable therapeutic effects
of hydrogen peroxide as a radiosensitizer for superficially exposed
and unresectable neoplasms were obtained, as reported in a previous
study (6).
The most effective method of injecting hydrogen
peroxide into tumor tissue was then examined. This proved difficult
as 3% w/v hydrogen peroxide solution (Oxydol) is an antiseptic
agent for skin lesions, and thus injection into an affected lesion
may result in hydrogen peroxide soaking into a body cavity and
possibly causing an intra-arterial oxygen embolism. Regarding
intratumoral hydrogen peroxide injection (7), 3–5 ml of 3% w/v Oxydol was
administered for meningioma with no significant side effects.
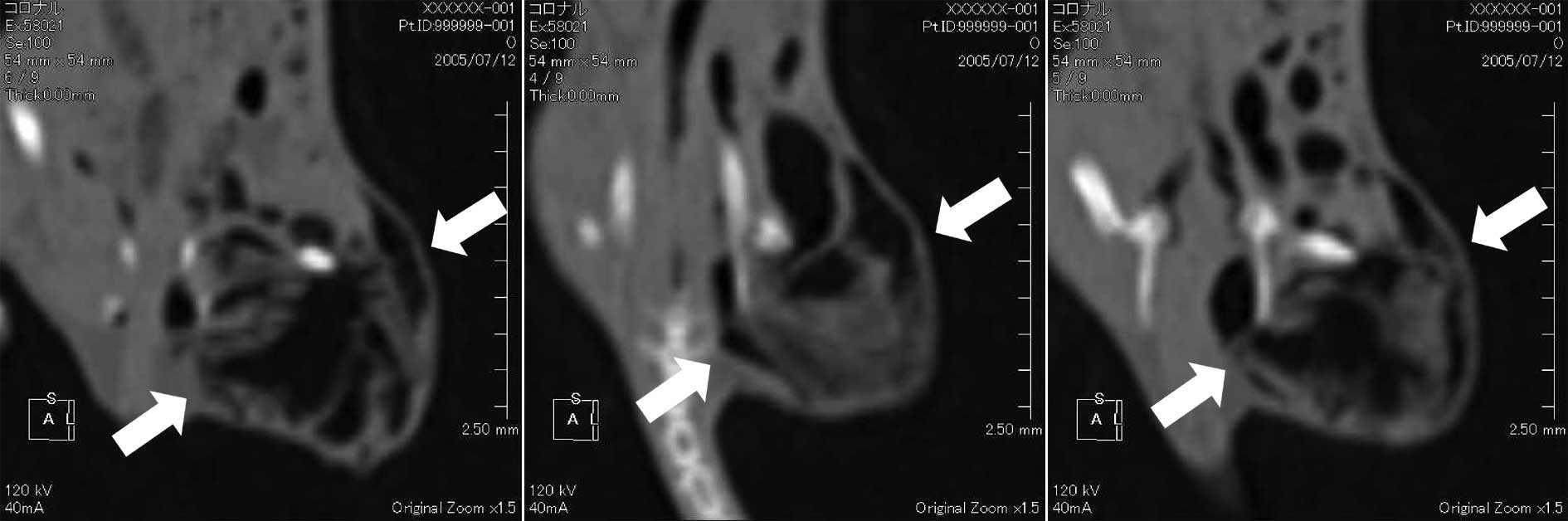
Notably, the formation of oxygen bubble following an intratumoral
injection of 1 ml of 0.5% w/v hydrogen peroxide into mice tumors
using multi-row detector computerized tomography (MDCT) was
confirmed (Fig. 1).
Local pain appeared to be strong as the hydrogen
peroxide was rapidly degraded by the peroxidase and catalase in the
tumor tissue. Furthermore, the diffusion of hydrogen peroxide into
surrounding tissues necessitates frequent injections to maintain
the oxygen concentration in the tumor tissue, if hydrogen peroxide
is used alone. However, if the local pain can be relieved and the
oxygen concentration in the tumor can be maintained for at least 24
h following an intratumoral injection of hydrogen peroxide, patient
stress can be largely reduced by lowering the frequency of hydrogen
peroxide injections.
This study therefore aimed to identify the most
effective combination of drugs containing hydrogen peroxide for
relief of local pain at the injection site and to preserve high
intratumoral oxygen concentration.
Materials and methods
Drug/agent combinations
To examine various drug/agent combinations, PBS
alone (control), PBS containing 0.5% w/v hydrogen peroxide
(PBS-hydrogen peroxide), 0.8% w/v sodium hyaluronate containing
0.5% w/v hydrogen peroxide (hyaluronate-hydrogen peroxide), 0.8%
w/v liposome containing 0.5% w/v hydrogen peroxide
(liposome-hydrogen peroxide), 0.8% w/v gelatin (Gelpart) containing
0.5% w/v hydrogen peroxide (gelatin-hydrogen peroxide) and 0.8% w/v
glycerol containing 0.5% w/v hydrogen peroxide (glycerol-hydrogen
peroxide) were prepared immediately prior to the injection of each
agent. First, ~105 SCCVII tumor cells were inoculated
into the right thigh of each C3H/He mouse. Once each tumor had
grown to ~10 mm in diameter, an intratumoral injection of 0.25 ml
of one of the drug combinations mentioned above was administered.
The intratumoral oxygen concentration was then measured using
IMP-211 apparatus (Inter Medical Co., Ltd., Japan) immediately, 1
and 24 h after injection of the test agents.
Test agents
ARTZ dispo
ARTZ dispo is the injection agent for sodium
hyaluronate for knee joints and has been shown to improve joint
function (8). This agent contains
sodium hyaluronate at a concentration of 1% w/v, and has
therapeutic effects for chronic osteoarthritis of knee joints,
frozen shoulder and knee pain due to rheumatoid arthritis. ARTZ
dispo protects the joint tissue by covering the latter and by
improving lubrication. This injection agent soaks into degenerating
cartilage, thereby inhibiting degeneration of cartilage and
improving its metabolism. Moreover, ARTZ dispo permeates into the
synovial tissue to control inflammation and degenerative changes,
and consequently relieves pain. This product provides remission of
pain, an increase in daily life activities, and improvement in the
range of motion in the joint.
Gelpart
Gelpart is porous gelatin composed of gelatin and
the embolus medicine used for transcatheter arterial embolization
therapy for hepatocellular carcinoma patients (9). The effect of a long-term embolization
is evident for several days to weeks. Gelpart physically forms an
embolus on the intravascular lumen of the hepatic artery that
provides nourishment to the tumor through a catheter. Therefore,
Gelpart induces tumor avascular necrosis.
Liposomes
Liposomes are closed endoplasmic reticula (ER) that
form when phosphatide, the ER architectural component, is dissolved
in water (10). Liposomes are used
as a drug delivery system, i.e., technologies that deliver the
amount of medicine required to the relevant part of the body at the
appropriate time. The drug can be sent to a specific part of the
body by enclosing the medicine in a film or in the corpuscle that
forms when a lipid is distributed in water.
Glycerol
Glycerol is a concentrated glycerin and fructose
injection liquid used to treat intracranial hypertension and
intracranial edema when there is a reduction in brain capacity
during cerebral surgery and when a decrease in the pressure of the
interior of the eye is required (11). Glycerin dissolves slightly in ether
and easily in water and is highly hygroscopic. Moreover, by
hyperosmosis dehydration action, glycerin channels edema fluid to
the blood vessels from brain tissues by raising the osmotic
pressure of the blood when administered intravenously. Therefore,
it is used widely as a therapeutic agent for acute strokes.
IMP-211
The IMP-211 oxygen concentration monitor is used to
measure oxygen concentration, based on polarography. Polarography
is an electrolytic analysis, in which adequate voltage is applied
between the working and reference electrodes in order to conduct
electrolysis. The current that flows in the electrodes is then
measured, thereby obtaining a voltage-current characteristic curve.
Utilizing the chemical reaction described below, the diffusion
current is measured and then converted into oxygen concentration.
Platinum is used as the working electrode and Ag-AgCl is used as
the reference electrode. Platinum consumes oxygen, allowing for
current to flow. Based on the correlation between the consumption
of oxygen and the current, the oxygen concentration can be
measured. Furthermore, the electrode tip is coated with a special
polymeric membrane in such a manner that only oxygen molecules are
able to pass through this membrane to cause the reaction. However,
this polymer membrane is extremely thin and easily damaged.
Results
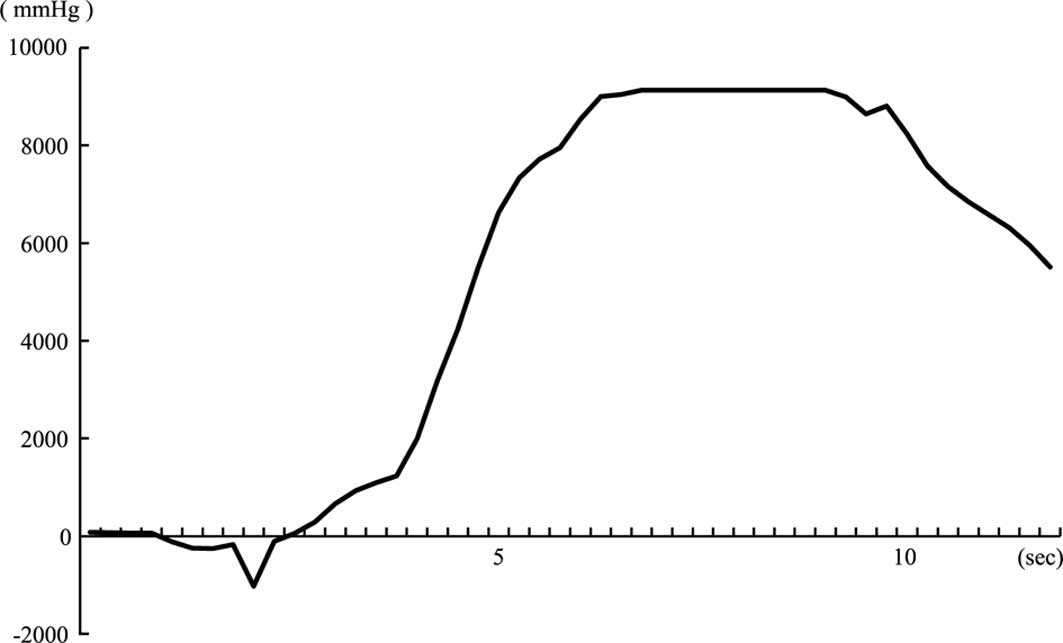
Fig. 2 shows the
oxygen concentration obtained immediately following intratumoral
injection of PBS containing 0.5% w/v hydrogen peroxide. The oxygen
concentration increased rapidly ~4 sec following the intratumoral
injection of PBS-hydrogen peroxide.
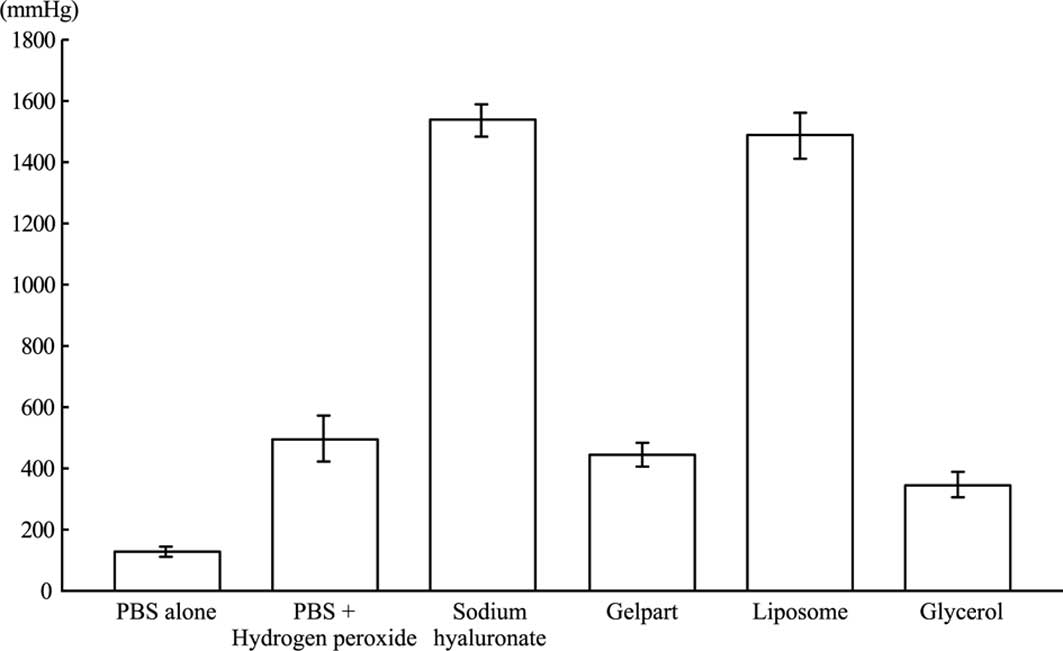
The oxygen concentrations in the tumor tissues at 1
h after injection of each test agent are shown in Fig. 3. Although the oxygen concentrations
in the tumor tissues had decreased compared with that of each test
agent received immediately after the intratumoral injection, the
oxygen concentrations were higher than the control group (PBS
alone) for all agents. Furthermore, the hyaluronate-and
liposome-hydrogen peroxide-injected groups were found to preserve
high intratumoral oxygen pressure.
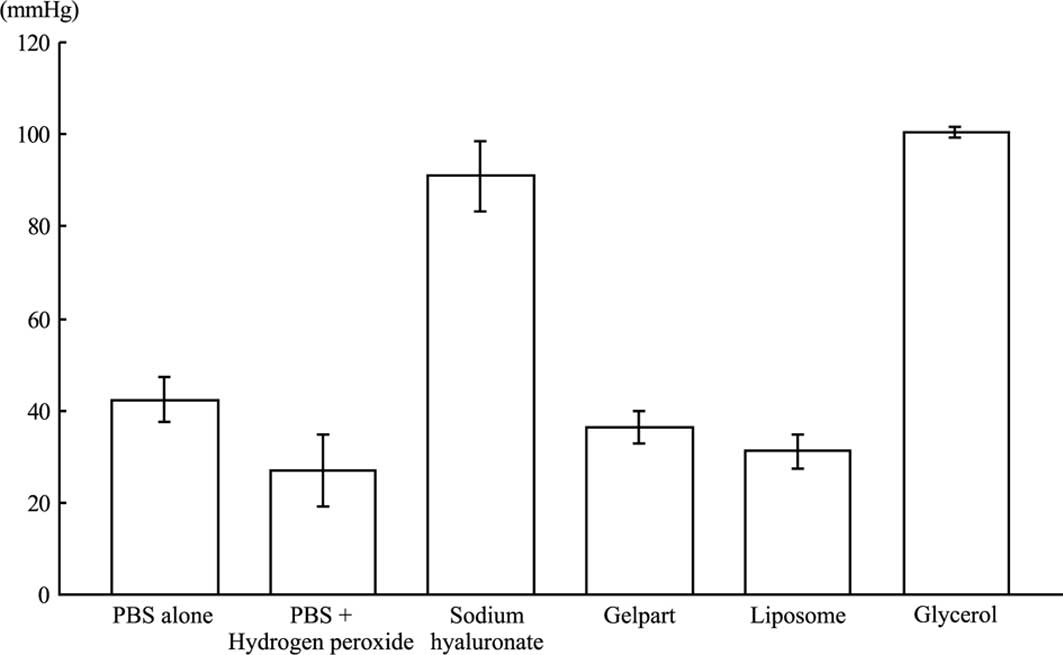
Fig. 4 shows the
oxygen concentrations in the tumor tissues at 24 h after the
injection of each test agent. In the liposome-hydrogen
peroxide-injected group, which had shown a high oxygen
concentration 1 h after injection of the agent, the oxygen
concentration had decreased to the level of the control group by 24
h. The hyaluronate-and glycerol-hydrogen peroxide-injected groups
were the only groups to show preserved high intratumoral oxygen
pressure at 24 h after injection.
Thus, hyaluronate-hydrogen peroxide was identified
as the most effective combination of drugs containing hydrogen
peroxide to preserve high intratumoral oxygen concentration for 24
h following intratumoral injection of the agent.
Discussion
This study showed that intratumoral injection of
hydrogen peroxide rapidly raises the oxygen concentration in the
tumor tissue. Since hydrogen peroxide rapidly diffuses to the
surrounding tissues, alone it results in only short-lived effects
in terms of preservation of a high oxygen concentration in tumor
tissue. At present, clinical radiotherapy is generally performed
five times per week, and thus the development of a long-acting
radiosensitizer for intratumoral injection is essential in order to
decrease injection frequency. Moreover, the development of a
radiosensitizer for intratumoral injection that can maintain a high
oxygen concentration in the tumor tissue for more than 24 h is
crucial. Its significance is due to the frequency of radiotherapy,
since if the high oxygen concentration induced by the
radiosensitizer is maintained from the Monday of the first
radiotherapy to the Tuesday of the second radiotherapy, the
frequency of injection of the radiosensitizer can be reduced to a
twice-weekly basis. This reduction would be the preferred injection
schedule for patients and clinicians.
At 1 h following intratumoral injection of each
agent, the hyaluronate-and liposome-hydrogen peroxide-injected
groups showed high oxygen concentrations in the tumor tissue, while
at 24 h it was the hyaluronate-and glycerol-hydrogen
peroxide-injected groups that showed high oxygen concentrations in
tumor tissue. Thus, the most suitable combination of drugs for
preserving a high intratumoral oxygen concentration is
hyaluronate-hydrogen peroxide.
In general, sodium hyaluronate is utilized in
cosmetic surgery (12) and chronic
articular disorders (13), and
under normal healthy conditions is found in the eyes, skin and
joints. Therefore, sodium hyaluronate can be safely injected into
the human body and when used as a medicine it has a
pain-controlling effect. Moreover, absorption of sodium hyaluronate
occurs gradually due to its strong water-holding capacity and thus
its ability to maintain oxygen levels by retarding the degradation
of hydrogen peroxide over a long period of time, thereby
maintaining the oxygen concentration in tumor tissues.
The glycerol-hydrogen peroxide-injected group also
maintained oxygen concentration in the tumor tissue at 24 h
following injection of the agent. Glycerol is a concentrated
glycerin and fructose injection liquid that is readily dissolved in
water and is highly hygroscopic. Thus, glycerol-hydrogen peroxide
would also be effective in maintaining tumor oxygen concentration.
However, the pain-relieving effects of hyaluronate-hydrogen
peroxide render it the more useful agent in the clinical
setting.
In conclusion, we found that sodium hyaluronate was
the most effective supporting agent for hydrogen peroxide in
maintaining the oxygen concentration in tumor tissues following
intratumoral injection of the hydrogen peroxide agent and for pain
relief at the intratumoral injection site. Based on these results,
clinical application of a novel enzyme-targeting radiosensitization
treatment, known as KORTUC, has begun chiefly for malignant tumors
such as advanced breast cancer, soft tissue sarcoma and cervical
lymph node metastasis and has demonstrated marked therapeutic
effects (14). Moreover, we have
developed KORTUC III for locally advanced hepatocellular carcinoma,
and KORTUC IV for locally advanced pancreatic cancer (stage
IVa).
References
|
1
|
Hall EJ: The oxygen effect and
reoxygenation. Radiobiology For The Radiologist. Hall EJ: 5th
edition. J.B. Lippincott Co; Philadelphia, PA: pp. 91–111. 2000
|
|
2
|
Ogawa Y, Takahashi T, Kobayashi T, et al:
Mechanism of apoptotic resistance of human osteosarcoma cell line,
HS-Os-1, against irradiation. Int J Mol Med. 12:453–458.
2003.PubMed/NCBI
|
|
3
|
Ogawa Y, Takahashi T, Kobayashi T, et al:
Apoptotic-resistance of the human osteosarcoma cell line HS-Os-1 to
irradiation is converted to apoptotic-susceptibility by hydrogen
peroxide: A potent role of hydrogen peroxide as a new
radiosensitizer. Int J Mol Med. 12:845–850. 2003.PubMed/NCBI
|
|
4
|
Ogawa Y, Takahashi T, Kobayashi T, et al:
Immunocytochemical characteristics of human osteosarcoma cell line
HS-Os-1: Possible implication in apoptotic resistance against
irradiation. Int J Mol Med. 14:397–403. 2004.
|
|
5
|
Kariya S, Sawada K, Kobayashi T, et al:
Combination treatment of hydrogen peroxide and X-rays induces
apoptosis in human prostate cancer PC-3 cells. Int J Radiat Oncol
Biol Phys. 75:449–454. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Ogawa Y, Ue H, Tsuzuki K, et al: New
radiosensitization treatment (KORTUC I) using hydrogen peroxide
solution-soaked gauze bolus for unresectable and superficially
exposed neoplasms. Oncol Rep. 19:1389–1394. 2008.
|
|
7
|
Lichtenbaum R, De Souza AA and Jafar JJ:
Intratumoral hydrogen peroxide injection during meningioma
resection. Neurosurgery. 59(Suppl 4): 470–473. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Goto M, Hanyu T, Yoshio T, et al:
Intra-articular injection of hyaluronate (SI-6601D) improves joint
pain and synovial fluid prostaglandin E2 levels in rheumatoid
arthritis: a multicenter clinical trial. Clin Exp Rheumatol.
19:377–383. 2001.PubMed/NCBI
|
|
9
|
Yamada R, Sawada S, Uchida H, et al:
Clinical study of porous gelatin sphere (YM670) in transcatheter
arterial embolization. Jpn J Cancer Chemother. 32:1431–1436.
2005.PubMed/NCBI
|
|
10
|
Teichert J, Kern HJ, Tritschler H, et al:
Investigations on the pharmacokinetics of alpha-lipoic acid in
healthy volunteers. Int J Clin Pharmacol Ther. 36:625–628.
1998.PubMed/NCBI
|
|
11
|
Sakamaki M, Igarashi H, Nishiyama Y, et
al: Effect of glycerol on ischemic cerebral edema assessed by
magnetic resonance imaging. J Neurol Sci. 209:69–74. 2003.
View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Brandt FS and Cazzaniga A: Hyaluronic acid
gel fillers in the management of facial aging. Clin Interv Aging.
3:153–159. 2008.PubMed/NCBI
|
|
13
|
Karatosun V, Unver B, Ozden A, et al:
Intra-articular hyaluronic acid compared to exercise therapy in
osteoarthritis of the ankle. A prospective randomized trial with
long-term follow-up. Clin Exp Rheumatol. 26:288–294.
2008.PubMed/NCBI
|
|
14
|
Ogawa Y, Kubota K, Ue H, et al: Phase I
study of a new radiosensitizer containing hydrogen peroxide and
sodium hyaluronate for topical tumor injection: A new
enzyme-targeting radiosensitization treatment, Kochi
Oxydol-Radiation Therapy for Unresectable Carcinomas, Type II
(KORTUC II). Int J Oncol. 34:609–618. 2009. View Article : Google Scholar
|