Introduction
Malignant glioma is the most common subtype of
primary brain tumors. Glioblastoma multiforme, the most malignant
glioma subtype, is associated with a median survival duration in
the range of 6–18 months (1,2). Due
to their specific properties, including infiltrative growth and
resistance to tumoricidal agents, numerous advances in conventional
therapeutic approaches, such as extensive surgical excision and
adjuvant radio- and chemotherapy have been unsuccessful (3,4). This
poor outcome relates, at least in part, to the inability to deliver
therapeutic agents to the tumor (5). Accumulating evidences of tropism of
stem cells for malignant glioma (6)
show that gene therapies, using stem cells as the vehicles for
therapeutic agents, have emerged as a promising treatment modality
for malignant glioma. Furthermore, a number of pre-clinical trials
of stem cell-based gene therapies have shown that neural stem cells
(NSCs) are effective tumor-specific delivery vehicles for
transgenes to malignant glioma (7–12).
Similarly, evidence indicated that bone marrow-derived mesenchymal
stem cells (MSCs) are effective vehicles for the delivery of gene
therapies to malignant glioma (5,13). In
previous studies, the extensive tropism of NSC and MSC for
malignant glioma was observed, as well as a sufficient effect of
the gene therapy using a suicide gene, the herpes simplex
virus-thymidine kinase (HSVtk) gene, and a prodrug, ganciclovir
(GCV) (14–18).
The mechanism underlying the tropism of NSC and MSC
for tumors in general, and malignant gliomas in particular, has
recently been identified as including soluble factors, cell
adhesion molecules and extracellular matrix components (19–22).
Malignant gliomas produce growth factors, cytokines and chemokines,
which then mediate the tropism of NSC and MSC for malignant glioma.
Previous studies using in vitro migration assays suggested
that the exposure of NSC and MSC to specific growth factors,
particularly stem cell factor (SCF) (21), platelet-derived growth factor BB
(PDGF-BB) (22), stromal-derived
factor-1α (SDF-1α) (19) and
vascular endothelial growth factor (VEGF) (20), enhanced the migration of NSC and MSC
(19–22).
Induced pluripotent stem (iPS) cells have been
established both in rodents and humans, and various pre-clinical
studies have been performed in the field of regeneration therapy
(23). As previously noted, NSCs
and MSCs are excellent vehicles for gene delivery to gliomas. Thus,
the use of iPS cells from patients is likely to be more ideal in
terms of the quality control of the cells and the invasiveness of
cell collection. In the present study, the tumor-tropic activity of
iPS cells was examined to evaluate whether the cells could be
utilized as vehicles for glioma gene therapies.
Materials and methods
Cell culture
The mouse iPS cells, iPS-MEF-Ng-20D-17 established
by Yamanaka et al (23),
were obtained from Riken Biosource Center (Tsukuba, Japan) and were
cultured on mitotically inactivated mouse embryonic fibroblasts in
the medium composed of Dulbecco’s modified Eagle’s medium (DMEM)
high glucose 1X (Invitrogen, Tokyo, Japan) supplemented with 15%
fetal bovine serum (FBS; Sigma-Aldrich Japan, Tokyo, Japan), 0.1 mM
MEM non-essential amino acids (Invitrogen), 0.1 mM
2-mercaptoethanol (Sigma-Aldrich Japan) and 1,000 U/ml leukemia
inhibitory factor (ESGRO; Millipore, Temecula, CA, USA) on a
gelatin-coated dish at 37°C in a 5% CO2 humidified
atmosphere according to the protocol previously reported (24). Experiments were performed using the
mouse iPS cells during passages 2–4. The mouse glioma cell line
GL261 and the rat glioma cell line C6 were purchased from Health
Science Research Resources Bank (Osaka, Japan), and the human
glioma cell lines A172, T98G, YKG1 and U87 from the American Type
Culture Collection (ATCC, Manassas, VA, USA). The cells were grown
in DMEM (Sigma-Aldrich, Japan) supplemented with 10% FBS,
penicillin (100 IU/ml) and streptomycin (100 μg/ml) at 37°C in a
humidified atmosphere of 5% CO2. The mouse iPS cells
were dissociated at 37°C for 2 min using 0.25% trypsin with 1 mM
EDTA, and the glioma cell lines were dissociated using 0.25%
trypsin with 1 mM EDTA for 3 min.
Migration of induced pluripotent stem
cells towards the glioma-conditioned media and specific growth
factors
The in vitro migratory capacity of iPS cells
was assessed using the 24-well Matrigel Invasion Chamber (BD
Biosciences Discovery Labware, Bedford, MA, USA), which contained
an 8-μm pore size PET membrane treated with Matrigel Basement
Membrane Matrix in the insert (25). First, 0.5 ml DMEM was added to the
interior of the inserts and the bottom of the wells and allowed to
rehydrate for 2 h at 37°C in a 5% CO2 humidified
atmosphere. The DMEM was then carefully removed without disturbing
the layer of Matrigel Matrix on the membrane. The mouse iPS cells
were washed twice in phosphate-buffered saline (PBS) and
resuspended to 1×105 cells/ml. Cell suspension (0.5 ml)
(5×104 cells) was added to the upper insert. The lower
chamber was filled with 0.75 ml of conditioned medium (CM) of the
glioma cell lines as well as unconditioned medium (DMEM) as a
control. CM was obtained by collecting, centrifuging and filtering
medium from GL261, C6, A172, T98G, YKG1 and U87 clones
(1×106), which were cultured in 10 ml of DMEM without
FBS for 48 h. For the migration stimulation assays, the specific
growth factors SCF, PDGF-BB, SDF-1α and VEGF were added to the
lower chamber at concentrations from 0.1 to 100 ng/ml. For the
specific growth factors blocking experiments, CM from the GL261
mouse glioma cell line was incubated with anti-SCF, anti-PDGF-BB,
anti-SDF-1α and anti-VEGF neutralizing antibodies (Abcam PLC,
Tokyo, Japan) for 3 h prior to transfer into the lower chamber at
concentrations of 1 and 10 μg/ml.
Following incubation of the Matrigel Invasion
Chambers for 24 h at 37°C in a 5% CO2 humidified
atmosphere, the non-invading cells and/or Matrigel Matrix were
removed from the upper surface of the membrane in the inserts with
a cotton swab. The cells migrating to the lower surface of the
membrane were stained with the Diff-Quick kit (International
Reagents, Hyogo, Japan), which was achieved by sequentially
transferring the inserts to air dry. The nuclei of the migrated
cells were counted in 4 high-power fields (HPF) per membrane using
a magnification of ×200. All experiments were conducted in
triplicate and results were expressed as the mean number of cells
migrating per field ± SD.
Expression of the receptors for growth
factors
The status of the growth factor receptors of mouse
iPS cells was analyzed by reverse transcriptase-polymerase chain
reaction (RT-PCR). The receptors used for the growth factors SCF,
PDGF-BB, SDF-1α and VEGF were c-Kit, intercellular adhesion
molecule-1 (ICAM-1), CXC chemokine receptor 4 (CXCR4) and vascular
endotherial growth factor receptor 2 (VEGFR2), respectively. Total
RNA was extracted from the mouse iPS cells and from the control
mouse fibroblasts using TRIzol reagent (Invitrogen) according to
the manufacturer’s instructions. cDNA was generated from 1 μg of
total RNA from each sample. The primers used were: c-Kit, forward,
5′-CAGAGGCTTAGCGGAGTGAAGTG-3′ and reverse,
5′-TCCCTGGATTGGCAGCATTAC-3′; ICAM-1, forward,
5′-AACTGTGGCACCGTGCAGTC-3′ and reverse, 5′-AGGG
TGAGGTCCTTGCCTACTTG-3′; CXCR4, forward, 5′-CCG
GTACCTCGCTATTGTCCAC-3′ and reverse, 5′-GGATCCAG ACGCCCACACATAGA-3′;
VEGFR2, forward, 5′-TCTCC GTTATTGCTTCTGTTAG-3′ and reverse,
5′-GTGATACC TTGCACAGAGTGACAC-3′; β-actin, forward, 5′-TCAGGT
CATCACTATCGGCAAT-3′ and reverse, 5′-AAAGAAAGGGT GTAAAACGCA-3′. The
PCR conditions consisted of an initial denaturation at 94°C for 2
min followed by 30 cycles of denaturation at 94°C for 30 sec,
annealing at 50°C for 30 sec and extension at 72°C for 30 sec in a
thermal cycler (LightCycler, Roche Diagnostics K.K., Tokyo, Japan).
The integrated density values were determined by extrapolation
using the cRNA standard curve, and normalized with that of β-actin.
The fold increase was calculated from the results of three
independent experiments.
Statistical analysis
The data (mean ± SD) were analyzed using the
two-tailed unpaired Student’s t-test with 95% confidence interval
for a two-group comparison. Differences were considered significant
at p<0.01.
Results
Migration of induced pluripotent stem
cells towards the glioma-conditioned media and specific growth
factors
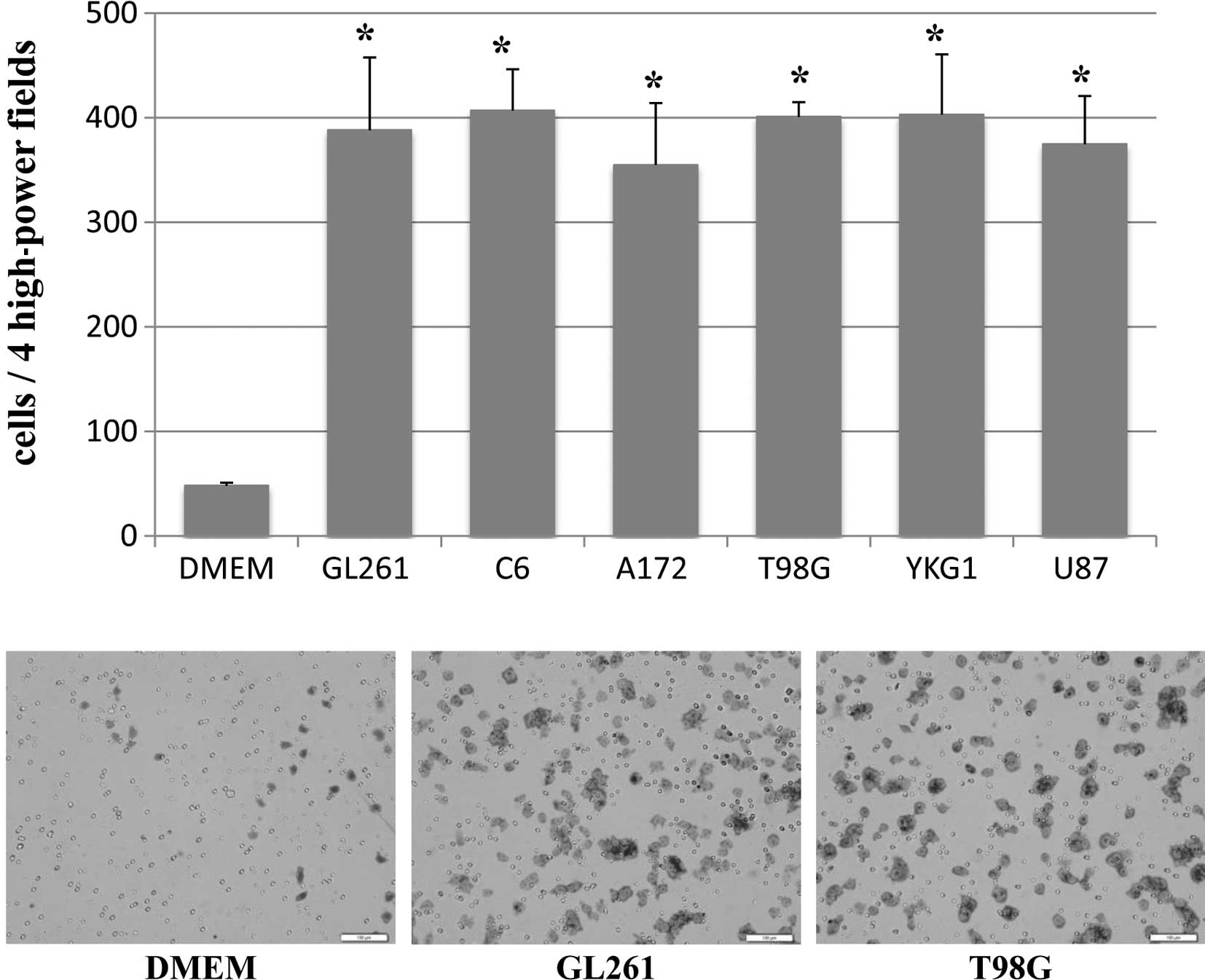
Directional migration of mouse iPS cells towards the
CM prepared from six different glioma cell lines (GL261, C6, A172,
T98G, YKG1 and U87) was analyzed using the 24-well Matrigel
Invasion Chamber. A high number of mouse iPS cells were observed
migrating towards the CM of GL261, C6, A172, T98G, YKG1 and U87
(388±70, 407±40, 355±59, 401±14, 403±58 and 375±46 per 4HPF,
respectively), whereas few cells migrated towards the unconditioned
medium with or without FBS (89±6 and 48±3 per 4HPF, respectively)
(Fig. 1). Every CM from glioma cell
lines significantly stimulated the directional migration of mouse
iPS cells compared to unconditioned medium with or without FBS
(p<0.001).
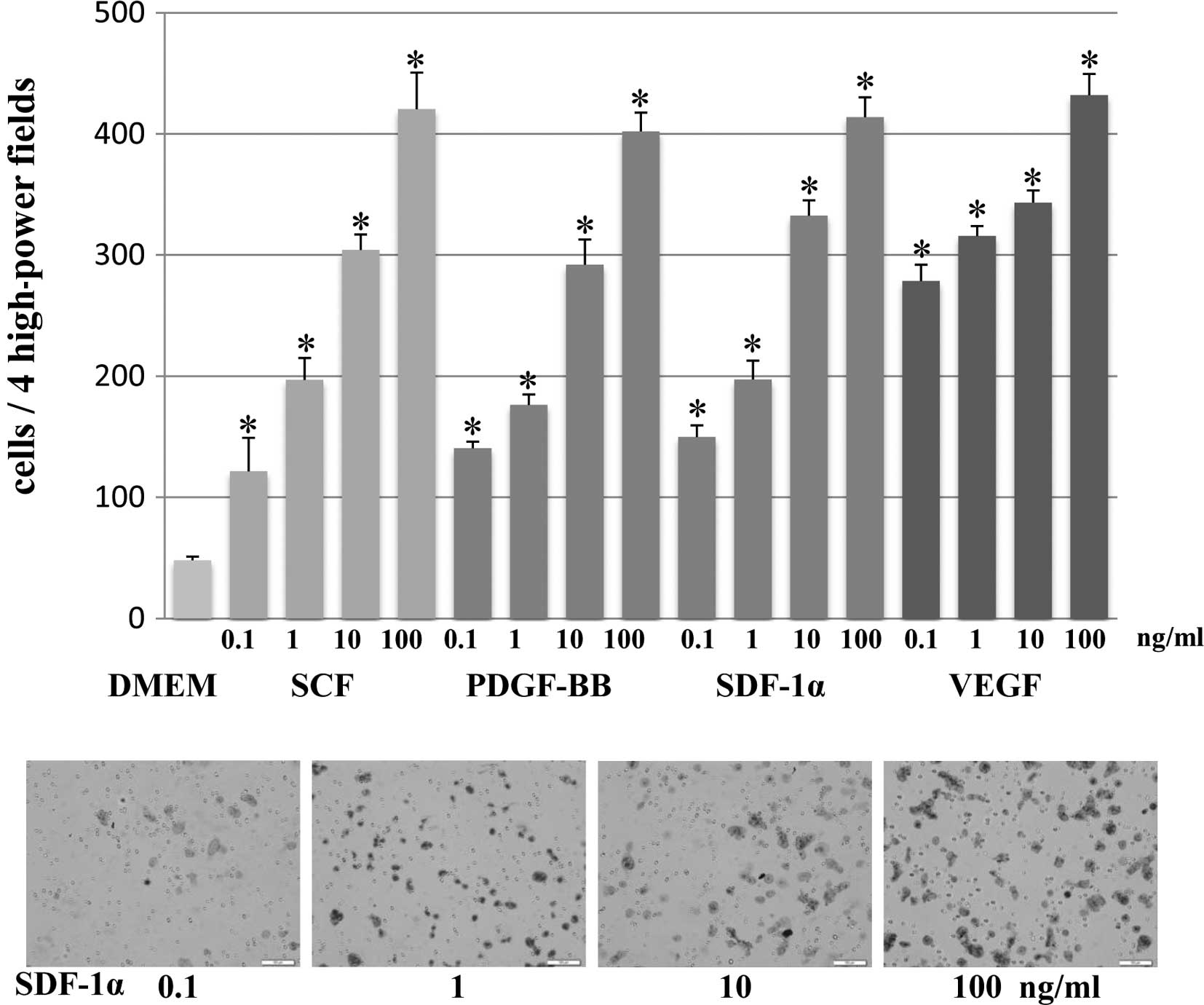
The migration of mouse iPS cells towards increasing
concentrations of specific growth factors, such as SCF, SDF-1α VEGF
and PDGF-BB (Fig. 2) was then
assessed. Specifically, 0.1–100 ng/ml of specific growth factors
were placed in the lower chambers. Migration was assayed after 24 h
by counting the number of mouse iPS cells in 4HPF on the membrane.
The migration of mouse iPS cells increased significantly with the
stimulation of each specific growth factor (SCF, SDF-1α VEGF and
PDGF-BB) at concentrations of 0.1, 1, 10 and 100 ng/ml compared to
the unconditioned medium without FBS (p<0.001). Furthermore, the
number of migrating mouse iPS cells increased dose-dependently with
concentrations of each specific growth factor from 0.1 to 100
ng/ml.
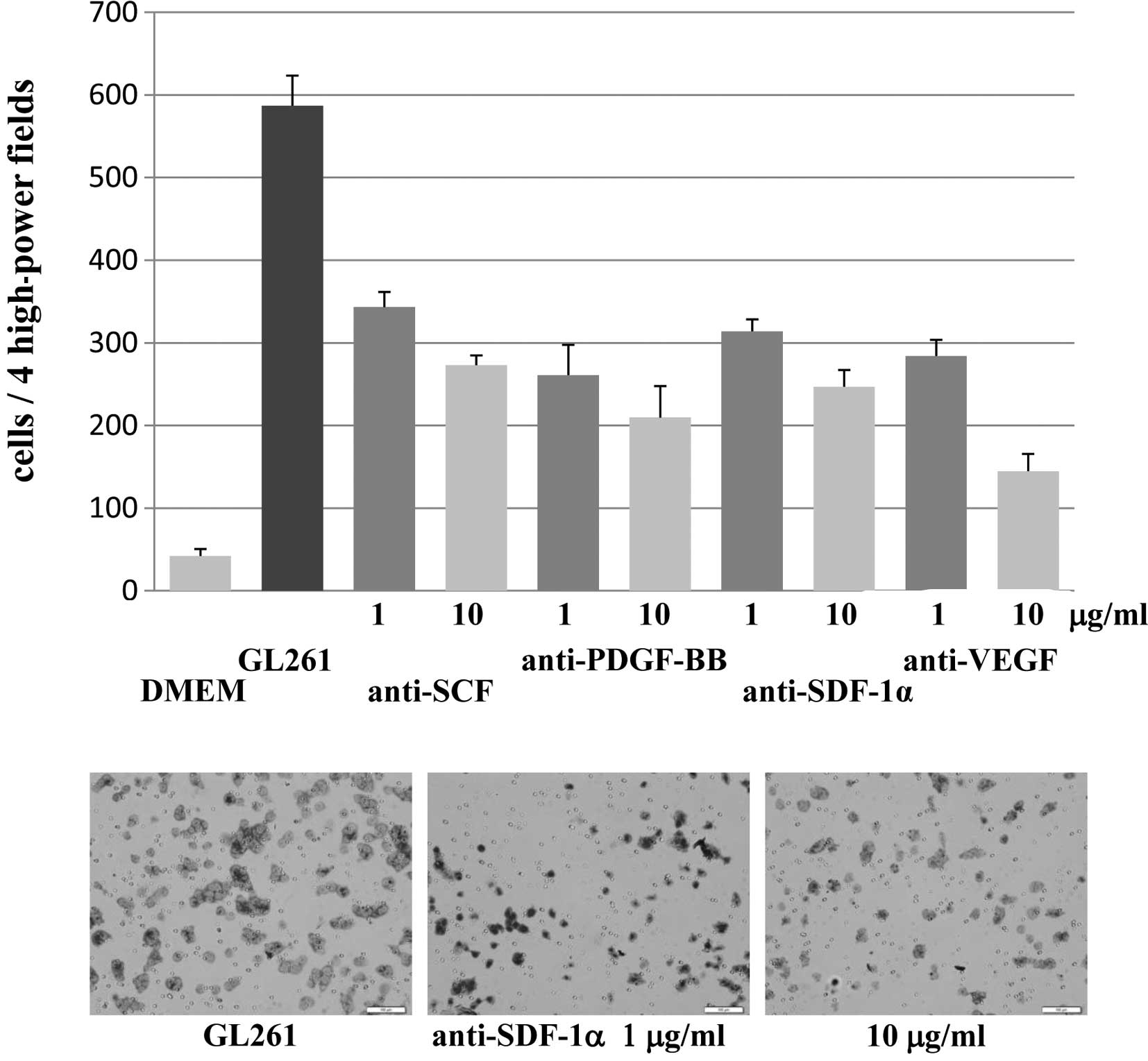
To investigate whether the increase in the migration
of mouse iPS cells towards CM prepared from glioma cell lines was
specifically attributable to the presence of specific growth
factors, migration assays were performed using CM from the GL261
mouse glioma cell line treated with increasing concentrations of
the inhibitory monoclonal anti-SCF, SDF-1α, VEGF and PDGF-BB
antibodies that neutralized the activity of SCF, SDF-1α, VEGF and
PDGF-BB, respectively. The high level of the migration of mouse iPS
cells that resulted following exposure to native CM from the GL261
mouse glioma cell line was significantly attenuated by treatment
with the inhibitory monoclonal anti-SCF, anti-SDF-1α, anti-VEGF and
anti-PDGF-BB antibodies (Fig. 3).
The application of the antibodies without any CM did not show any
effect on mouse iPS cell migration (data not shown). The inhibition
was dose-dependent, with 10 μg/ml of antibodies resulting in more
effective inhibition of mouse iPS cell migration compared to 1
μg/ml of antibodies. Anti-SCF, anti-SDF-1α, anti-VEGF and
anti-PDGF-BB antibodies (10 μg/ml) blocked the effects of CM by
46.5, 42.1, 24.6 and 35.7%, respectively. On the other hand, 1
μg/ml of anti-SCF, anti-SDF-1α, anti-VEGF and anti-PDGF-BB
antibodies blocked the effects of CM by 58.5, 53.5, 48.4 and 44.5%,
respectively. Furthermore, the combination of all the antibodies
showed a stronger attenuating effect of mouse iPS cell migration,
with 10 μg/ml blocked by 18.2% and 1 μg/ml by 32.2%. Taken
together, these results indicate that tumor-derived specific growth
factors (SCF, SDF-1α VEGF and PDGF-BB) promote the migration of
mouse iPS cells towards gliomas in vitro.
Expression of the receptors for growth
factors
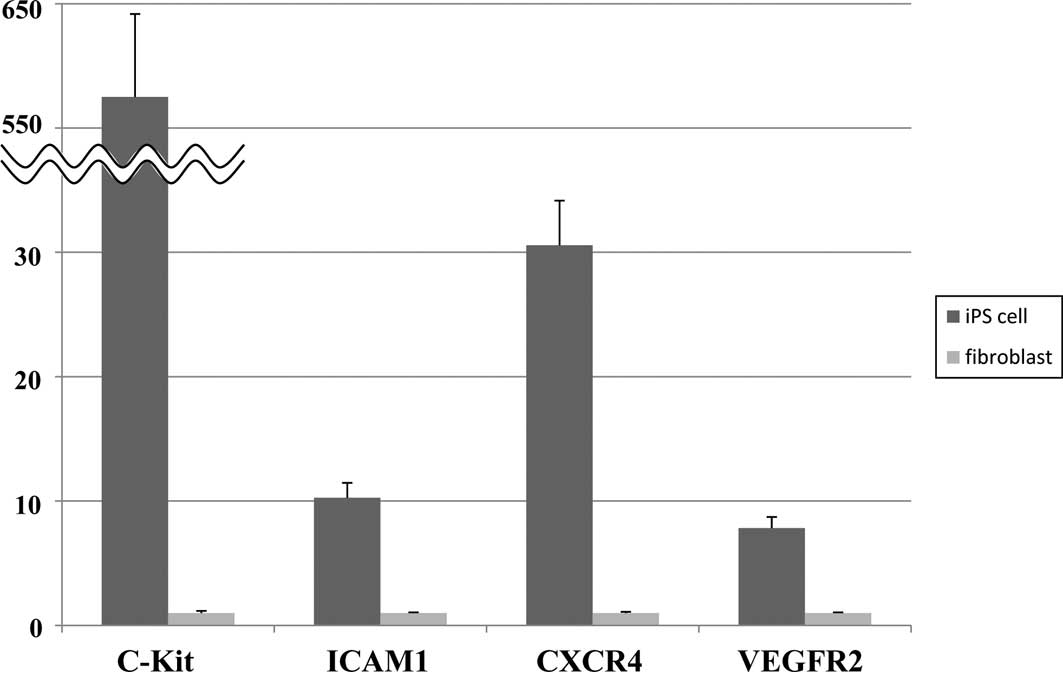
The expression of four different growth factor
receptors, c-Kit, CXCR4, VEGFR2 and ICAM-1, was analyzed in mouse
iPS cells using RT-PCR (Fig. 4). As
a positive control, mouse fibroblasts were analyzed in parallel.
All of the growth factor receptors were found to be expressed by
the mouse iPS cells. When the values were normalized to β-actin
expresssion, c-Kit, CXCR4, VEGFR2 and ICAM-1 mRNA expression in
mouse iPS cells was significantly up-regulated compared to the
mouse fibroblasts (p<0.001).
Discussion
Following the establishment of mouse iPS cells
generated from mouse skin fibroblasts by the retroviral
introduction of four transcription factors (Oct3/4, Sox2, c-Myc and
Klf4) (23), various cell
transplantation studies were performed due to the high reproductive
and pluripotent ability of iPS cells (26–29).
For iPS cells to function appropriately, the migratory activity of
iPS cells to the appropriate regions is crucial. Although numerous
studies have shown the in vitro and in vivo
tumor-tropic migratory ability of NSCs and MSCs to malignant
gliomas (6,7,9,11,12,15,30,31),
studies of migratory activity of iPS cells have yet to be
performed.
This study aimed to examine the migratory capacity
of mouse iPS cells towards gliomas in order to evaluate the
usefulness of iPS cells as vehicles for glioma gene therapies. The
migration of mouse iPS cells was significantly stimulated by CM
from six rodent and human glioma cell lines as well as four
specific growth factors that are secreted by gliomas (SCF, PDGF-BB,
SDF-1α and VEGF) (19–22). Furthermore, the expression of the
corresponding receptors (c-Kit, ICAM-1, CXCR4 and VEGFR2) was also
significantly up-regulated in the mouse iPS cells. These findings
indicated that soluble factors secreted by malignant glioma cells,
including the four growth factors examined, were potent inducers of
mouse iPS cell migration.
However, factors other than these four growth
factors that stimulate the migration of mouse iPS cells may be
produced by the glioma cells to various extents, depending on the
cell line. The heterogeneity of growth factor production presumably
expresses the in vivo differences in the biological behavior
of malignant gliomas, including the proliferative and invasive
natures associated with the expression profiles of cytokines,
interleukins and growth factors, such as transforming growth
factor-β1 (TGF-β1) (32–34) and matrix metalloproteinases
(35). Other specific growth
factors known to be expressed in malignant gliomas are fibroblast
growth factor-1 (FGF-1), PDGF-AA, insulin-like growth factor-1
(IGF-1), scatter factor/hepatocyte growth factor (SF/HGF) and
TGF-α, -β1 and -β2 (36,37). A number of these factors already
play a role in the stimulation of NSC migration (31).
The results of the present study showed that the
four specific growth factors (SCF, PDGF-BB, SDF-1α and VEGF) serve
as attractants for mouse iPS cells. Subsequently, blocking
experiments were performed by adding the inhibitory monoclonal
antibodies for those factors in the CM from GL261 mouse glioma
cells known to secrete numerous specific growth factors. Stimulated
mouse iPS cell migration by GL261 CM was significantly inhibited by
all the neutralizing antibodies examined, indicating that the
presence of these specific growth factors was significantly
responsible for the chemoattractant capacity of the CM.
Various types of stem cells are known to express the
receptors for SCF, PDGF-BB, SDF-1α and VEGF (c-Kit, ICAM-1,CXCR4
and VEGFR2, respectively) (38,39).
These receptors were highly expressed in the mouse iPS cells. The
presence of ligand/receptor combinations of the chemoattractive
factors, such as SCF/c-Kit, PDGF-BB/ICAM-1, SDF-1α/CXCR4 and
VEGF/VEGFR2, allow malignant glioma and iPS cells to communicate
with each other and, consequently, facilitate the migration of iPS
cells to gliomas.
The present study showed, for the first time, that
mouse iPS cells exerted marked tropism to glioma CM and at least
four specific growth factors (SCF, PDGF-BB, SDF-1α and VEGF). The
tropism was blocked by the neutralizing antibodies for these growth
factors. The majority of the malignant glioma cells are supposed to
secrete numerous soluble factors that attract mouse iPS cells,
although the amount is variable among the tumors. Additionally,
mouse iPS cells recognize a broad spectrum of signals from
malignant glioma cells as migration triggers. These observations
suggest that iPS cells are likely to aid as therapeutic vehicles
for the treatment of malignant gliomas if they are genetically
modified to express therapeutic transgenes that encode oncolytic
agents, apoptosis-inducing factors, interleukins, factors that
inhibit angiogenesis and the suicide genes.
We have investigated the use of NSCs and MSCs as
therapeutic vehicles for a suicide gene therapy, HSVtk/GCV, and
obtained encouraging results in pre-clinical models (14–18).
However, the use of this strategy for patients is hampered by
significant limitations, such as the isolation of clinically viable
and legally utilizable sources and ethical problems (20). Similarly, iPS cells remain in
pre-clinical phases and also experience ethical problems, including
cell tumorigenesis (40,41). If tumor formation of the iPS cells
is adequately regulated and all of the variables affecting safety
issues are rigorously evaluated, the clinical use of iPS cell-based
therapies may become a useful tool in the field of regeneration
therapy. The results of the present study strongly suggest that the
use of iPS cells as therapeutic vehicles for the delivery of
suicide genes is a novel strategy for the treatment of malignant
gliomas. Additional studies are required to compare the migration
characteristics of iPS cells to those of NSCs and MSCs,
particularly under in vivo conditions.
Acknowledgements
This study was supported in part by the Japan
Society for the Promotion of Science Young Investigators Grants
(S.K.).
References
|
1
|
Michotte A, Neyns B, Chaskis C, Sadones J
and In’t Veld P: Neuropathological and molecular aspects of
low-grade and high-grade gliomas. Acta Neurol Belg. 104:148–153.
2004.PubMed/NCBI
|
|
2
|
Louis DN, Ohgaki H, Wiestler OD, et al:
The 2007 WHO classification of tumours of the central nervous
system. Acta Neuropathol. 114:97–109. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Surawicz TS, Davis F, Freels S, Laws ER Jr
and Menck HR: Brain tumor survival: results from the National
Cancer Data Base. J Neurooncol. 40:151–160. 1998. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
DeAngelis LM: Brain tumors. N Engl J Med.
344:114–123. 2001. View Article : Google Scholar
|
|
5
|
Nakamizo A, Marini F, Amano T, et al:
Human bone marrow-derived mesenchymal stem cells in the treatment
of gliomas. Cancer Res. 65:3307–3318. 2005.PubMed/NCBI
|
|
6
|
Aboody KS, Brown A, Rainov NG, et al:
Neural stem cells display extensive tropism for pathology in adult
brain: evidence from intracranial gliomas. Proc Natl Acad Sci USA.
97:12846–12851. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Benedetti S, Pirola B, Pollo B, et al:
Gene therapy of experimental brain tumors using neural progenitor
cells. Nat Med. 6:447–450. 2000. View
Article : Google Scholar : PubMed/NCBI
|
|
8
|
Ehtesham M, Kabos P, Gutierrez MA, et al:
Induction of glioblastoma apoptosis using neural stem cell-mediated
delivery of tumor necrosis factor-related apoptosis-inducing
ligand. Cancer Res. 62:7170–7174. 2002.PubMed/NCBI
|
|
9
|
Ehtesham M, Kabos P, Kabosova A, Neuman T,
Black KL and Yu JS: The use of interleukin 12-secreting neural stem
cells for the treatment of intracranial glioma. Cancer Res.
62:5657–5663. 2002.PubMed/NCBI
|
|
10
|
Kim SK, Cargioli TG, Machluf M, et al:
PEX-producing human neural stem cells inhibit tumor growth in a
mouse glioma model. Clin Cancer Res. 11:5965–5970. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Kim SK, Kim SU, Park IH, et al: Human
neural stem cells target experimental intracranial medulloblastoma
and deliver a therapeutic gene leading to tumor regression. Clin
Cancer Res. 12:5550–5556. 2006. View Article : Google Scholar
|
|
12
|
Lee DH, Ahn Y, Kim SU, et al: Targeting
rat brainstem glioma using human neural stem cells and human
mesenchymal stem cells. Clin Cancer Res. 15:4925–4934. 2009.
View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Sasportas LS, Kasmieh R, Wakimoto H, et
al: Assessment of therapeutic efficacy and fate of engineered human
mesenchymal stem cells for cancer therapy. Proc Natl Acad Sci USA.
106:4822–4827. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Amano S, Li S, Gu C, et al: Use of
genetically engineered bone marrow-derived mesenchymal stem cells
for glioma gene therapy. Int J Oncol. 35:1265–1270. 2009.PubMed/NCBI
|
|
15
|
Li S, Gao Y, Tokuyama T, et al:
Genetically engineered neural stem cells migrate and suppress
glioma cell growth at distant intracranial sites. Cancer Lett.
251:220–227. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Li S, Tokuyama T, Yamamoto J, Koide M,
Yokota N and Namba H: Potent bystander effect in suicide gene
therapy using neural stem cells transduced with herpes simplex
virus thymidine kinase gene. Oncology. 69:503–508. 2005. View Article : Google Scholar
|
|
17
|
Li S, Tokuyama T, Yamamoto J, Koide M,
Yokota N and Namba H: Bystander effect-mediated gene therapy of
gliomas using genetically engineered neural stem cells. Cancer Gene
Ther. 12:600–607. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Namba H, Tagawa M, Iwadate Y, Kimura M,
Sueyoshi K and Sakiyama S: Bystander effect-mediated therapy of
experimental brain tumor by genetically engineered tumor cells. Hum
Gene Ther. 9:5–11. 1998. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Schichor C, Birnbaum T, Etminan N, et al:
Vascular endothelial growth factor A contributes to glioma-induced
migration of human marrow stromal cells (hMSC). Exp Neurol.
199:301–310. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Ehtesham M, Yuan X, Kabos P, et al: Glioma
tropic neural stem cells consist of astrocytic precursors and their
migratory capacity is mediated by CXCR4. Neoplasia. 6:287–293.
2004. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Serfozo P, Schlarman MS, Pierret C, Maria
BL and Kirk MD: Selective migration of neuralized embryonic stem
cells to stem cell factor and media conditioned by glioma cell
lines. Cancer Cell Int. 6:12006. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Hata N, Shinojima N, Gumin J, et al:
Platelet-derived growth factor BB mediates the tropism of human
mesenchymal stem cells for malignant gliomas. Neurosurgery.
66:144–157. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Okita K, Ichisaka T and Yamanaka S:
Generation of germline-competent induced pluripotent stem cells.
Nature. 448:313–317. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Takahashi K, Okita K, Nakagawa M and
Yamanaka S: Induction of pluripotent stem cells from fibroblast
cultures. Nat Protoc. 2:3081–3089. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Mohanam S, Sawaya R, McCutcheon I,
Ali-Osman F, Boyd D and Rao JS: Modulation of in vitro invasion of
human glioblastoma cells by urokinase-type plasminogen activator
receptor antibody. Cancer Res. 53:4143–4147. 1993.PubMed/NCBI
|
|
26
|
Amabile G and Meissner A: Induced
pluripotent stem cells: current progress and potential for
regenerative medicine. Trends Mol Med. 15:59–68. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Koch P, Kokaia Z, Lindvall O and Brustle
O: Emerging concepts in neural stem cell research: autologous
repair and cell-based disease modelling. Lancet Neurol. 8:819–829.
2009. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Ronaghi M, Erceg S, Moreno-Manzano V and
Stojkovic M: Challenges of stem cell therapy for spinal cord
injury: human embryonic stem cells, endogenous neural stem cells,
or induced pluripotent stem cells? Stem Cells. 28:93–99.
2010.PubMed/NCBI
|
|
29
|
Yu J and Thomson JA: Pluripotent stem cell
lines. Genes Dev. 22:1987–1997. 2008. View Article : Google Scholar
|
|
30
|
Cheng P, Gao ZQ, Liu YH and Xue YX:
Platelet-derived growth factor BB promotes the migration of bone
marrow-derived mesenchymal stem cells towards C6 glioma and
up-regulates the expression of intracellular adhesion molecule-1.
Neurosci Lett. 451:52–56. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Heese O, Disko A, Zirkel D, Westphal M and
Lamszus K: Neural stem cell migration toward gliomas in vitro.
Neuro Oncol. 7:476–484. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Brat DJ, Bellail AC and van Meir EG: The
role of interleukin-8 and its receptors in gliomagenesis and
tumoral angiogenesis. Neuro Oncol. 7:122–133. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
33
|
Mentlein R and Held-Feindt J:
Pleiotrophin, an angiogenic and mitogenic growth factor, is
expressed in human gliomas. J Neurochem. 83:747–753. 2002.
View Article : Google Scholar : PubMed/NCBI
|
|
34
|
Teicher BA: Malignant cells, directors of
the malignant process: role of transforming growth factor-beta.
Cancer Metastasis Rev. 20:133–143. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
35
|
Nagashima G, Suzuki R, Asai J and Fujimoto
T: Immunohistochemical analysis of reactive astrocytes around
glioblastoma: an immunohistochemical study of postmortem
glioblastoma cases. Clin Neurol Neurosurg. 104:125–131. 2002.
View Article : Google Scholar
|
|
36
|
Dunn IF, Heese O and Black PM: Growth
factors in glioma angiogenesis: FGFs, PDGF, EGF, and TGFs. J
Neurooncol. 50:121–137. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
37
|
Hamel W and Westphal M: Growth factors in
gliomas revisited. Acta Neurochir. 142:113–138. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
38
|
Das AV, James J, Zhao X, Rahnenfuhrer J
and Ahmad I: Identification of c-Kit receptor as a regulator of
adult neural stem cells in the mammalian eye: interactions with
Notch signaling. Dev Biol. 273:87–105. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
39
|
Tran PB, Ren D, Veldhouse TJ and Miller
RJ: Chemokine receptors are expressed widely by embryonic and adult
neural progenitor cells. J Neurosci Res. 76:20–34. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
40
|
Baudino TA, McKay C, Pendeville-Samain H,
et al: c-Myc is essential for vasculogenesis and angiogenesis
during development and tumor progression. Genes Dev. 16:2530–2543.
2002. View Article : Google Scholar : PubMed/NCBI
|
|
41
|
Miura K, Okada Y, Aoi T, et al: Variation
in the safety of induced pluripotent stem cell lines. Nat
Biotechnol. 27:743–745. 2009. View
Article : Google Scholar : PubMed/NCBI
|