Introduction
Tumours and cancers have become major public health
problems in Morocco, particularly due to a rapid epidemiological
transition. Cancer mortality remains high since diagnosis is
frequently delayed, and medical management is difficult and costly.
Health authorities in Morocco launched various campaigns to combat
cancer, since a large proportion of these diseases may be prevented
or detected early and properly treated. However, familial forms of
cancer only recently attracted interest, and some local genetic
centres have begun to provide oncogenetic services and offer
genetic testing for certain inherited forms of cancer with special
focus on breast cancer.
Hereditary breast and ovarian cancer syndrome is an
inherited cancer-susceptibility syndrome. This syndrome is
characterised by multiple family members with breast or ovarian
cancer or both, the presence of both breast and ovarian cancer in a
single individual, and early age of breast cancer onset (1). Germline mutations in BRCA1 and
BRCA2 genes account for a substantial proportion of families
with hereditary breast and ovarian cancer syndrome. Approximately
10% of cases of ovarian cancer and 3–5% of cases of breast cancer
are known to be associated with germline mutations in BRCA1
and BRCA2 (2–4). The two genes are tumour-suppressor
genes, and complete loss of their wild-type allele is a common
mechanism of gene inactivation in tumourigenesis (5). BRCA1 and BRCA2 are
involved in pathways that are crucial for DNA damage recognition,
double-strand break repair, checkpoint control, transcription
regulation and chromatin remodeling (6). Mutations in BRCA genes lead to
defects in DNA repair processes resulting in elevated genome
instability and a predisposition to breast and ovarian cancers.
BRCA1 and BRCA2 are large genes
containing 5,592 and 11,385 nucleotides spread over approximately
100,000 bases of genomic DNA each. More than 1,000 BRCA mutations
are reported in the Breast Cancer Information Core database
(7). In the general population, it
is estimated that approximately 1 in 300 to 1 in 800 individuals
carry a mutation in the BRCA1 or BRCA2 gene (8).
Hereditary breast and ovarian cancer syndrome is
characterised by four or more breast or ovarian cancers within a
family, typically occurring at young ages or bilaterally in the
case of breast cancer. Ovarian cancers are typically epithelial,
with a younger age of onset in BRCA1 carriers (mean 54
years), compared to sporadic ovarian cancers (mean 63 years), which
have a comparable age of onset to BRCA2 carriers (mean 62
years). Breast cancer in these families is also typically noted at
younger ages, particularly in BRCA1 carriers, compared to
that in the general population (9).
Clinical genetic testing for gene mutations allows
physicians to identify more precisely female individuals who are at
a substantial risk of developing breast and ovarian cancers. For
these individuals, screening and prevention strategies can be
instituted to reduce the risks (1).
The main objective of this study is to report the
first use of predictive genetic testing to detect a known familial
mutation in healthy Moroccan females with a high risk of developing
breast cancer and introduce supervision of these asymptomatic
female carriers as a new aspect in the combat against breast and
ovarian cancers in Morocco.
Patients and methods
Patients and their family members
Patients with breast cancer from unrelated families
were referred to our Medical Genetics Department for genetic
counseling. BRCA genetic testing was carried out in patients with
early age of onset at diagnosis, positive family history or
bilateral breast cancer. Table I
shows the clinical data for three index cases from 23 unrelated
families enrolled in the study. Genetic testing for presymptomatic
diagnosis was requested by 5 healthy female individuals among 45
female individuals with an elevated risk of breast cancer from the
three families in whom mutations of the BRCA1/2 genes were
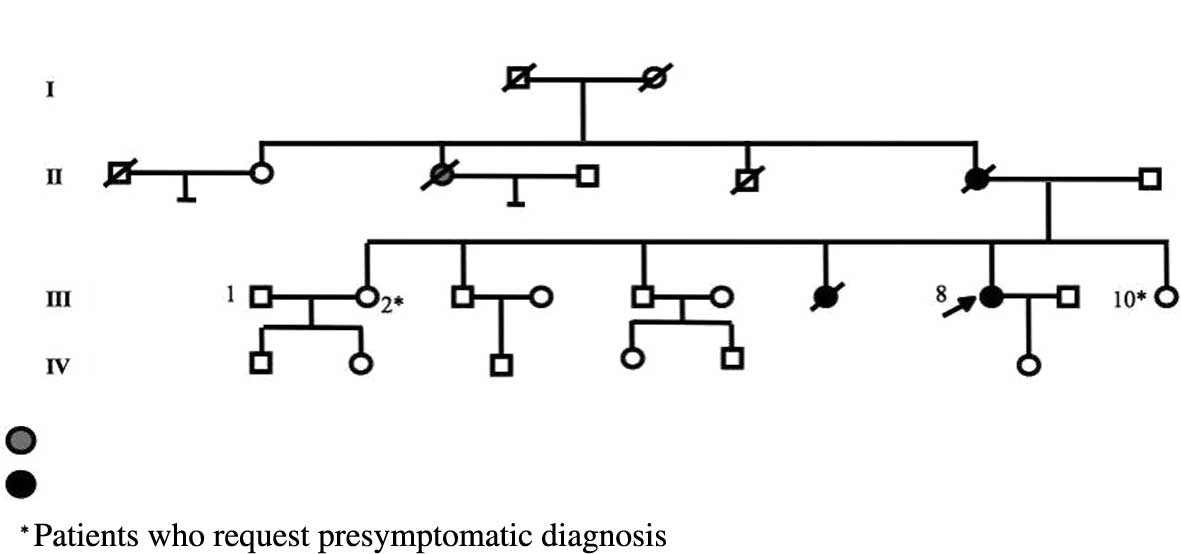
identified (Fig. 1). The study was
approved by our local ethics committee, and the subjects included
in the study gave written informed consent for DNA testing.
 | Table IClinical details of the three probands
in the three families. |
Table I
Clinical details of the three probands
in the three families.
| Proband III-8/family
1 | Proband III-18/family
2 | Proband III-17/family
3 |
|---|
| Age (years) | 37 | 48 | 55 |
| Bilateral breast
cancer | No | No | No |
| Left breast
cancer | No | Yes | No |
| First menstrual
period (years) | 13 | 13 | 14 |
| Tobacco, alcohol
use | None | None | |
| Menopause | No | No | Yes |
| Tumour size (cm) | 8 | 1 | 1.8 |
| Histological
diagnosis | Ductal carcinoma | Ductal carcinoma | Ductal carcinoma |
| Inflammatory breast
cancer | No | No | No |
| SBR | III | II | III |
| Progesterone
receptor | Positive | Positive | Positive |
| Oestrogen
receptor | Positive | Positive | Positive |
| TNM stage | T3N0M0 | T1N0M0 | T2N1M0 |
| Surgery | Radical
mastectomy
Axillary lymph node dissection |
Tumourectomy
Axillary lymph node dissection | Radical
mastectomy
Axillary lymph node dissection |
| Radiotherapy | Yes | Yes | Yes |
| Chemotherapy | FECa | CMFb | 3 FEC + taxotere |
| Clinical response (3
months) | Complete
response | Complete
response | Complete
response |
| Clinical response (6
months) | Complete
response | Liver metastasis | Complete
response |
Mutation screening
Genomic DNA was extracted from peripheral blood
lymphocytes using salt extraction methods and a complete analysis
of BRCA1/2 coding regions by bi-directional sequencing was
performed. When BRCA mutations were detected, they were confirmed
on a second patient DNA sample. The familial mutation was
identified by targeted direct sequencing of DNA from family members
who were at a high risk of developing breast or ovarian cancers
according to their pedigree data and who had requested this type of
genetic testing.
Results
BRCA1/2 mutation analysis
Two BRCA mutations were identified in the three
families. The 185delAG (c.68_69delAG) mutation in exon 2 of the
BRCA1 gene was found in two unrelated families and the
c.5073dupA; p.Trp1692MetfsX3 mutation in exon 11 of the
BRCA2 gene was detected in one family. The finding of these
mutations in the three families enabled us to conduct predictive
DNA testing for 5 female individuals who requested evaluation of
their genetic status with regards to their familial BRCA
mutation.
Two sisters from family 1 (III-2 and III-10;
Fig. 1A) were found to be carriers
of the BRCA1-185delAG mutation. Clinical and imaging surveillance
of the two sisters detected a breast tumour using magnetic
resonance imaging of the breast in the 48-year-old sister (III-2),
currently living abroad and followed by a foreign medical team.
Additionally, ovarian cancer was detected in her 42-year-old sister
(III-10) living in Morocco by transvaginal pelvic ultrasound with
colour Doppler. This patient underwent salpingo-oophorectomy, and
the histology revealed a papillary serous carcinoma, stage I,
T2N0M0. She was treated with six adjuvant cycles of chemotherapy
type taxol-carboplatin. A complete response was achieved.
In family 2, Patient IV-17 (Fig. 1B) was a carrier of the familial
mutation c.5073dupA/p.Trp1692MetfsX3 in exon 11 of the BRCA2
gene, confirmed by DNA testing. Her mother (III-20) was identified
as an obligate carrier. These two female patients are healthy with
no cancer history and are under surveillance according to standard
protocols (clinical breast examination semi-annually, annual
mammography and breast magnetic resonance imaging screening, and
annual transvaginal pelvic ultrasound with colour Doppler).
In family 3, genetic testing showed that the female
patient identified as IV-31, and her mother (III-13; Fig. 1C) were not carriers of the familial
BRCA1-185delAG mutation. The female individuals were informed that
their risk of developing breast cancer does not differ from females
of the same age in the general population.
Discussion
Germline mutations in either of the two predisposing
genes, BRCA1 and BRCA2, account for a significant
proportion of hereditary breast and ovarian cancers. Approximately
10% of cases of ovarian cancer and 3–5% of cases of breast cancer
are due to germline mutations in BRCA1 and BRCA2
(2). In the general population, it
is estimated that approximately 1 in 300 to 1 in 800 individuals
carry a mutation in BRCA1 or BRCA2 (3).
A large number of different mutations in the two
genes have been reported, some of which are founder mutations noted
in the ethnic groups of Ashkenazi Jews, Icelanders, the French and
other populations (10,11). Three founder mutations have been
identified in Ashkenazi Jews, BRCA1-185delAG, BRCA1-5382insC and
6174delT in the BRCA2 gene. The overall rate of the three
founder mutations is 2.6% (1/40) compared to the rate of 0.2%
(1/500) of mutation carriers in BRCA1/2 in the general
population (12,13). The three mutations of
BRCA1-185delAG, BRCA1-5382insC and BRCA2-6174delT were found in 1,
0.13 and 1.52% of the Ashkenazi Jews population, respectively
(12,13).
Among the North African population, the mutational
spectrum of BRCA1/2 has yet to be well characterised. Mutation
c.798_799delTT has been observed in two Algerian families, as well
as in two Tunisian families presenting with breast cancer,
indicating the first non-Jewish founder mutation to be described in
Northern Africa (14).
In the present study, the 185delAG mutation in exon
2 of the BRCA1 gene and the c.5073dupA mutation in exon 11
of the BRCA2 gene are the first mutations described in
Moroccan families with hereditary breast and ovarian cancer
syndrome. The 185delAG mutation in exon 2 of the BRCA1 gene
was detected in families 1 and 3, whereas the proband III-8 in
family 2 was a carrier of the c.5073dupA/p.Trp1692MetfsX3 mutation
in exon 11 of the BRCA2 gene. Genetic counseling was offered
to each of the families. Female individuals with either BRCA
mutation have a cumulative lifetime risk of invasive breast cancer
of 65–74% (15,16). For females with a BRCA1
mutation, the risk of ovarian cancer is 39–46%. This risk is lower
(12–20%) for women carrying BRCA2 mutations (15,16).
The 185delAG mutation reported for the first time in
females of two Moroccan families may be common in Morocco. Thus,
further investigations into this mutation should be conducted in a
larger cohort of patients. If the repeated occurrence of the
185delAG mutation is confirmed in the Moroccan population, this may
simplify genetic testing and have clinical and public health
implications.
The finding of the mutations in the three families
enabled us to conduct DNA testing in 5 female individuals to
determine whether they had inherited the familial BRCA mutation.
Once a mutation was identified in the proband III-8 in family 1,
the genetic status of two asymptomatic sisters was determined. The
two sisters were found to be carriers of the familial
BRCA1-185delAG mutation. Therefore, a medical follow-up of the two
sisters was implemented. Surveillance imaging detected breast
cancer by magnetic resonance imaging of the breast in a 48-year-old
female (Patient III-2; Fig. 1A),
and ovarian cancer was detected by transvaginal pelvic ultrasound
with colour Doppler in her 42-year-old sister (Patient III-10;
Fig. 1A); a complete response to
treatment was achieved. In family 2, patient IV-17 (Fig. 1B) was a carrier of the familial
mutation c.5073dupA/p.Trp1692MetfsX3 mutation of BRCA2.
Consequently, her mother was identified as an obligate carrier. The
two patients are healthy thus far, with no history of cancer, and
are under supervision in accordance with standard protocols. This
BRCA2 mutation confers an increased risk of developing breast or
ovarian cancers depending on age and the penetrance of the
mutation.
In family 3, genetic testing identified that patient
IV-31 (Fig. 1C) and her mother were
not carriers of the familial BRCA1 mutation. Consequenlty,
it was determined that the risk of developing sporadic breast
cancer is at a rate roughly equivalent to that of the general
population. These female patients may have undergone unnecessary
intervention, including prophylactic surgery. Thus, the
availability of the BRCA analysis has beneficial impact on the care
and counseling of female individuals at risk. Once a mutation is
identified in an affected person, asymptomatic family members can
subsequently be tested for this mutation, since first-degree
relatives of patients with breast cancer have increased risk for
early onset of this disease (17).
Female individuals who remain untested for the gene mutation, but
have a first-degree relative with a BRCA mutation, have a 36–85%
lifetime risk of developing breast cancer, indicating a need for
accurate, life-long surveillance. The American Cancer Society and
the National Comprehensive Cancer Network recommend that magnetic
resonance imaging be used in addition to, and not instead of
mammography, this surveillance (18).
Genetic testing can be extremely valuable in the
clinical process and for personal decision-making for high-risk
families. The identification of a carrier of a BRCA mutation in a
family is useful in the clinical management of the affected
patient, but also provides appropriate recommendations for other
members of the family. The identification of a family that is
highly susceptible to hereditary cancer syndrome is the key to
management of these families.
In conclusion, we report our initial experience in
the management and presymptomatic diagnosis of breast cancer in
three Moroccan families with hereditary breast and ovarian cancer
syndrome and known BRCA1/2 gene mutations. Efforts are
underway to reduce the high incidence and mortality associated with
breast cancer on a global scale. Morocco, which has 30,000 new
cases of cancer every year, has launched an ambitious national
program of prevention and monitoring of cancer in the population
for the decade 2010–2019. This program is based on the early
detection of female individuals at high risk and should also
integrate molecular testing and management of females with an
increased familial risk of breast and ovarian cancers, since
genetic predisposition is the strongest risk factor. Early
detection is of high priority in the medical management of this
diseasein order for recommendations to be made for public health
action on molecular genetic testing and genetic counseling.
Acknowledgements
The authors extend their sincere thanks to all of
the staff of the Department of Medical Genetics of the National
Institute of Health for their continuous support. We are
particularly thankful to Dr Rachid Tazi Ahnini for the
indispensable editorial assistance.
References
|
1
|
ACOG Committee on Practice Bulletins.
Hereditary breast and ovarian cancer syndrome. Gynecol Oncol.
113:6–11. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Robson ME, Boyd J, Borgen PI and Cody HS
III: Hereditary breast cancer. Curr Probl Surg. 38:387–480. 2001.
View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Risch HA, McLaughlin JR, Cole DE, et al:
Population BRCA1 and BRCA2 mutation frequencies and cancer
penetrances: a kin-cohort study in Ontario, Canada. J Natl Cancer
Inst. 98:1694–1706. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Rubin SC, Blackwood MA, Bandera C, et al:
BRCA1, BRCA2, and hereditary nonpolyposis colorectal cancer gene
mutations in an unselected ovarian cancer population: relationship
to family history and implications for genetic testing. Am J Obstet
Gynecol. 178:670–677. 1998. View Article : Google Scholar
|
|
5
|
Ratajska M, Brozek I, Senkus-Konefka E,
Jassem J, Stepnowska M, Palomba G, Pisano M, Casula M, Palmieri G,
Borg A and Limon J: BRCA1 and BRCA2 point mutations and large
rearrangements in breast and ovarian cancer families in Northern
Poland. Oncol Rep. 19:263–268. 2008.PubMed/NCBI
|
|
6
|
Mohamad HB: Counseling for male BRCA
mutation carriers: a review. Apffelstaedt JP Breast. 17:441–450.
2008.PubMed/NCBI
|
|
7
|
Filippini S, Blanco A, Fernández-Marmiesse
A, Alvarez-Iglesias V, Ruíz-Ponte C, Carracedo A and Vega A:
Multiplex SNaPshot for detection of BRCA1/2 common mutations in
Spanish and Spanish related breast/ovarian cancer families. BMC Med
Genet. 29:402007. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Whittemore AS, Gong G and Itnyre J:
Prevalence and contribution of BRCA1 mutations in breast cancer and
ovarian cancer: results from three U.S. population-based
casecontrol studies of ovarian cancer. Am J Hum Genet. 60:496–504.
1997.PubMed/NCBI
|
|
9
|
Hanson H and Hodgson S: Cancer genetics
and reproduction, best practice and research. Clin Obstet Gynaecol.
24:3–18. 2010.
|
|
10
|
Neuhausen SL: Ethnic differences in cancer
risk resulting from genetic variation. Cancer. 86:2575–2582. 1999.
View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Ferla R, Calo V, Cascio S, Rinaldi G,
Badalamenti G, Carreca I, Surmacz E, Colucci G, Bazan V and Russo
A: Founder mutations in BRCA1 and BRCA2 genes. Ann Oncol. 18:93–98.
2007. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Roa BB, Boyd AA, Volcik K, et al:
Ashkenazi Jewish population frequencies for common mutations in
BRCA1 and BRCA2. Nat Genet. 14:185–187. 1996. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Neuhausen S, Gilewski T, Norton L, et al:
Recurrent BRCA2 6174delT mutations in Ashkenazi Jewish women
affected by breast cancer. Nat Genet. 13:126–128. 1996. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Uhrhammer N, Abdelouahab A, Lafarge L,
Feillel V, Ben Dib A and Bignon YJ: BRCA1 mutations in Algerian
breast cancer patients: high frequency in young, sporadic cases.
Int J Med Sci. 5:197–202. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Antoniou A, Pharoah PD, Narod S, et al:
Average risks of breast and ovarian cancer associated with BRCA1 or
BRCA2 mutations detected in case series unselected for family
history: a combined analysis of 22 studies. Am J Hum Genet.
72:1117–1130. 2003. View
Article : Google Scholar : PubMed/NCBI
|
|
16
|
King MC, Marks JH and Mandell JB: Breast
and ovarian cancer risks due to inherited mutations in BRCA1 and
BRCA2. New York Breast Cancer Study Group. Science. 302:643–646.
2003. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Loman N, Bladstrom A, Johannsson O, Borg A
and Osson H: Cancer incidence in relatives of a population-based
set of cases of early-onset breast cancer with a known BRCA1 and
BRCA2 mutation status. Breast Cancer Res. 5:175–186. 2003.
View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Waters CM, Hoover AC, McClain LC, Moore
TT, Rogers CT and Thornton K: Current guidelines and best practice
evidence for intensified/enhanced breast cancer screening in women
with BRCA mutations. J Nurs Pract. 5:447–453. 2009. View Article : Google Scholar
|