Case report
Extranodal marginal zone B-cell lymphoma (EMZL) of
mucosa-associated lymphoid tissue lymphoma arises from the marginal
zone of mucosa-associated lymphoid tissue. EMZL is common among
ocular adnexal malignant tumors; however, orbital lymphomas
involving striated muscles are rare. This report examines an
unusual case of orbital EMZL involving the superior rectus
muscle.
A 66-year-old female suffering from proptosis of the
left eye (OS) and double vision for 1 month was referred to our
hospital due to an abnormality of the superior rectus muscle OS.
Visual acuity was found to be 20/20 in both eyes with a normal
intraocular pressure. Extraocular examination demonstrated upper
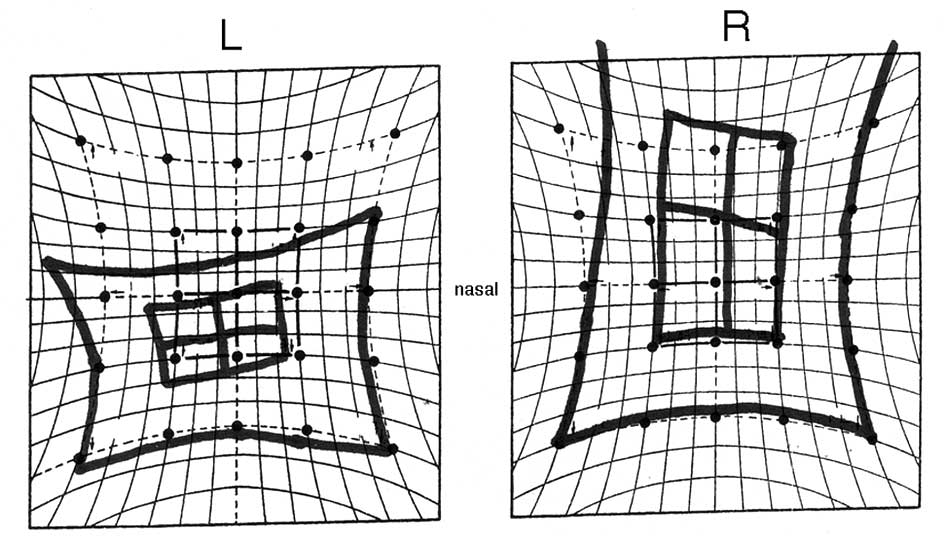
eyelid swelling without ocular pain. The fundus was normal. Hess
screen analysis revealed supraduction OS (Fig. 1). The laboratory values, including a
blood cell count, biochemistry, and thyroid hormones, were found to
be normal. No systemic abnormality was detected with the exception
of the orbit. Initial magnetic resonance imaging (MRI) of the orbit
revealed an indistinct mass in the superior orbit close to, or
within, the superior rectus muscle (Fig. 2). Differential diagnoses of the mass
lesion in the extraocular muscle were orbital tumor, Graves’
disease, and orbital myositis. Biopsy of the orbital mass was
performed.
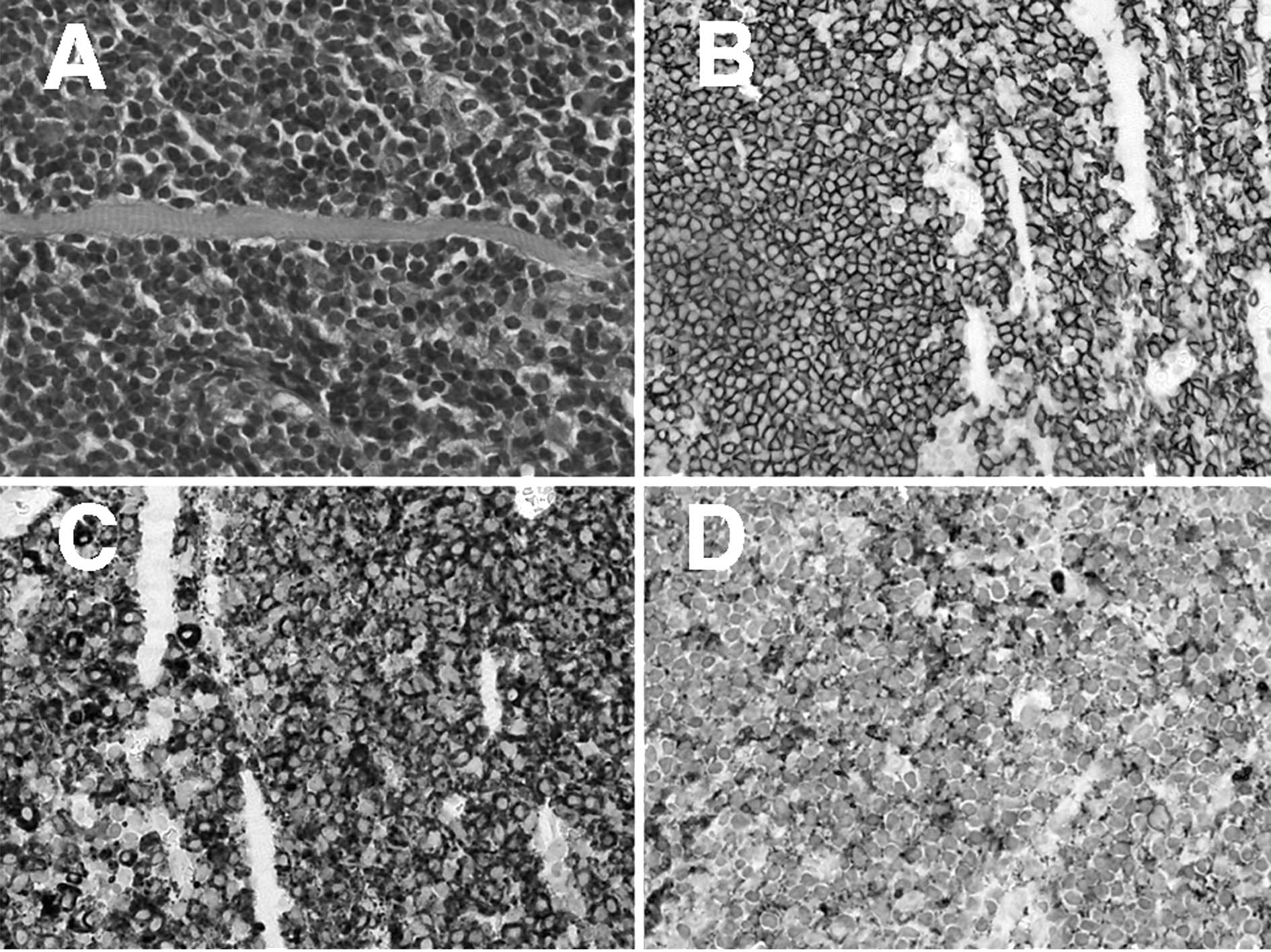
A histological examination showed diffuse atypical
lymphoid cell infiltration, mixed with plasma cells with Russell
bodies. Lymphoid cells were present within fragmented striated
muscles (Fig. 3A).
Immunohistochemically, the atypical lymphoid cells were positive
for CD20 and CD79a, markers for B-cells (Fig. 3B and C), and negative for CD3 and
CD5, markers for T-cells. The immunohistochemical examination of
immunoglobulin showed deviation to κ chains in the infiltrating
lymphoid cells (Fig. 3D).
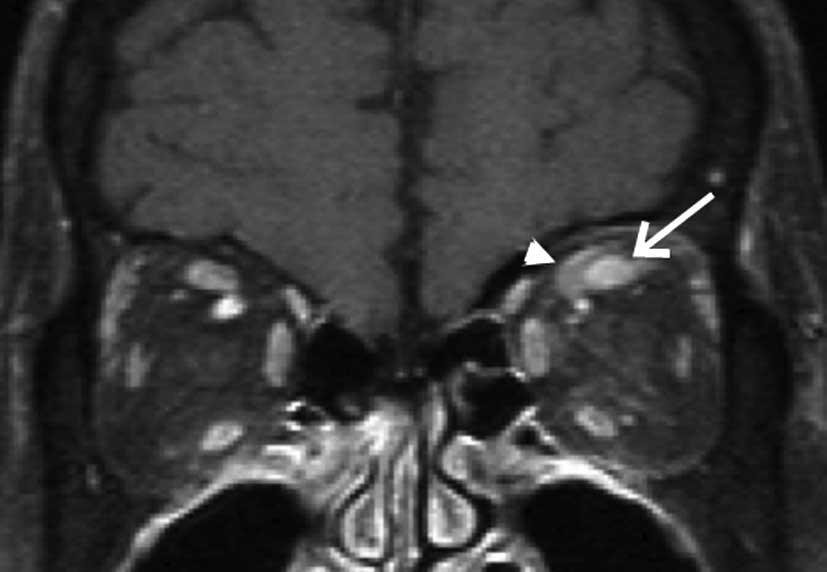
The orbital tumor was diagnosed as EMZL involving
the superior rectus muscle. Radiotherapy with a total dosage of 30
Gy was administered. The radiotherapy reduced the volume of the
tumor (Fig. 4, red arrow), and the
superior rectus muscle was clearly identified (Fig. 4, white arrow). The supraduction
limitation in OS movement remained unchanged, although tumor
recurrence was not observed one and a half years after
radiotherapy.
Discussion
Since the border between the tumor and superior
rectus muscle was not differentiated in the initial MRI of the
orbit, the origin of the tumor remains to be determined.
Histological examination showed atypical lymphoid cell infiltration
within the fragmented striated muscle. Muscle fibers in the
remaining striated muscle were clearly noted in the specimen,
indicating that the muscle was not degenerative. Following
radiotherapy, superior rectus muscle with a reduced tumor was
visualized. Therefore, the clinicopathological findings indicate
that EMZL did not arise in the extraocular muscle, but arose in the
orbital soft tissue adjacent to the muscle, followed by invasion to
the superior rectus muscle.
In this case, only superior muscle was involved in
tumor cell invasion, presenting with supraduction limitation, but
not inferior adduction limitation. These results suggest that
supraduction limitation occurred due to muscular contraction
disorder of the superior rectus and not due to restriction by an
enlarged antagonist muscle as observed in Graves’ disease. Together
with the histological findings, it was noted that the extraocular
muscle contraction disorder is caused by direct lymphoma cell
invasion. Despite resolution of the tumor after irradiation,
supraduction limitation was not improved, suggesting that
irradiation led not only to tumor cell death, but also subsequent
irreversible muscle fibrosis.
It was previously reported that the most common site
of ocular EMZL was the conjunctiva (51%), while extraocular muscles
were the most rare localization (only 5%) (1). A review the literature revealed only 9
cases of orbital lymphoma invading the superior rectus muscle, in
which, histologically, EMZL was not included (2–5)
(Table I). In contrast, 7 cases of
extraocular muscle involvement in EMZL have been reported, but no
case exists involving the superior rectus muscle and ocular
movement disorder with the exception of this case (6–8)
(Table II). Two cases of diffuse
large B-cell lymphoma and peripheral T-cell lymphoma exhibited the
mild limitation of eye movement following treatment (Table I). Irreversible eye movement
disorder involving EMZL following either chemo- or radiotherapy has
not been reported as in this case. Therefore, EMZL arising in the
orbit shows extraocular muscle involvement and leads to impairment
of the visual function.
 | Table IClinicopathological characteristics in
orbital lymphomas involving the superior rectus muscle in the
literature. |
Table I
Clinicopathological characteristics in
orbital lymphomas involving the superior rectus muscle in the
literature.
| Case | Gender | Age (years) | Eye | Orbital site
involved | Histology | Extraorbital
involvement | Therapy | Eye movement disorder
after therapy | Refs. |
|---|
| 1 | F | 62 | R | Superior
rectus-levator muscle complex | Diffuse large B-cell
lymphoma | No | C | Mildly limited | 2 |
| 2 | M | 82 | L | Superior and medial
rectus muscle | Diffuse large B-cell
lymphoma | Yes (stage III) | C and R | Improved | 3 |
| 3 | M | 44 | Bilateral | All extraocular
muscles | Peripheral T-cell
lymphoma | Yes (stage III) | C | Mildly limited | 4 |
| 4 | M | 40 | R | Superior
rectus-levator muscle complex | Follicular
lymphoma | No | R | Improved | 5 |
| 5 | M | 57 | R | Superior
rectus-levator muscle complex | Diffuse T-cell
lymphoma | No | R | Improved | 5 |
| 6 | F | 61 | R | Superior
rectus-levator muscle complex | Poorly differentiated
lymphocytic lymphoma | Yes | R | Improved | 5 |
| 7 | M | 60 | R | Superior rectus
muscle | Lymphoplasmacytoid
lymphoma | No | R | Improved | 5 |
| 8 | F | 62 | R | Superior rectus
muscle | Mature T-cell
lymphoma | No | R | Improved | 5 |
| 9 | F | 67 | L | Superior rectus
muscle | Diffuse mature
lymphoma | No | R | Improved | 5 |
| 10 | F | 66 | L | Superior rectus
muscle | Extranodal marginal
zone B-cell lymphoma | No | R | Not improved | Present case |
 | Table IIClinicopathological characteristics
with extraocular muscle involvement in extranodal marginal zone
B-cell lymphoma of the orbit. |
Table II
Clinicopathological characteristics
with extraocular muscle involvement in extranodal marginal zone
B-cell lymphoma of the orbit.
| Case | Gender | Age (years) | Eye | Orbital site
involved | Extraorbital
involvement | Therapy | Eye movement disorder
after therapy | Refs. |
|---|
| 1 | F | 54 | R | Inferior oblique
muscle | No | R | - | 6 |
| 2 | M | 52 | L | Inferior rectus
muscle | No | Rituximab | - | 7 |
| 3 | F | 57 | R | Inferior rectus
muscle | No | R | - | 8 |
| 4 | M | 75 | R | Medial rectus
muscle | Yes (stage IV) | C | - | 8 |
| 5 | M | 80 | L | Lateral rectus
muscle | No | Chlorambucil | - | 8 |
| 6 | F | 54 | R | Inferior oblique
muscle | No | R | - | 8 |
| 7 | M | 34 | R | Levator muscle | No | R | - | 8 |
| 8 | F | 66 | L | Superior rectus
muscle | No | R | Not improved | Present case |
References
|
1
|
Lee JL, Kim MK, Lee KH, et al: Extranodal
marginal zone B-cell lymphomas of mucosa-associated lymphoid
tissue-type of the orbit and ocular adnexa. Ann Hematol. 84:13–18.
2005. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Hsu MW, Chung CH, Chang CH, Hu PS and Hsu
SL: Ptosis as an initial manifestation of orbital lymphoma: a case
report. Kaohsiung J Med Sci. 22:194–198. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Payne J, Shields C, Eagle RJ and Shields
J: Orbital lymphoma simulating thyroid orbitopathy. Ophthal Plast
Reconstr Surg. 22:302–304. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Janatpour K, Choo P and Lloyd WC III:
Primary orbital peripheral T-cell lymphoma: histologic,
immunophenotypic, and genotypic features. Arch Ophthalmol.
125:1289–1292. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Hornblass A, Jakobiec F, Reifler D and
Mines J: Orbital lymphoid tumors located predominantly within
extraocular muscles. Ophthalmology. 94:688–697. 1987. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Curutchet L, Gicquel J, Adenis J and
Dighiero P: Lymphoma revealed by isolated obliquus inferior muscle
involvement in exophthalmia. J Fr Ophtalmol (In French).
26:626–630. 2003.PubMed/NCBI
|
|
7
|
Benetatos L, Alymara V, Asproudis I and
Bourantas KL: Rituximab as first line treatment for MALT lymphoma
of extraocular muscles. Ann Hematol. 85:625–626. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Izambart C, Robert P-Y, Petellat F, et al:
Extraocular muscle involvement in marginal zone B-cell lymphomas of
the Orbit. Orbit. 27:345–349. 2008. View Article : Google Scholar : PubMed/NCBI
|