Introduction
Ulcerative colitis (UC) is a chronic inflammatory
bowel disease with an increased risk of developing into colorectal
cancer (CRC). The meta-analysis by Eaden et al reported that
the cumulative risk probability of ulcerative colitis-associated
CRC (UC-CRC) was 1.6% after 10 years, 8.3% after 20 years, and
18.4% after 30 years of disease duration (1). Risk factors for UC-CRC have been shown
to be greater with the extent and duration of disease, increased
severity of bowel inflammation, coexisting primary sclerosing
cholangitis, young age at onset of UC and family history of
sporadic CRC (2).
Typically, UC patients with a higher risk of UC-CRC
undergo periodic colonoscopic surveillance with multiple biopsies
for the early diagnosis and treatment of dysplasia or cancer
lesions. However, such a surveillance program has a number of
limitations, including its efficacy, high cost, invasiveness,
incomplete patient enrollment, sampling variations and poor
agreement in histopathological interpretation (3). A number of molecular markers
predictive for UC-CRC have been reported (4–6), but
remain unavailable in the practical management of UC patients.
Chronic inflammation in UC is considered to cause
colonic epithelial injury, repair and regeneration, or the
development of UC-CRC (7). Stem
cell (SC) research and the cancer stem cell (CSC) hypothesis have
shown that colonic SCs or CSCs are involved in tissue regeneration
and colonic carcinogenesis (8–10).
CSCs may greatly contribute to inflammation-associated
carcinogenesis in UC.
The transcription factors OCT4 and NANOG play
significant roles in maintaining pluripotency and self-renewal of
embryonic stem cells as well as in adult stem cells (11). OCT4 is a nuclear protein belonging
to a family of transcription factors containing the POU DNA-binding
domain (12). NANOG is a homeobox
transcription factor that contains DNA-binding domains involved in
the regulation of key eukaryotic developmental processes (13). CD133 is a cell surface glycoprotein
with five transmembrane domains. CD133 is currently regarded as one
of the most significant markers of colon CSCs (14).
Subsequently, we investigated the expression of stem
cell markers in UC-CRC and inflamed colonic epithelium as compared
to sporadic CRC. To evaluate the expression levels of each molecule
in colonic epithelial cells, microdissection techniques were used
for the reduction of the contamination of stromal cells as much as
possible.
In the present study, expression levels of
PROM, POU5F1 and NANOG mRNAs were investigated
in UC-CRC, inflamed colonic epithelium, sporadic CRC and adjacent
colonic epithelium. Furthermore, the associations between disease
characteristics and stem cell marker expression were also examined
to evaluate their predictive value for the development of
UC-CRC.
Materials and methods
Patients with UC and UC-CRC
A total of 24 UC patients and 6 patients with UC-CRC
were included in the current analyses. All patients were treated at
the Department of Gastrointestinal and Pediatric Surgery in the Mie
University Graduate School of Medicine, Japan.
The UC diagnosis was based on the medical history,
endoscopic findings, histological examination, laboratory tests and
clinical disease presentation. The extent of disease was defined as
proctitis, left-sided and extensive colitis. The severity of
disease was classified as ‘mild’, ‘moderate’ and ‘severe’ based on
clinical, endoscopic and histopathological findings as discussed
above.
Patients with sporadic colorectal
cancer
A total of 37 patients with sporadic CRC were also
included in this study to compare the expression of stem cell
markers between UC-CRC and sporadic CRC.
Sample selection criteria
For inclusion in the study, selection criteria
required the availability of samples accompanying complete clinical
data and the quality of isolated RNA for real-time PCR based on the
expression of the β-actin (ACTB) gene as an internal
control.
Microdissection of formalin-fixed,
paraffin-embedded (FFPE) specimens
To purify colonic epithelial cells or cancer cells,
a microdissection technique was used. Surgically resected specimens
were fixed in 10% formaldehyde solution v/v and embedded in
paraffin. Sections (10 μm) of FFPE specimens were stained with
nuclear fast red. Manual microdissection using a scalpel was
performed to collect only inflamed and non-inflamed colonic
epithelial or cancer cells, excluding stromal cells as much as
possible. Sample collection by microdissection typically ensured
>70% of target cells for each sample.
RNA extraction from FFPE specimens
Microdissected samples were digested with proteinase
K in lysis buffer containing Tris-HCl, EDTA and sodium dodecyl
sulfate as previously reported with minor modifications (15). RNA was purified by phenol and
chloroform extraction.
cDNA synthesis
cDNA was synthesized with random hexamer primers and
Superscript III reverse transcriptase (Invitrogen, Carlsbad, CA,
USA) according to the manufacturer’s instructions.
Real-time quantitative RT-PCR
Real-time quantitative RT-PCR analysis was performed
with the SYBR-Green PCR master mix using an Applied Biosystems 7500
real-time PCR system according to the manufacturer’s instructions
(Applied Biosystems, Inc., Foster City, CA, USA). Primers and
probes for PROM (CD133), POU5F1 (OCT4), NANOG
and ACTB (β-actin) were designed with primer3 software
(Biology Workbench Version 3.2, San Diego Supercomputer Center,
University of California, San Diego, CA, USA). Primer sequences
were as follows: PROM-specific: sense, GCT TTGCAATCTCCCTGTTG
and antisense, TTGATCCGG GTTCTTACCTG; POU5F1-specific:
sense, CTGGAGAAGG AGAAGCTGGA and antisense, CAAATTGCTCGAGTTCT
TTCTG; NANOG-specific: sense, GAGATGCCTCACACG GAGAC and
antisense, CTTTGGGACTGGTGGAAGAA and ACTB-specific: sense,
ACAGAGCCTCGCCTTTGC and antisense, GCGGCGATATCATCATCC. PCR was
performed in a final volume of 25 μl with a SYBR-Green PCR master
mix using 1 μl cDNA and 400 nM of each primer for the respective
genes. Cycling conditions were 50°C for 2 min and 95°C for 10 min
followed by 40 cycles at 95°C for 15 sec and 60°C for 1 min.
Relative mRNA levels of target genes
Relative mRNA levels were determined by the standard
curve method. The standard curves and line equations were generated
using 5-fold serially diluted solutions of cDNA from the colon
cancer cell line LoVo. Standard curves were linear in the analyzed
range with an acceptable correlation coefficient (R2). The amount
of target gene expression was calculated from the standard curve.
Quantitative normalization of cDNA in each sample was performed
using the expression of the ACTB gene as an internal
control. mRNA levels of target genes were then provided as ratios
to ACTB mRNA levels. Real-time PCR assays were performed in
duplicate for each sample and the mean values were used for
calculations of the mRNA levels.
Immunohistochemical staining for CD133,
OCT4 and NANOG in UC and CRC
Sections (2 μm) of formalin-fixed, paraffin-embedded
specimens were produced. After deparaffinization and dehydration
for antigen unmasking, sections were brought to a boil in 10 mM
sodium citrate buffer. Sections were then blocked and incubated
with primary antibody overnight at 4°C. The antibody was detected
by Envision reagents (Envision kit/HRP, Dako Cytomation, Denmark).
Sections were counterstained with hematoxylin. Primary anti-CD133
rabbit monoclonal antibody (C24B9, Cell Signaling Technology Inc.,
Danvers, MA, USA), anti-OCT4 goat polyclonal antibody (C20, sc8629,
Santa Cruz Biotechnology, Santa Cruz, CA, USA), and anti-NANOG
rabbit polyclonal antibody (ab21603, Abcam plc, Cambridge, UK) were
used at a dilution of 1:100, and detected with the streptavidin
biotin method (LASB2 kit/HRP, Dako Cytomation, Denmark). Negative
controls were run simultaneously with pre-immune
immunoglobulin.
Statistical analysis
All statistical analyses were performed using JMP
version 5 (SAS Institute Inc. Cary, NC, USA). Relative mRNA levels
of each gene were expressed as median values (inter-quartile
range).
Associations between gene expression levels
(continuous variables) and groups (categorical variables) were
evaluated using Mann-Whitney U tests for two groups or
Kruskal-Wallis tests for multiple groups.
Box and whisker plots were used to summarize the
distribution of mRNA levels of PROM, POU5F1 and
NANOG for each group. The horizontal line in the box
represents the 50th quartile (median), and the upper and lower
lines of the box represent 75th and 25th quartiles, respectively.
The whiskers indicate the range of the measurements. P<0.05 was
considered to be statistically significant.
Results
Clinical characteristics of UC-CRC and UC
patients
The mean age of six UC-CRC patients (3 men and 3
women) was 39 years (range 28–51). Among the 6 patients, 3 (50%)
had extensive colitis and 3 (50%) had left-sided colitis. The
median duration of disease was 11 years (range 1–19).
The mean age of the 24 UC patients (14 men and 10
women) was 32 years (range 17 to 56 years). Among the 24 patients
with UC, 19 had extensive colitis and 5 had left-sided colitis. The
median duration of disease was 6 years (range 0.1–28) (Table I).
 | Table IClinical characteristics of UC-CRC
and UC patients. |
Table I
Clinical characteristics of UC-CRC
and UC patients.
| Variable | UC-CRC (n=6) | UC (n=24) |
|---|
| Gender |
| Male | 3 (50%) | 14 (58%) |
| Female | 3 (50%) | 10 (42%) |
| Age, mean
(range) | 39 (28–51) | 32 (17–56) |
| Age at diagnosis
mean (range) | 31 (18–50) | 26 (13–50) |
| Duration of disease
median (range) | 11 (1–19) | 6 (0.1–28) |
| Extent of
disease |
| Proctitis | 0 (0%) | 0 (0%) |
| Left-sided
colitis | 2 (33%) | 5 (21%) |
| Extensive
colitis | 4 (67%) | 19 (79%) |
| Severity of
imflammation |
| Mild | 3 (50%) | 1 (0.4%) |
| Moderate | 3 (50%) | 17 (74.6%) |
| Severe | 0 (0%) | 6 (25%) |
Clinical characteristics of UC-CRC and
sporadic CRC patients
In the UC-CRC patients, the primary tumor was
located in the rectum (n=3) or the colon (n=3). Pathological T
status (pT) of UC-CRC was pT1 (n=2) and pT3 (n=4). The UC-CRC were
well differentiated (n=2, 34%), moderately differentiated (n=1,
17%) or poorly/undifferentiated (n=3, 49%). Two patients with
UC-CRC were staged as Dukes’ A and 4 patients as Dukes’ B.
In sporadic CRC patients, the mean age of 37
patients (26 men and 11 women) was 63 years (range 37–82). These
tumors were located in the rectum (n=26) or the colon (n=11).
Distribution of pTs were pT1 (8%), pT2 (16%), pT3 (68%) and pT4
(8%). A total of 21 patients (57%) had pathological lymph node
metastases. The tumors were well-differentiated (n=19, 51%),
moderately differentiated (n=15, 40%) or poorly/undifferentiated
(n=3, 9%). Seven patients with sporadic CRC were staged as Dukes’
A, 7 as Dukes’ B, 12 as Dukes’ C and 11 as Dukes’ D (Table II).
 | Table IIClinicopathological characteristics
of UC-CRC and sporadic CRC patients. |
Table II
Clinicopathological characteristics
of UC-CRC and sporadic CRC patients.
| Variable | UC-CRC (n=6) | Sporadic CRC
(n=37) |
|---|
| Gender | | |
| Male | 3 (50%) | 26 (70%) |
| Female | 3 (50%) | 11 (30%) |
| Age, mean
(range) | 39 (28–51) | 63 (37–82) |
| Tumor location | | |
| Rectum | 3 (50%) | 26 (70%) |
| Colon | 3 (50%) | 11 (30%) |
| Tumor invasion | | |
| pT1 | 2 (33%) | 3 (8%) |
| pT2 | 0 (0%) | 6 (16%) |
| pT3 | 4 (67%) | 25 (68%) |
| pT4 | 0 (0%) | 3 (8%) |
| Lymph node
metastasis | | |
| Present | 0 (0%) | 21 (57%) |
| Absent | 6 (100%) | 16 (43%) |
| Histological
differentiation | | |
| Well | 2 (34%) | 19 (51%) |
| Moderate | 1 (17%) | 15 (40%) |
| Poor | 3 (49%) | 3 (9%) |
| Dukes’
classification | | |
| A | 2 (33%) | 7 (19%) |
| B | 4 (67%) | 7 (19%) |
| C | 0 (0%) | 12 (32%) |
| D | 0 (0%) | 11 (30%) |
Levels of stem cell markers in UC-CRC and
inflamed colonic epithelium
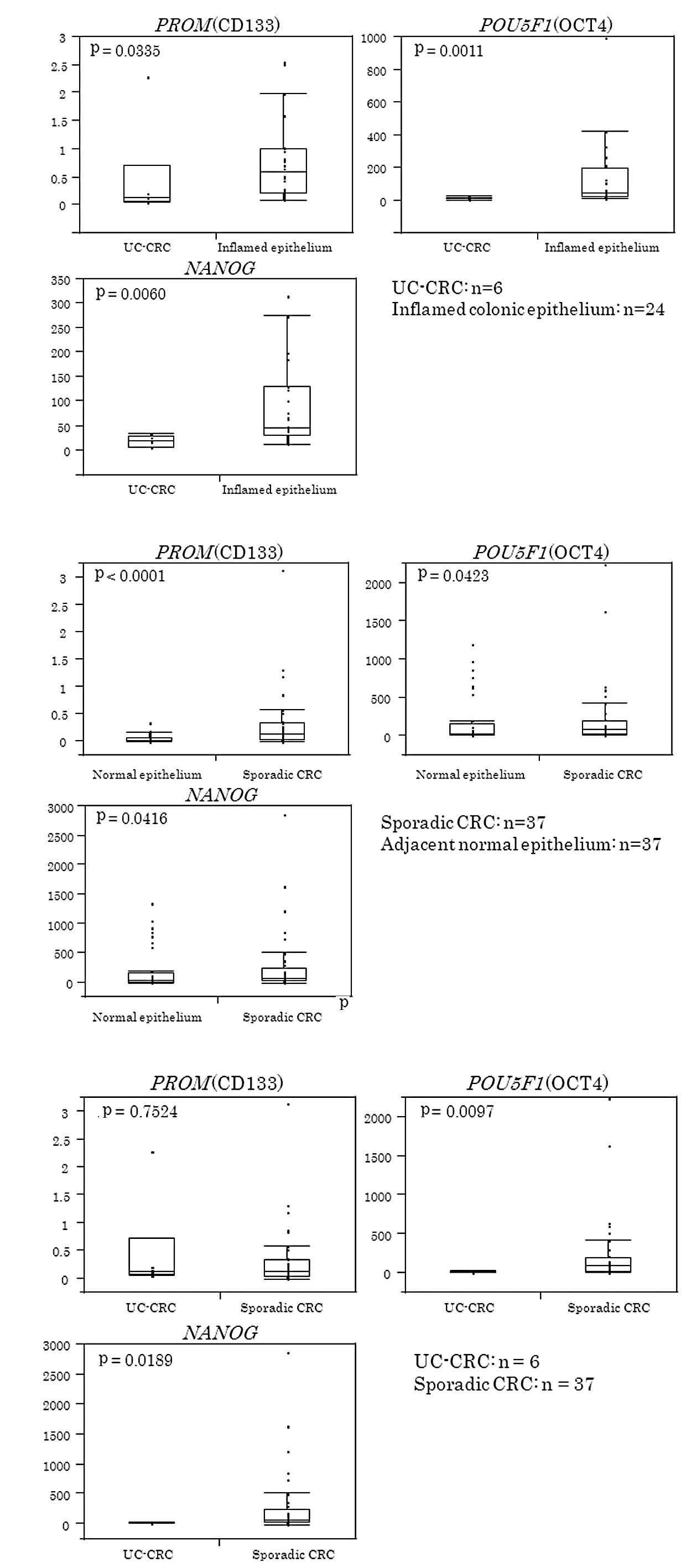
The relative mRNA levels of PROM,
POU5F1 and NANOG were expressed as ratios between the
gene of interest (PROM, POU5F1 and NANOG) and
the internal reference gene (ACTB), providing a
normalization factor for the amounts of the mRNAs.
Table III shows
the median value (inter-quartile range) for each gene in UC-CRC and
inflamed colonic epithelium. As shown in Fig. 1A, PROM, POU5F1 and
NANOG were significantly lower in colitis-associated CRC
than in inflamed colonic epithelium (P=0.0335 for PROM,
P=0.0011 for POU5F1 and P=0.006 for NANOG).
 | Table IIIStem cell markers in UC-CRC and
inflamed colonic epithelium. |
Table III
Stem cell markers in UC-CRC and
inflamed colonic epithelium.
| Stem cell
maker | UC-CRC (n=6) | Imflamed colonic
epithelium (n=24) |
|---|
| PROM (CD133,
range) | 0.138
(0.065–0.725) | 0.590
(0.205–1.006) |
| POU5F1
(OCT4, range) | 11.84
(8.298–18.12) | 44.59
(24.26–196.7) |
| NANOG | 19.15
(6.998–28.54) | 46.16
(30.08–130.2) |
Levels of stem cell markers in sporadic
CRC and adjacent normal epithelium
Table IV shows the
median value (inter-quartile range) of each gene in sporadic CRC
and the adjacent normal epithelium. As shown in Fig. 1B, PROM, POU5F1 and
NANOG were significantly higher in sporadic CRC than in
adjacent normal colonic epithelium (P=0.0001 for PROM,
P=0.0423 for POU5F1 and P=0.0416 for NANOG).
 | Table IVStem cell markers in sporadic CRC and
normal colonic epithelium. |
Table IV
Stem cell markers in sporadic CRC and
normal colonic epithelium.
| Stem cell
maker | Sporadic CRC
(n=6) | Normal colonic
epithelium (n=37) |
|---|
| PROM (CD133,
range) | 0.274
(0.137–0.830) | 0.129
(0.033–0.345) |
| POU5F1
(OCT4, range) | 29.48
(11.74–61.20) | 91.00
(24.80–197.0) |
| NANOG | 31.47
(17.44–74.69) | 70.70
(26.50–246.2) |
Comparison of PROM, POU5F1 and NANOG in
UC-CRC and sporadic CRC
Fig. 1C shows that
POU5F1 and NANOG mRNA levels were significantly lower
in colitis-associated CRC than in sporadic CRC (P=0.0097 for
POU5F1, and P=0.0189 for NANOG). No significant
difference was observed in PROM between colitis-associated
and sporadic CRC.
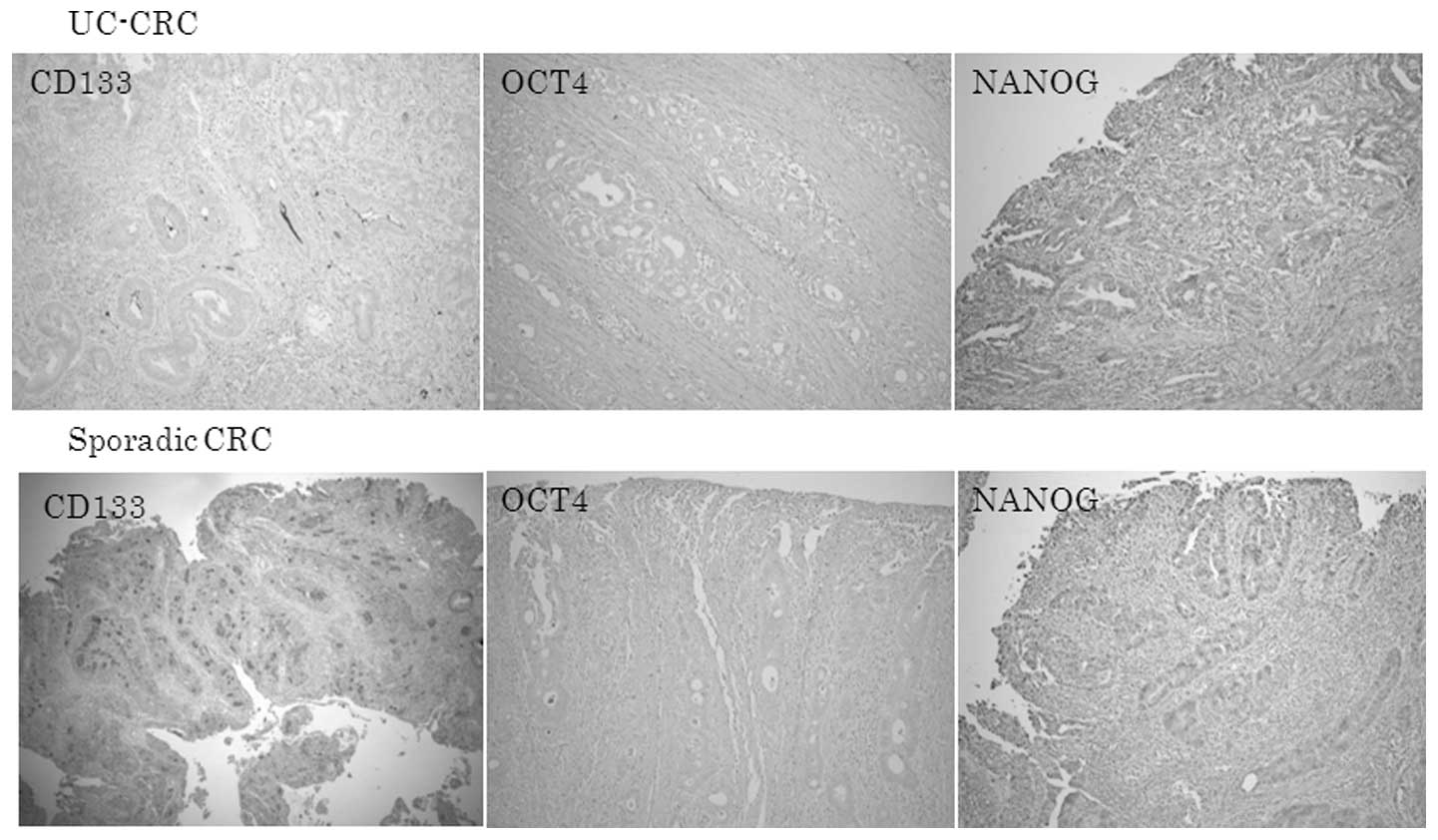
Immunoreactive CD133, OCT4 and NANOG in
UC-CRC and sporadic CRC
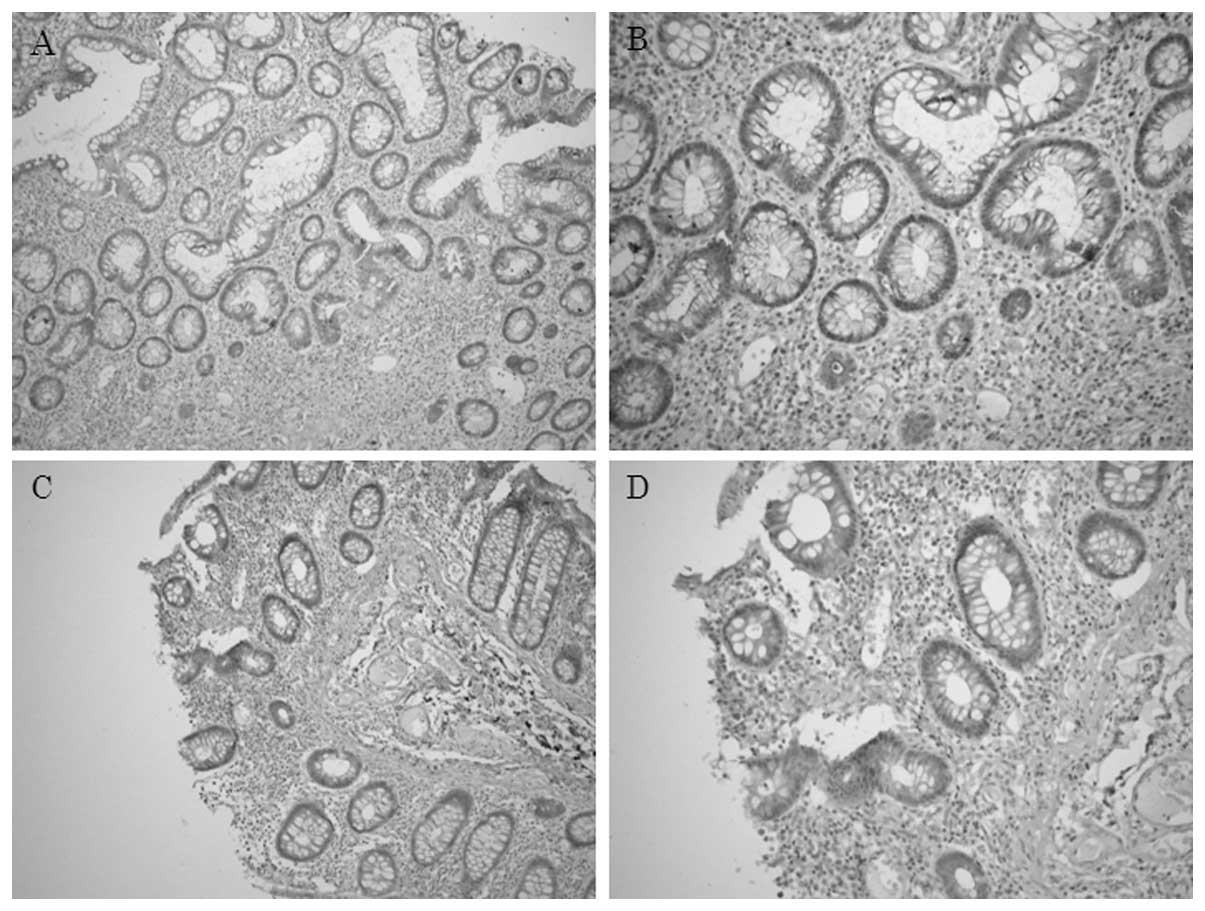
Fig. 2 shows that
the expression of CD133, OCT4 and NANOG proteins was also lower in
UC-CRC than in sporadic CRC.
Immunoreactive CD133 protein was observed in a
minority of CRC cells. CD133 was located at the apical/endoluminal
surface (membranous), in the cytoplasm (cytoplasmic) or in both
sites, for CRC cells (Fig. 4).
In UC-CRC and sporadic CRC, OCT4 was found in the
cytoplasm of cancer cells. Although germ cell tumors have been
reported to show strong nuclear OCT4 immunostaining, colorectal
cancer cells had diffuse cytoplasmic OCT4 staining.
Diffuse cytoplasmic NANOG protein was detected in
UC-CRC cells. Sporadic CRC cells showed, not only cytoplasmic, but
also nuclear NANOG immunoreactivity.
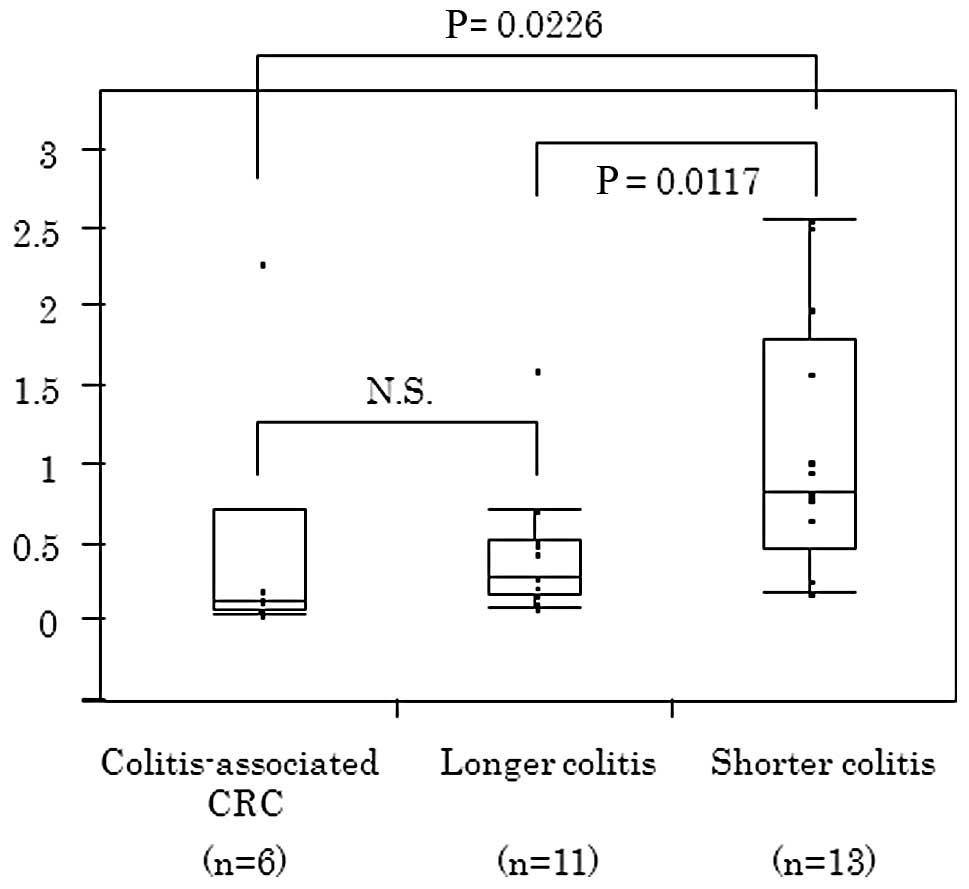
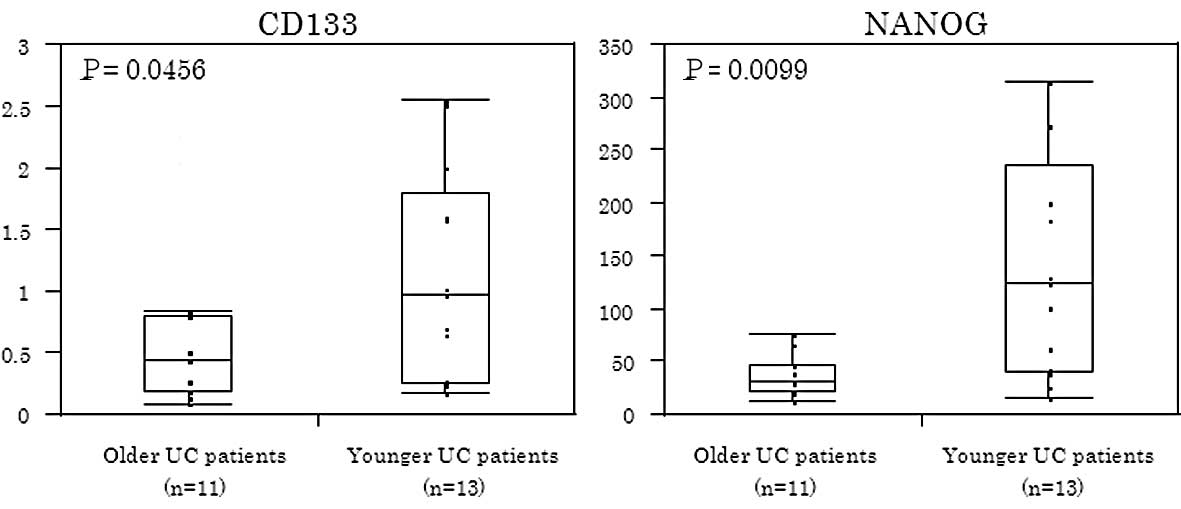
Association between CD133, OCT4, and
NANOG in inflamed colonic epithelium and disease or patient
characteristics
The expression of CD133 and NANOG proteins in
inflamed colonic epithelium was significantly higher among younger
UC patients (P<0.05) (Fig. 3).
CD133 in inflamed colonic epithelium was significantly associated
with the duration of colitis. Based on the median value of the
duration of colitis, 24 patients were divided into two groups
(shorter duration colitis, n=13; and longer duration colitis,
n=11). As shown in Fig. 4, patients
with shorter periods of colitis showed a higher CD133 expression
than patients with colitis of longer duration (P=0.0117) or
patients with UC-CRC (P=0.0226). No significant difference in CD133
levels was found between UC-CRC patients and longer duration
colitis patients.
Immunohistochemical staining of CD133 in
inflamed colonic epithelium
In UC patients, the minority of inflamed colonic
epithelial cells expressed immunoreactive CD133 protein (Fig. 5). CD133 was observed diffusely in
the cytoplasm of epithelial cells and was also located at the
apical/endoluminal surface (membranous), in the cytoplasm or in
both sites, of inflamed colonic epithelial cells.
Discussion
To the best of our knowledge, no report has
investigated the expression of the three stem cell markers
considered in this study in the context of UC-CRC or inflamed
colonic epithelium, compared to sporadic CRC.
Stem cells capable of self-renewal and pluripotency
contribute to normal tissue development, regeneration and disease
(16). Recently, the CSC concept
has been advanced through the use of isolation techniques dependent
upon cell surface markers for putative CSCs and functional assays
of stem/progenitor cell properties in non-obese diabetic severe
combined immunodeficient mice (17,18).
CD133 is one of the most significant cell surface markers of colon
CSCs (19). A recent report showed
that CD133 immunoreactivity was associated with poor survival in
sporadic CRC (14). POU5F1
and NANOG play significant roles in maintaining pluripotency
and self-renewal of SCs (11).
Although each stem cell marker has been reported to be expressed in
certain human malignancies, the clinical significance of these stem
cell markers in UC-CRC has yet to be established.
We demonstrated that UC-CRC had a significantly
lower expression of PROM, POU5F1 and NANOG
genes compared to inflamed colonic epithelium, whereas sporadic CRC
had a significantly higher expression of these genes compared to
adjacent normal colonic epithelium. UC-CRC has been reported to
develop along a different genetic pathway compared to sporadic CRC.
Previous studies showed that mutations of the TP53 (p53) gene were
observed in the early stage, and adenomatous polyposis coli gene or
k-ras gene mutations were less frequent events in UC-CRC (20–22).
Although UC-CRC appears to have a completely different carcinogenic
pathway from sporadic CRC, the mechanisms underlying these
differences are not understood. Our stem cell marker analysis may
support this concept, showing genetic or carcinogenic differences
between UC-CRC and sporadic CRC. Another possible interpretation of
our results is that colonic SCs or CSCs scarcely contribute to
UC-associated carcinogenesis relative to sporadic CRC. However,
further analyses are required to address the reason for stem cell
markers being lower in UC-CRC compared with sporadic CRC or
inflamed colonic epithelium.
We also demonstrated that the CD133 level in
inflamed colonic epithelium was significantly lower in UC patients
with a longer duration of disease than those with a shorter
duration. These results indicate that decreased CD133 levels in the
colonic mucosa of UC patients may identify patients at higher risk
for developing UC-CRC.
Periodic surveillance colonoscopy with two to four
random biopsies collected at 10 cm intervals throughout the entire
colon is now highly recommended for the early detection of UC-CRC
(23). To increase the macroscopic
detection rate of precancerous or dysplastic lesions, methylene
blue or indigo carmine chromoendoscopy with careful inspection have
also been utilized (24,25). However, current surveillance systems
are unsatisfactory for the detection of dysplasia and early-stage
UC-CRC due to the difficulties associated with endoscopic or
histological assessment.
The analysis of the CD133 level in colonoscopic
biopsy specimens in addition to conventional cancer risk evaluation
may increase the identification rate of patients who are likely to
develop UC-CRC. If reliable and reproducible evaluation criteria
for immunohistochemical CD133 expression are established for
inflamed colonic mucosa, it may be an easy and useful supplementary
method to predict the development of UC-CRC.
However, our data should be interpreted with
caution. A significant limitation of this study was the relatively
small number of UC patients (n=30), including only six patients
with UC-CRC. Large prospective trials are required to confirm our
results.
In conclusion, UC-CRC showed different expression
profiles of stem cell markers compared with sporadic CRC. A
decreased CD133 expression in inflamed colonic epithelium may
identify UC patients at a high risk for the development of
UC-CRC.
References
|
1
|
Eaden JA, Abrams KR and Mayberry JF: The
risk of colorectal cancer in ulcerative colitis: a meta-analysis.
Gut. 48:526–535. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Zisman TL and Rubin DT: Colorectal cancer
and dysplasia in inflammatory bowel disease. World J Gastroenterol.
14:2662–2669. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Gupta RB, Harpaz N, Itzkowitz S, Hossain
S, Matula S, Kornbluth A, Bodian C and Ullman T: Histologic
inflammation is a risk factor for progression to colorectal
neoplasia in ulcerative colitis: a cohort study. Gastroenterology.
133:1099–1105. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Watanabe T, Kobunai T, Toda E, et al: Gene
expression signature and the prediction of ulcerative
colitis-associated colorectal cancer by DNA microarray. Clin Cancer
Res. 13:415–420. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Fujii S, Tominaga K, Kitajima K, et al:
Methylation of the oestrogen receptor gene in non-neoplastic
epithelium as a marker of colorectal neoplasia risk in longstanding
and extensive ulcerative colitis. Gut. 54:1287–1292. 2005.
View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Nishikawa M, Oshitani N, Matsumoto T,
Nishigami T, Arakawa T and Inoue M: Accumulation of mitochondrial
DNA mutation with colorectal carcinogenesis in ulcerative colitis.
Br J Cancer. 93:331–337. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Bartsch H and Nair J: Chronic inflammation
and oxidative stress in the genesis and perpetuation of cancer:
role of lipid peroxidation, DNA damage, and repair. Langenbecks
Arch Surg. 391:499–510. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Boman BM and Huang E: Human colon cancer
stem cells: a new paradigm in gastrointestinal oncology. J Clin
Oncol. 26:2828–2838. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Vermeulen L, Sprick MR, Kemper K, Stassi G
and Medema JP: Cancer stem cells – old concepts, new insights. Cell
Death Differ. 15:947–958. 2008.
|
|
10
|
Shipitsin M and Polyak K: The cancer stem
cell hypothesis: in search of definitions, markers, and relevance.
Lab Invest. 88:459–463. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Liang J, Wan M, Zhang Y, et al: Nanog and
Oct4 associate with unique transcriptional repression complexes in
embryonic stem cells. Nat Cell Biol. 10:731–739. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Tai MH, Chang CC, Kiupel M, Webster JD,
Olson LK and Trosko JE: Oct4 expression in adult human stem cells:
evidence in support of the stem cell theory of carcinogenesis.
Carcinogenesis. 26:495–502. 2005.PubMed/NCBI
|
|
13
|
Wang J, Levasseur DN and Orkin SH:
Requirement of Nanog dimerization for stem cell self-renewal and
pluripotency. Proc Natl Acad Sci USA. 105:6326–6331. 2008.
View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Horst D, Kriegl L, Engel J, Kirchner T and
Jung A: CD133 expression is an independent prognostic marker for
low survival in colorectal cancer. Br J Cancer. 99:1285–1289. 2008.
View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Bijwaard KE, Aguilera NS, Monczak Y,
Trudel M, Taubenberger JK and Lichy JH: Quantitative real-time
reverse transcription-PCR assay for cyclin D1 expression: utility
in the diagnosis of mantle cell lymphoma. Clin Chem. 47:195–201.
2001.PubMed/NCBI
|
|
16
|
Lanzoni G, Roda G, Belluzzi A, Roda E and
Bagnara GP: Inflammatory bowel disease: Moving toward a stem
cell-based therapy. World J Gastroenterol. 14:4616–4626. 2008.
View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Ricci-Vitiani L, Lombardi DG, Pilozzi E,
et al: Identification and expansion of human
colon-cancer-initiating cells. Nature. 445:111–115. 2007.
View Article : Google Scholar : PubMed/NCBI
|
|
18
|
O’Brien CA, Pollett A, Gallinger S and
Dick JE: A human colon cancer cell capable of initiating tumour
growth in immunodeficient mice. Nature. 445:106–110.
2007.PubMed/NCBI
|
|
19
|
Ieta K, Tanaka F, Haraguchi N, et al:
Biological and genetic characteristics of tumor-initiating cells in
colon cancer. Ann Surg Oncol. 15:638–648. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Brentnall TA, Crispin DA, Rabinovitch PS,
et al: Mutations in the p53 gene: an early marker of neoplastic
progression in ulcerative colitis. Gastroenterology. 107:369–378.
1994.PubMed/NCBI
|
|
21
|
Tarmin L, Yin J, Harpaz N, et al:
Adenomatous polyposis coli gene mutations in ulcerative
colitis-associated dysplasias and cancers versus sporadic colon
neoplasms. Cancer Res. 55:2035–2038. 1995.PubMed/NCBI
|
|
22
|
Chaubert P, Benhattar J, Saraga E and
Costa J: K-ras mutations and p53 alterations in neoplastic and
nonneoplastic lesions associated with longstanding ulcerative
colitis. Am J Pathol. 144:767–775. 1994.PubMed/NCBI
|
|
23
|
Farrell RJ and Peppercorn MA: Ulcerative
colitis. Lancet. 359:331–340. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Matsumoto T, Nakamura S, Jo Y, Yao T and
Iida M: Chromoscopy might improve diagnostic accuracy in cancer
surveillance for ulcerative colitis. Am J Gastroenterol.
98:1827–1833. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Rutter MD, Saunders BP, Schofield G,
Forbes A, Price AB and Talbot IC: Pancolonic indigo carmine dye
spraying for the detection of dysplasia in ulcerative colitis. Gut.
53:56–260. 2004. View Article : Google Scholar : PubMed/NCBI
|