Introduction
Findings of the majority of meta-analyses of
randomized trials with surgery versus surgery and chemoradiotherapy
for advanced esophageal cancer showed that preoperative
chemoradiotherapy is beneficial in improving outcome for patients
with locally advanced esophageal cancer compared with surgery alone
(1–4). Despite recent advances in
multimodality treatment, complete pathological response to
chemoradiotherapy occurred in 10–45.5% of patients with advanced
esophageal cancer (5). Patients
with advanced esophageal cancer are not likely to reap any benefits
from chemoradiotherapy. The prediction of chemoradiosensitivity for
patients with advanced esophageal cancer is necessary to determine
the therapeutic course prior to treatment. Various studies have
identified candidates for molecular markers to predict the efficacy
of chemoradiotherapy for advanced esophageal cancer using biopsy
specimens prior to chemoradiotherapy (6–14).
These studies demonstrated the correlation between the response of
chemoradiotherapy and the expression of molecular markers including
apoptosis, cell cycle, stress, DNA damage and proliferation-related
genes. Among them, p53 and its related genes, p21 and bax, which
play a pivotal role in the regulation of cell fate, have been
investigated the most in the evaluation of chemoradiosensitivity
(7–10). Regarding apoptosis-related genes,
bcl-2 is also known to act as an apoptotic suppressor (10). Moreover, the heat shock protein
family, including HSP27, HSP70 and HSP90, has been demonstrated to
have anti-apoptotic effects and is resistant to chemo- and
radiotherapy (11). In particular,
apoptosis induced by radiation occurred due to DNA double-strand
breaks that are predominantly repaired by the binding of Ku70 and
Ku86 proteins to the free DNA ends followed by recruitment of the
catalytic subunit of DNA-dependent protein kinase (12,13).
Hypoxic conditions with hypoxia-inducible factor 1α (HIF-1α)
expression also are resistant to chemotherapy and radiotherapy
(14). Although these molecules may
contribute to predicting the efficacy of chemoradiotherapy in
esophageal cancer, at present there is no consensus regarding the
application of these markers in clinical practice.
In this study, we focused on the detection of early
response to chemoradiotherapy to determine the appropriate
therapeutic course, resulting in the prevention of severe adverse
events, and reduction of the costs involved for patients with
esophageal cancer. Thus, we investigated the apoptotic index (AI)
immediately prior to treatment and following a radiation dose of 10
Gy using biopsy specimens. Additionally, we examined molecular
marker candidates for chemoradiosensitivity, including p53, p21,
bax, bcl-2, HSP27, HSP70, HSP90, Ku70, Ku86 and HIF-1α, as
previously reported (6–14).
Materials and methods
Patients and tissue samples
Biopsy specimens were obtained endoscopically from
28 patients (26 males and 2 females) with esophageal squamous cell
carcinoma prior to chemoradiotherapy or radiotherapy and following
a radiation dose of 10 Gy in one week at the Saitama Medical
Center, Japan, between November 2007 and December 2008. The median
age of the patients was 70 years (range 52–83). The location of the
primary tumor was as follows: cervical esophagus in 1 patient,
upper thoracic esophagus in 8 patients, middle thoracic esophagus
in 12 patients and lower thoracic esophagus in 7 patients. Tumor
stage was classified according to the sixth edition of the TNM
classification of the International Union against Cancer (UICC)
(15). Tumor stage: stage I, 4
patients; stage II, 5 patients; stage III, 14 patients; and stage
IV, 5 patients. Biopsy specimens were fixed in formalin, embedded
in paraffin and sectioned at a thickness of 4 μm. The samples were
examined following hematoxylin and eosin staining.
Immunohistochemical studies and an apoptosis study were also
performed. Written informed consent to participate in the study was
obtained from each patient prior to treatment, according to the
ethics guidelines of Saitama Medical Center, Saitama Medical
University.
Treatment protocol
Following diagnosis, the patients underwent
radiotherapy or chemoradiotherapy, consisting of concurrent
radiotherapy and chemotherapy, for 7 weeks. External-beam
radiotherapy was delivered by a two-field technique using a 10 MV
photon beam and the total dose was 60–70 Gy in 30–35 fractions.
Radiation therapy without concurrent chemotherapy was performed in
4 patients. A total of 24 patients received the following
concurrent chemotherapy: 13 patients underwent a regimen of 70
mg/m2 cisplatinum administered intravenously over 1 h on
days 1 and 29, and 700 mg/m2 5-fluorouracil (5-FU)
administered as a continuous intravenous infusion on days 1–5 and
29–33. Two patients received 6.6 mg/m2 cisplatinum
administered intravenously over 1 h on days 1–5, 8–12 and 29–33,
and 350 mg/m2 5-FU was administered as a continuous
intravenous infusion on days 1–5, 8–12 and 29–33. Nine patients
received the regimen that consisted of 6.6 mg/m2
docetaxel administered intravenously over 1.5 h on days 1, 8, 15,
22, 29 and 37.
Clinical features and evaluation of
treatment
Prior to treatment, all 28 patients were evaluated
by radiographic examination (chest X-rays and barium swallow),
endoscopy (esophagoscopy and in certain cases bronchoscopy),
endoscopic ultrasonography and computed tomography (CT). Biopsy
samples were obtained from three or more points. The clinical
response was evaluated 2 weeks following the end of treatment
according to the Response Evaluation Criteria in Solid Tumors
(RECIST) (16) and the guidelines
of the Japanese Society for Esophageal Diseases (JSED) (17,18).
When the case had a lesion that could be evaluated, we evaluated
the response according to RECIST. When such a lesion was not
present, we evaluated the response according to the guidelines of
JSED. Assessment included repeated endoscopy and CT scans.
Endoscopy was carried out by two investigators. All 28 patients
underwent a CT scan of the neck, chest and abdomen. CT was
performed at a slice width of 10 mm from the neck to the bottom of
the liver using an intravenous contrast medium. The response was
classified as complete response, partial response (>30%
decrease), stable disease (<30% decrease) and progressive
disease in the treatment lesion.
Immunohistochemical staining
Immunohistochemical staining was performed by the
labeled streptavidin biotinylated antibody (LSAB) method using a
Super Sensitive Detection Kit (BioGenex Laboratories, Inc., CA,
USA). Paraffin-embedded histological sections (4-μm) were
deparaffinized and washed with water, and then endogenous
peroxidase activity was blocked with 0.3%
H2O2 in methanol. After washing in phosphate-
buffered saline (PBS), a blocking agent (Dako, Glostrup, Denmark)
was used to regulate non-specific reactivity. For antigen
retrieval, the sections were autoclaved at 121˚C for 15 min or in a
microwave oven for 10 min. These sections were then incubated with
the primary antibodies at room temperature for 60 min or overnight.
After washing in PBS, tissues were incubated with biotin-labeled
anti-rabbit or anti-mouse secondary antibodies for 20 min at room
temperature and then reacted with streptavidin-biotin horseradish
peroxidase complex for 20 min. Immunostaining was visualized by
developing the slides in diaminobenzidine (DAB). The sections were
lightly counterstained with hematoxylin. Negative controls were
prepared by substituting blocking buffer for each primary antibody,
and no detectable staining was evident.
Antibodies were purchased from the following
manufacturers: monoclonal antibody (Mab) specific for p53 (DO-7;
DAKO A/S, Glostrup, Denmark; 1:40), Mab specific for p21 (4D10;
Novocastra Laboratories Ltd., Newcastle, UK; 1:20), Mab specific
for bax (sc-7480; Santa Cruz Biotechnology, Inc., Santa Cruz, CA,
USA; 1:100), Mab specific for bcl-2 (124; DAKO A/S; 1:100), Mab
specific for HSP27 (G3.1; StressGen Biotechnologies Corporation,
Victoria, BC, Canada; 1:400), Mab specific for HSP70 (C92F3A-5;
StressGen Biotechnologies Corporation; 1:100), Mab specific for
HSP90 (k3705; StressGen Biotechnologies Corporation; 1:600), Mab
specific for Ku70 (M-19; Santa Cruz Biotechnology, Inc.; 1:500),
Mab specific for Ku86 (M-20; Santa Cruz Biotechnology, Inc.; 1:20)
and Mab specific for HIF-1α (OZ12; Thermo Fisher Scientific Inc.
Waltham, MA, USA; 1:10).
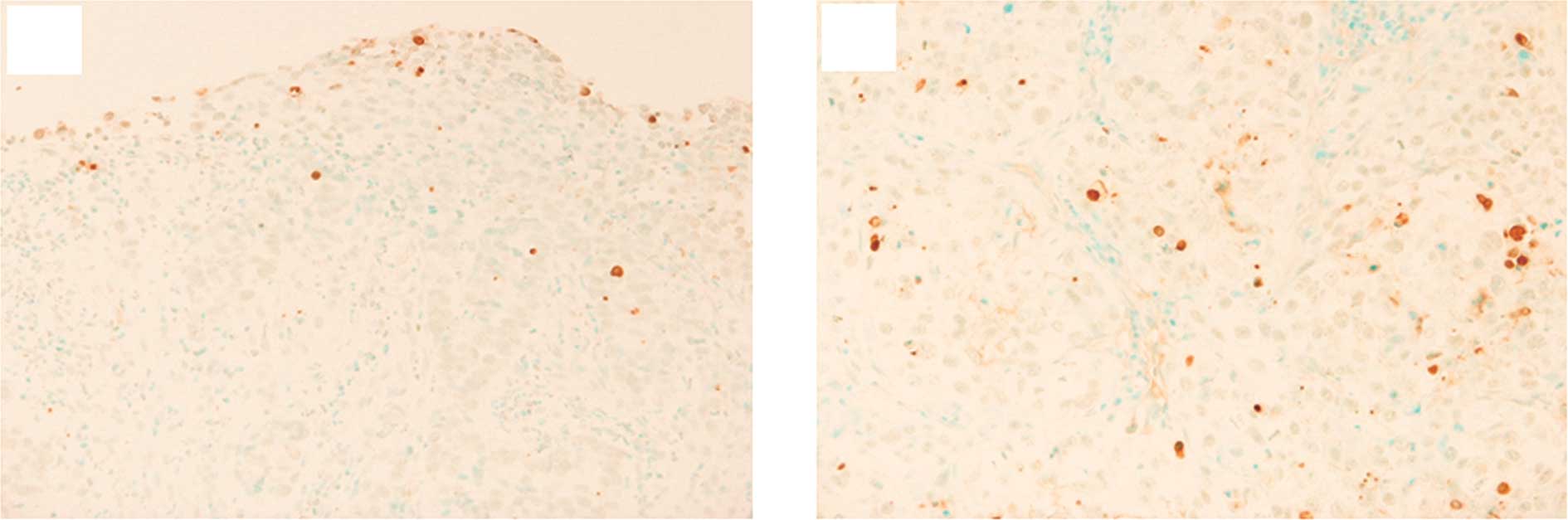
TUNEL method
Apoptotic cells were determined by the TUNEL method.
Apoptotic cells were visualized using the ApopTag Plus peroxidase
in situ apoptosis detection kit (Chemicon International,
Temecula, CA, USA). Formalin-fixed, paraffin-embedded sections were
deparaffinized in xylene and dehydrated through graded alcohol.
Briefly, following routine deparaffinization, sections were
incubated with proteinase K for 15 min at room temperature. The
sections were washed twice in distilled water for 2 min each time
and incubated with 3% H2O2 for 5 min. The
sections were subjected to enzymic homopolymeric tailing with TdT
and digoxigenin-labeled nucleotides for 60 min at room temperature
in a humidified atmosphere. The nucleotides incorporated were
revealed by incubation with anti-digoxigenine antibody bound to
peroxidase for 30 min at room temperature. Immunostaining was
visualized by developing the slides in DAB. Counterstaining was
performed with methyl green.
Evaluation of molecular marker expression
and the AI
Expression of molecular markers was evaluated as
positive when the nucleus and/or cytoplasm of cancer tissue
indicated at least 5% dye-affinity when the total field of view was
observed at a magnification of ×40. The AI was statistically
averaged as the number of positive cells among >1,000 tumor
cells counted in three randomly selected areas. The AI ratio (AIR)
was determined by dividing the AI following 10 Gy radiation by the
pretreatment AI. Assessment of the staining was evaluated by two
independent pathologists who had no access to data pertaining to
the clinical status of the patients.
Statistical analysis
Associations between categorical variables and the
expression of molecular markers were evaluated with the Fisher’s
exact probability test, Mann-Whitney’s U test, Wilcoxon
signed-ranks test and the paired t-test. A receiver operating
characteristics (ROC) curve was generated to determine the optimal
cut-off value for diagnostic discrimination. The differences at
P-values <0.05 were considered significant, and all P-values
reported were two-sided. Statistical analyses were carried out
using Statflex (ver6.0 Artec, Osaka, Japan).
Results
Correlation between clinicopathological
characteristics and the response to chemoradiotherapy
Regarding the efficacy of chemoradiotherapy, there
was a complete response in 5 patients (17.9%), a partial response
in 14 patients (50%), stable disease in 6 patients (21.4%) and
progressive disease in 3 patients (10.7%). The patients were
divided into two groups depending on the response: responder group
(RG) (n=19), including the patients with complete or partial
response, and the non-responder group (NRG) (n=9), which included
patients with stable or progressive disease. The correlation
between the patient characteristics and the response to
chemoradiotherapy is shown in Table
I. No correlations were statistically observed between RG and
NRG in terms of age, gender, tumor location, depth of invasion,
regional lymph node, distant metastasis and UICC stage.
 | Table ICorrelation between
clinicopathological characteristics and response to
chemoradiotherapy. |
Table I
Correlation between
clinicopathological characteristics and response to
chemoradiotherapy.
| Responders
(n=19) | Non-responders
(n=9) | P-value |
|---|
| Age median
(range) | 74 (62–80) | 68 (52–83) | 0.27 |
| Gender | | | 0.99 |
| Male (n=26) | 18 | 8 | |
| Female (n=2) | 1 | 1 | |
| Location | | | 0.27 |
| Cervical (n=1) | 1 | 0 | |
| Upper thoracic
(n=8) | 7 | 1 | |
| Middle thoracic
(n=12) | 8 | 4 | |
| Lower thoracic
(n=7) | 3 | 4 | |
| Depth of
invasion | | | 0.14 |
| T1 (n=4) | 4 | 0 | |
| T2 (n=5) | 3 | 2 | |
| T3 (n=15) | 8 | 7 | |
| T4 (n=4) | 4 | 0 | |
| Regional lymph
node | | | 0.44 |
| N0 (n=9) | 7 | 2 | |
| N1 (n=19) | 12 | 7 | |
| Distant
metastasis | | | 0.68 |
| M0 (n=23) | 16 | 7 | |
| M1 (n=5) | 3 | 2 | |
| Stage | | | 0.52 |
| I (n=4) | 4 | 0 | |
| II (n=5) | 3 | 2 | |
| III (n=14) | 9 | 5 | |
| IV (n=5) | 3 | 2 | |
AI comparing with RG and NRG
Using biopsy specimens, the AI was examined prior to
treatment and following a radiation dose of 10 Gy in RG and NRG
(Fig. 1A and B). In RG and NRG, AI
of pretreatment was 4.7±5.3 (cells/1000 cells) and 5.9±3.7,
respectively (P=0.18). Following a radiation dose of 10 Gy, the AI
was 12.9±6.8 in RG and 11.0±10 in NRG (P=0.36). No statistically
significant difference was found between these groups prior to
treatment and following 10 Gy radiation (Table II).
 | Table IIApoptotic index. |
Table II
Apoptotic index.
| Responders
(n=19) | Non-responders
(n=9) | P-value |
|---|
| Pretreatment | 4.7±5.3 | 5.9±3.7 | 0.18 |
| After 10 Gy | 12.9±6.8 | 11.0±10 | 0.36 |
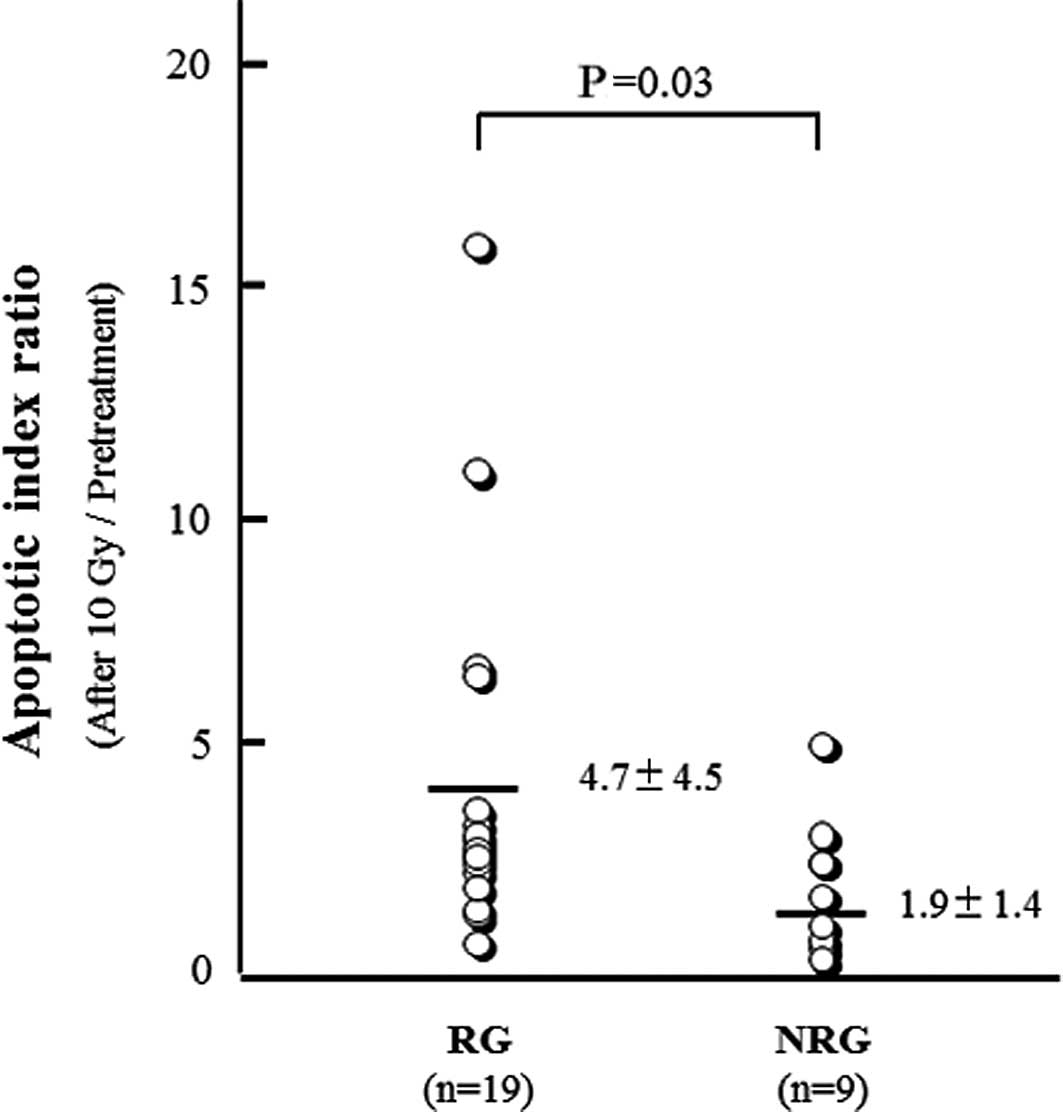
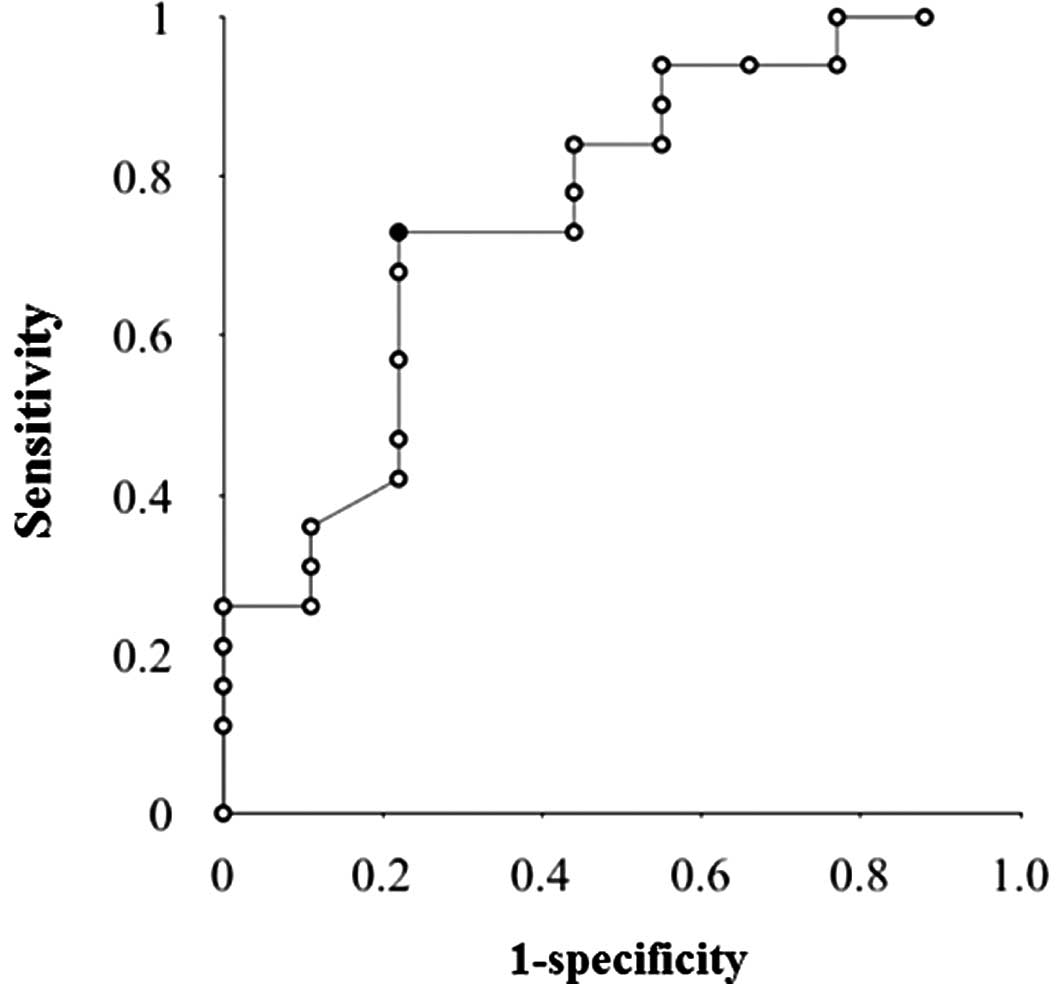
We then analyzed the AIR of prior to treatment and
10 Gy radiation. AIR was found to be 4.7±4.5 in RG and 1.9±1.4 in
NRG. The AIR of RG was significantly higher than that of NRG
(P=0.03) (Fig. 2). When the ROC
curve was generated to determine the optimal cut-off value for
predicting the response of chemoradiotherapy using AIR, the area
under the ROC curve was 0.78 (Fig.
3). Based on the result of the ROC curve, when the cut-off
value of AIR was set at 2.4, the sensitivity, specificity and
accuracy were 74, 78 and 76%, respectively.
Correlation between the expression of
molecular markers and the chemoradiosensitivity
Using biopsy specimens, we examined the expression
of the molecular markers, including p53, p21, bax, bcl-2, HSP27,
HSP70, HSP90, Ku70, Ku86 and HIF-1α, immunohistochemically prior to
treatment and following a radiation dose of 10 Gy, and analyzed the
correlation between the protein expression and
chemoradiosensitivity. The positive expression of p53 prior to
treatment is associated with the efficacy of chemoradiotherapy, no
statistical significance was observed (p=0.08). Regarding further
molecular expression in biopsy specimens obtained prior to
treatment and following a radiation dose of 10 Gy, no significant
correlations were found in RG and NRG.
Discussion
The candidates for molecular markers for the
prediction of chemoradiosensitivity for esophageal cancer have been
investigated to identify the responders or non-responders prior to
treatment. Chemoradiosensitivity may be used to allow appropriate
treatment to be administered for predicted responders and to
prevent severe adverse events and save costs for predicted
non-responders. A number of molecular markers have been examined
retrospectively and reported as good predictors for
chemoradiotherapy in esophageal cancer (6–14). It
is reasonable that most of these markers are associated with the
apoptotic pathway. However, consensus regarding the application of
these markers in clinical practice has not been reached. The aim of
the present study was to find the appropriate marker for the
prediction of tumor response against chemoradiosensitivity at a
relatively early step, and then focus on the observation of the
apoptotic cells directory using a TUNEL method as an AI. Based on
this hypothesis, we compared the AI of biopsy specimens following a
radiation dose of 10 Gy with that prior to treatment. As a result,
we found that AIR reflected the efficacy of chemoradiotherapy. AIR
of RG was significantly higher than that of NRG. Furthermore, the
sensitivity, specificity and accuracy were approximately 75% when
the cut-off value of AIR was set at 2.4. These results appear to be
significant.
We chose the evaluation point of 10 Gy (5 days)
following radiation. The clinically crucial objective is to make a
go/no-go decision for chemoradiotherapy by precise assessment of
chemoradiosensitivity at a relatively early stage. Although we are
not able to emphasize the reason for 10 Gy being the most
appropriate dose to judge the early efficacy of chemoradiotherapy,
the evaluation of the apoptotic state at 10 Gy appears to be an
acceptable dose to satisfy the clinical value as mentioned above. A
radiation dose of 9 Gy reportedly induces recruitment of cancer
cells from the heterogeneous cell cycling population to the
synchronous cycling cell population, resulting in the enhancement
of radiosensitivity (19). As a
result, the high growth fraction at 9 Gy was associated with a
favorable prognosis in cervical cancer patients (19). Moreover, another study demonstrated
that evaluation following 10 Gy doses of radiotherapy was useful in
predicting the response to radiotherapy in oral squamous cell
carcinoma (20). In in vitro
experiments, 2–10 Gy radiation substantially induced apoptosis
using cancer cells (21,22). We observed an apparent increase of
apoptotic cells in numerous biopsy specimens obtained following a
radiation dose of 10 Gy compared with that prior to treatment.
Therefore, our results suggest that the assessment of AIR was
appropriate to predict the efficacy of chemoradiotherapy for the
patients with advanced esophageal squamous cell carcinoma.
We further examined the expression of molecular
markers, including p53, p21, bax, bcl-2, HSP27, HSP70, HSP90, Ku70,
Ku86 and HIF-1α, which were previously shown to be candidates for
the prediction of chemoradiosensitivity. In our results, the
expression of these markers was not associated with the efficacy of
chemoradiotherapy using biopsy specimens obtained prior to
treatment. Moreover, the marked alteration of these markers was not
observed in tissues following a radiation dose of 10 Gy when
compared with that prior to treatment. Among those molecules,
p53-positive expression in pretreatment tissues had a tendency to
link to the efficacy of chemoradiotherapy. The p53 gene is one of
the most investigated genes and is mutated in approximately 50% of
cases in numerous types of cancer. Intensive studies have suggested
that wild-type p53 acts as a key inducer for apoptosis and cell
cycle arrest against anti-cancer agents and radiation, while
mutated p53 has achieved radioresistance and chemoresistance.
However, p53 status does not necessarily correspond to the clinical
value. A number of reports have shown that the patients with
immunohistochemically p53-positive expression have a good prognosis
and chemosensitivity in esophageal cancer (7,10),
although the opposite results have also been shown (8,23,24).
Another argument is that p53 status is not associated with
chemoradiosensitivity and prognosis for patients with esophageal
cancer (25,26). Based on these results, even p53 may
be unsuitable as a predictive marker of chemoradiosensitivity.
Therefore, it is unlikely that a single molecular marker to predict
the efficacy of chemoradiotherapy can be identified.
In the case that patients with early stages of
esophageal cancer have high-risk factors for surgical treatment or
desire to preserve laryngeal function, chemoradiotherapy would be
administered, although surgical treatment is also likely to produce
favorable results. If we were able to predict at an earlier stage
that the response for chemoradiotherapy is likely to be poor, then
surgical treatment should be re-considered for patients with early
stage cancer during chemoradiotherapy. That is certainly the case
with patients with advanced stage. Therefore, our study appears to
provide significant results, despite certain limitations. For
example, the number of clinical cases was small and the regimens of
chemotherapy combined with radiotherapy were not integrated. Based
on the results, the cases treated with identical regimens of
chemoradiotherapy for esophageal cancer are to be utilized in the
future to verify our current results.
In the present study, we found that the comparison
of AI between biopsy tissues obtained prior to treatment and
following a radiation dose of 10 Gy was clinically significant for
the prediction of chemoradiosensitivity in esophageal squamous cell
carcinoma. Consequently, our findings may contribute to determining
the therapeutic course, resulting in the prevention of severe
adverse events and reduced costs for the predicted non-responders
with esophageal squamous cell carcinoma.
References
|
1
|
Greer SE, Goodney PP, Sutton JE and
Birkmeyer JD: Neoadjuvant chemoradiotherapy for esophageal
carcinoma: A meta-analysis. Surgery. 137:172–177. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Fiorica F, Di Bona D, Schepis F, Licata A,
Shahied L, Venturi A, Falchi AM, Craxì A and Cammà C: Preoperative
chemoradiotherapy for oesophageal cancer: A systematic review and
meta-analysis. Gut. 53:925–930. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Urschel JD and Vasan H: A meta-analysis of
randomized controlled trials that compared neoadjuvant
chemoradiation and surgery to surgery alone for resectable
esophageal cancer. Am J Surg. 185:538–543. 2003. View Article : Google Scholar
|
|
4
|
Tepper J, Krasna MJ, Niedzwiecki D, Hollis
D, Reed CE, Goldberg R, Kiel K, Willett C, Sugarbaker D and Mayer
R: Phase III trial of trimodality therapy with cisplatin,
fluorouracil, radiotherapy, and surgery compared with surgery alone
for esophageal cancer: CALGB 9781. J Clin Oncol. 26:1086–1092.
2008. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Lv J, Cao XF, Zhu B, Ji L, Tao L and Wang
DD: Effect of neoadjuvant chemoradiotherapy on prognosis and
surgery for esophageal carcinoma. World J Gastroenterol.
15:4962–4968. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Theisen J, Krause B, Peschel C, Schmid R,
Geinitz H and Friess H: Early response evaluation and prediction in
neoadjuvant-treated patients with esophageal cancer. World J
Gastrointest Surg. 1:30–37. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Muro K, Ohtsu A, Boku N, Chin K, Oda Y,
Fujii T, Hosokawa K, Yoshida S and Hasebe T: Association of p53
protein expression with responses and survival of patients with
locally advanced esophageal carcinoma treated with
chemoradiotherapy. Jpn J Clin Oncol. 26:65–69. 1996. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Shimoyama S, Konishi T, Kawahara M, Aoki
F, Harada N, Shimizu S, Murakami T and Kaminishi M: Expression and
alteration of p53 and p21(waf1/cip1) influence the sensitivity of
chemoradiation therapy for esophageal cancer.
Hepatogastroenterology. 45:1497–1504. 1998.PubMed/NCBI
|
|
9
|
Kitamura K, Saeki H, Kawaguchi H, Araki K,
Ohno S, Kuwano H, Maehara Y and Sugimachi K: Immunohistochemical
status of the p53 protein and Ki-67 antigen using biopsied
specimens can predict a sensitivity to neoadjuvant therapy in
patients with esophageal cancer. Hepatogastroenterology.
47:419–423. 2000.PubMed/NCBI
|
|
10
|
Shimoji H, Miyazato H, Nakachi A,
Kuniyoshi S, Isa T, Shiraishi M, Muto Y and Toda T: Expression of
p53, bcl-2, and bax as predictors of response to radiotherapy in
esophageal cancer. Dis Esophagus. 13:185–190. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Jego G, Hazoumé A, Seigneuric R and
Garrido C: Targeting heat shock proteins in cancer. Cancer Lett. 13
November;2010.(E-pub ahead of print).
|
|
12
|
Gullo C, Au M, Feng G and Teoh G: The
biology of Ku and its potential oncogenic role in cancer. Biochim
Biophys Acta. 1765:223–234. 2006.PubMed/NCBI
|
|
13
|
Hefferin ML and Tomkinson AE: Mechanism of
DNA double-strand break repair by non-homologous end joining. DNA
Repair (Amst). 4:639–648. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Sohda M, Ishikawa H, Masuda N, Kato H,
Miyazaki T, Nakajima M, Fukuchi M, Manda R, Fukai Y, Sakurai H and
Kuwano H: Pretreatment evaluation of combined HIF-1alpha, p53 and
p21 expression is a useful and sensitive indicator of response to
radiation and chemotherapy in esophageal cancer. Int J Cancer.
110:838–844. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Sobin LH and Wittekind C: TNM
Classification of Malignant Tumours: Sixth edition. Wiley-Liss; New
York, NY: pp. 72–76. 2002
|
|
16
|
Therasse P, Arbuck SG, Eisenhauer EA,
Wanders J, Kaplan RS, Rubinstein L, Verweij J, Van Glabbeke M, van
Oosterom AT, Christian MC and Gwyther SG: New guidelines to
evaluate the response to treatment in solid tumors. J Natl Cancer
Inst. 92:205–216. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Japanese Society for Esophageal Diseases.
Guidelines for the clinical and pathologic studies on carcinoma of
the esophagus, ninth edition: Preface, general principles, part I.
Esophagus. 1:61–88. 2004.
|
|
18
|
Japan Esophageal Society. Japanese
Classification of Esophageal Cancer. 10th ed. Kanehara, Tokyo:
2007
|
|
19
|
Oka K, Suzuki Y and Nakano T: High growth
fraction at 9 grays of radiotherapy is associated with a good
prognosis for patients with cervical squamous cell carcinoma.
Cancer. 89:1526–1531. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Valente G, Orecchia R, Gandolfo S, Arnaudo
M, Ragona R, Kerim S and Palestro G: Can Ki67 immunostaining
predict response to radiotherapy in oral squamous cell carcinoma? J
Clin Pathol. 47:109–112. 1994. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Raju U, Ariga H, Koto M, Lu X, Pickett J,
Valdecanas D, Mason KA and Milas L: Improvement of esophageal
adenocarcinoma cell and xenograft responses to radiation by
targeting cyclin-dependent kinases. Radiother Oncol. 80:185–191.
2006. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Mitsuhashi N, Takahashi T, Sakurai H,
Nozaki M, Akimoto T, Hasegawa M, Saito Y, Matsumoto H, Higuchi K,
Maebayashi K and Niibe H: A radioresistant variant cell line,
NMT-1R, isolated from a radiosensitive rat yolk sac tumour cell
line, NMT-1: differences of early radiation-induced morphological
changes, especially apoptosis. Int J Radiat Biol. 69:329–336. 1996.
View Article : Google Scholar
|
|
23
|
Miyata H, Doki Y, Shiozaki H, Inoue M,
Yano M, Fujiwara Y, Yamamoto H, Nishioka K, Kishi K and Monden M:
CDC25B and p53 are independently implicated in radiation
sensitivity for human esophageal cancers. Clin Cancer Res.
6:4859–4865. 2000.PubMed/NCBI
|
|
24
|
Matsubara H, Kimura M, Sugaya M, Koide Y,
Gunji Y, Takegana K, Asano T, Ochiai T, Isono K, Sakiyama S and
Tagawa M: Expression of wild-type p53 gene confers increased
sensitivity to radiation and chemotherapeutic agents in human
esophageal carcinoma cells. Int J Oncol. 14:1081–1085.
1999.PubMed/NCBI
|
|
25
|
Ito T, Kaneko K, Makino R, Ito H, Konishi
K, Kurahashi T, Kitahara T and Mitamura K: Prognostic value of p53
mutations in patients with locally advanced esophageal carcinoma
treated with definitive chemoradiotherapy. J Gastroenterol.
36:303–311. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Sarbia M, Porschen R, Borchard F,
Horstmann O, Willers R and Gabbert HE: p53 protein expression and
prognosis in squamous cell carcinoma of the esophagus. Cancer.
74:2218–2223. 1994. View Article : Google Scholar : PubMed/NCBI
|