Introduction
In the last decade, two anti-epidermal growth factor
receptor monoclonal antibodies (EGFR mAbs), cetuximab and
panitumumab, were approved for the treatment of EGFR-positive
colorectal cancer (CRC) (1,2). EGFR signals are transduced by
KRAS and follow two signaling pathways, the RAS-RAF-MEK-ERK
and RAS-PI3 kinase-AKT/PKB pathways. Mutations at codons 12 and 13
of the KRAS gene have been identified as a level I
predictive biomarker against the treatment of advanced CRC with
anti-EGFR mAbs according to the College of American Pathologists
(CAP) level of evidence classification; that is, these mutations
have been definitively proven as biomarkers based on evidence from
multiple, statistically robust, published trials, and they are
generally used in patient management (3). BRAF is a serine-threonine kinase
located downstream of KRAS, which is a component of the
RAS-RAF-MEK-ERK signaling pathway (4). A valine to glutamate substitution
mutation at codon 600 (V600E) of the BRAF gene is a hot spot
and is observed in 5–22% of CRCs (4). BRAF has a level IIA CAP
predictive value, which means that extensive biological and
clinical studies have repeatedly shown it to have predictive value
for therapy; however, this remains to be validated in statistically
robust studies (3).
Phosphatidylinositol 3 kinase (PI3K) is composed of a regulatory
and a catalytic subunit (5). The
latter is encoded by the PIK3CA gene. Mutations in
PIK3CA are observed in 15% of CRCs (6); approximately 70% of PIK3CA
mutations are located at exon 9 [a glutamic acid to lysine
substitution at codons 542 (E542K) and 545 (E545K)] and 20% at exon
20 [a histidine to arginine substitution at codon 1047 (H1047R)]
(7). PIK3CA has a level IIB
CAP predictive value, indicating that it has shown promise in
multiple studies; however, sufficient data for its inclusion in
categories I or IIA are lacking (3). Although EGFR is a direct target of
EGFR mAbs, the EGFR expression level does not have any predictive
value in a clinical setting (3).
Glutathione S-transferase II (GSTP) is involved in detoxification
and may be used as a cancer marker (8). Overexpression of GSTP has been
reported to be closely correlated with KRAS mutations; the GSTP
expression level is higher in CRCs with KRAS mutations compared to
wild-type KRAS (9). Expression of
mutant KRAS activates GSTP at a transcriptional level. If this
observation is reproducible in a clinical setting, the presence of
a KRAS mutation may be distinguishable by GSTP immunohistochemistry
(IHC).
One report, analyzing 233 genes, indicated that
there may be differences in as few as 3% of genes between primary
and metastatic sites (10).
Moreover, mutations in the KRAS, BRAF and
PIK3CA genes occur around the adenoma stage (10). In these situations, it is thought
that the routine performance of one genetic test for KRAS
mutations associated with metastatic CRC using DNA obtained from
one organ, either from the primary or a metastatic site, whichever
is preferentially available, is sufficient. However, the
possibility of considerable tumor heterogeneity remains an issue.
Recently, the possibility of acquired or intratumoral mutations of
the KRAS gene was reported (11,12).
Although the number of cases surveyed was small, the frequency of
acquired mutations identified was not negligible. In our study, we
identified 9 cases in which synchronous or metachronous metastasis
was resectable, together with the primary CRC, and determined the
status of target genes, including KRAS, BRAF,
PIK3CA, EGFR and GSTP at each of these sites to determine
the incidence of acquired mutations that may affect treatment with
EGFR mAbs.
Materials and methods
Patient selection
Samples were collected from the primary site, and
from at least one site of distant synchronous or metachronous
metastasis, from 9 patients with colorectal adenocarcinoma whose
tumors were resected at Akita University Hospital (Japan). This
study was approved by the institutional ethics committee for
clinical studies at Akita University, Graduate School of Medicine,
on July 20th, 2010, and each of the patients gave their informed
consent to the procedure.
Direct sequencing
Direct sequencing of codons 12 and 13 of
KRAS, codon 600 of BRAF, and exons 9 and 20 of
PIK3CA was outsourced to SRL Inc. (Tokyo, Japan) or Falco
Biosystems Ltd. (Kyoto, Japan). Briefly, the tumor cell-rich area
of a hematoxylin and eosin-stained section was identified by
microscopy. Tissue was then removed from the same area of a
deparaffinized, unstained section. DNA from sections of that tissue
sample was then isolated using the QIAamp FFPE Tissue kit (QIAGEN
K.K.; Tokyo, Japan) and exon 1 of the KRAS gene, exon 15 of
the BRAF gene, and exons 9 and 20 of the PIK3CA gene
were amplified by polymerase chain reaction (PCR). The PCR products
were visualized using agarose gel electrophoresis with ethidium
bromide staining. PCR DNA fragments were directly sequenced using
an ABI 3130 Genetic Analyzer (Applied Biosystems; Foster City, CA,
USA) according to the manufacturer’s instructions.
Immunohistochemistry
Almost all of the procedures were performed using a
BenchMark XT IHC/ISH Staining Module (Roche Diagnostics K.K; Tokyo,
Japan). Deparaffinized 4-μm specimens were used for IHC along with
anti-human EGFR mouse monoclonal antibody (clone 2-18C9, Dako
Japan; Tokyo, Japan), anti-human KRAS mouse monoclonal antibody
(clone ab55391, Abcam Japan; Tokyo, Japan), and polyclonal rabbit
anti-human GSTP (311-H, Medical and Biological Laboratories Co.,
Ltd.; Nagoya, Japan). Immunopositivity for EGFR was judged as
positive if there were >0.1% positive cells. Immunoreactivities
for KRAS and GSTP were graded as negative (0 to <10% positive
cells), + (≥10 to <30% positive cells), ++ (>30 to <70%
positive cells) and +++ (>70% positive cells). The percentage of
immunopositive cells was calculated by counting at least 400 cancer
cells in contiguous fields with the greatest immunopositivity.
Results
Patient characteristics
A total of 9 patients (3 females and 6 males) were
included in this observational study. The median age was 67 years
(range, 56–75). The patients were diagnosed as having CRC
adenocarcinomas (2 rectal and 7 colon cancers). Three synchronous
and 5 metachronous liver metastases, 2 synchronous and 5
metachronous lung metastases, and 1 synchronous ovarian metastasis
were included. Resection of the primary region and at least one
metastasis site was conducted either simultaneously or
independently (Table I).
 | Table IClinical profiling of 9 mCRC patients
and their biomarker status. |
Table I
Clinical profiling of 9 mCRC patients
and their biomarker status.
| Characteristic | Case 1 | Case 2 | Case 3 | Case 4 | Case 5 | Case 6 | Case 7 | Case 8 | Case 9 |
|---|
| Age | 72 | 66 | 65 | 56 | 67 | 75 | 71 | 72 | 57 |
| Gender | M | M | M | F | M | F | M | M | F |
| Primary | R | A | R | A | A | A | A | T | S |
| Hist | Wel-mod | Mod | Mod>wel | Mod | Mod | Wel | Mod | Wel | Wel>mod |
| Meta | Liver | Liver | Liver | Liver | Liver | Liver | Lung | Liver | Ovary |
| | | Lung | | Lung | | | LN | |
| Occurence | S | S | M | S | S | M | M | M | S |
| | | M | | S | | | M | |
| Interval (D) | - | - | 483 | - | - | 382 | 1652 | 2321 | - |
| | | 1435 | | - | | | 2321 | |
| KRAS | G13D | Wild | Wild | Wild | G12D | Wild | Wild | Wild | Wild |
| G13D | Wild | Wild | Wild | G12D | Wild | Wild | G12V | Wild |
| | | Wild | | G12D | | | G12V | |
| BRAF | Wild | Wild | Wild | Wild | Wild | Wild | L597R | Wild | Wild |
| Wild | Wild | Wild | Wild | Wild | Wild | L597R | Wild | Wild |
| | | Wild | | Wild | | | ND | |
| PIK3CA | Wild | Wild | Wild | Q546E | Wild | Wild | Wild | Wild | Wild |
| Wild | Wild | Wild | Q546E | Wild | Wild | Wild | Wild | Wild |
| | | Wild | | Wild | | | ND | |
| EGFR | (−) | (+) | (+) | (+) | (−) | (−) | (−) | (−) | (+) |
| (−) | (+) | (+) | (+) | (−) | (−) | (+) | (+) | (+) |
| | | (+) | | (−) | | | ND | |
| GSTP | (+++) | (+++) | (+++) | (+++) | (++) | (−) | (+) | (−) | (−) |
| (++) | (++) | (++) | (+++) | (+++) | (−) | ND | (−) | (−) |
| | | ND | | ND | | | ND | |
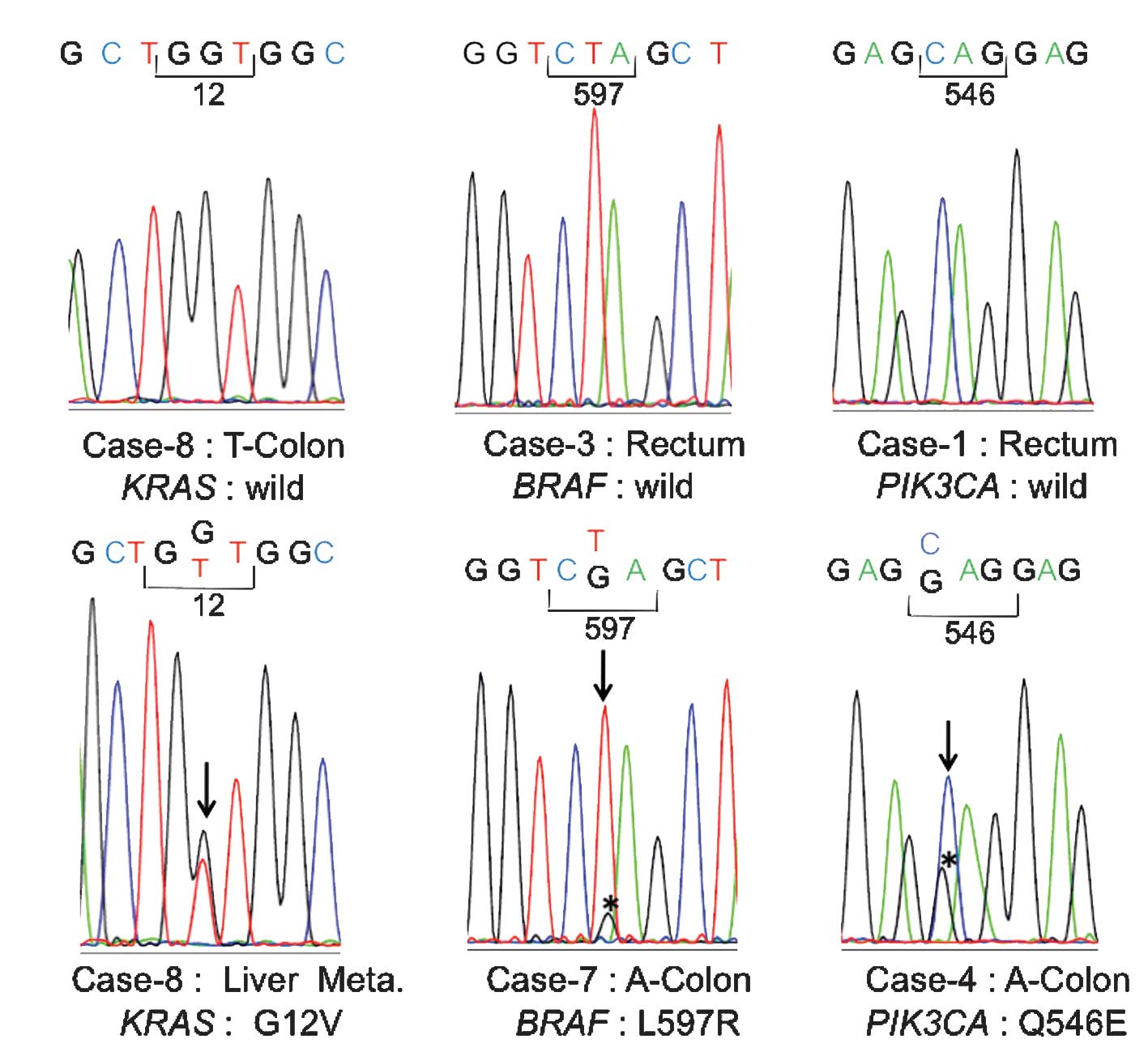
Sequence analyses of the KRAS, BRAF and
PIK3CA genes
Regarding KRAS mutations, a glycine to
aspartic acid mutation at codon 12 (G12D) was observed in the
primary region of case 5, and a glycine to aspartic acid mutation
at codon 13 (G13D) was observed in the primary region of case 1. In
the remaining cases, no mutations were observed in the primary
regions (Table I, Fig. 1A). The KRAS mutation
frequency in the primary region was thus estimated to be 22.2%
(2/9). At the metastatic sites, a G12D mutation was observed in
both the lung and liver metastatic sites of case 5, and a G13D
mutation was observed in the liver metastatic site of case 1. In
case 8, a KRAS mutation involving a glycine to valine
substitution at codon 12 (G12V) was observed in the liver
metastatic site (Fig. 1B). In the
remaining cases, no mutations were observed in the metastatic
regions. The mutation frequency of KRAS at each metastatic
site was thus estimated to be 27.3% (3/11).
No BRAF mutations were observed at exon
15 in the primary regions of all cases other than for case 7
(Fig. 1C)
In case 7, a leucine to arginine mutation was
observed at codon 597 (L597R) (Fig.
1D). This L597R mutation was also observed at the site of lung
metastasis in case 7. No other mutations were observed at any of
the remaining metastatic sites. According to the genomic
information found in the Catalogue of Somatic Mutations of Cancer
(COSMIC), released by the Sanger Institute, L597R was confirmed as
a somatic variant (http://www.sanger.ac.uk/perl/genetics/CGP/cosmic?action=sample&id=749760).
As for PIK3CA, no mutations were observed at
exons 9 and 20 in the primary region of all cases with the
exception of case 4 (Fig. 1E). In
case 4, a glutamine to glutamic acid mutation was observed at codon
546 (Q546E) at exon 9 (Fig. 1F).
This Q546E mutation was also observed at the site of liver
metastasis in case 4. No mutations were observed at the remaining
metastatic sites. Q546E was confirmed as a somatic variant by
COSMIC (http://www.sanger.ac.uk/perl/genetics/CGP/cosmic?action=mut_summary&id=6147).
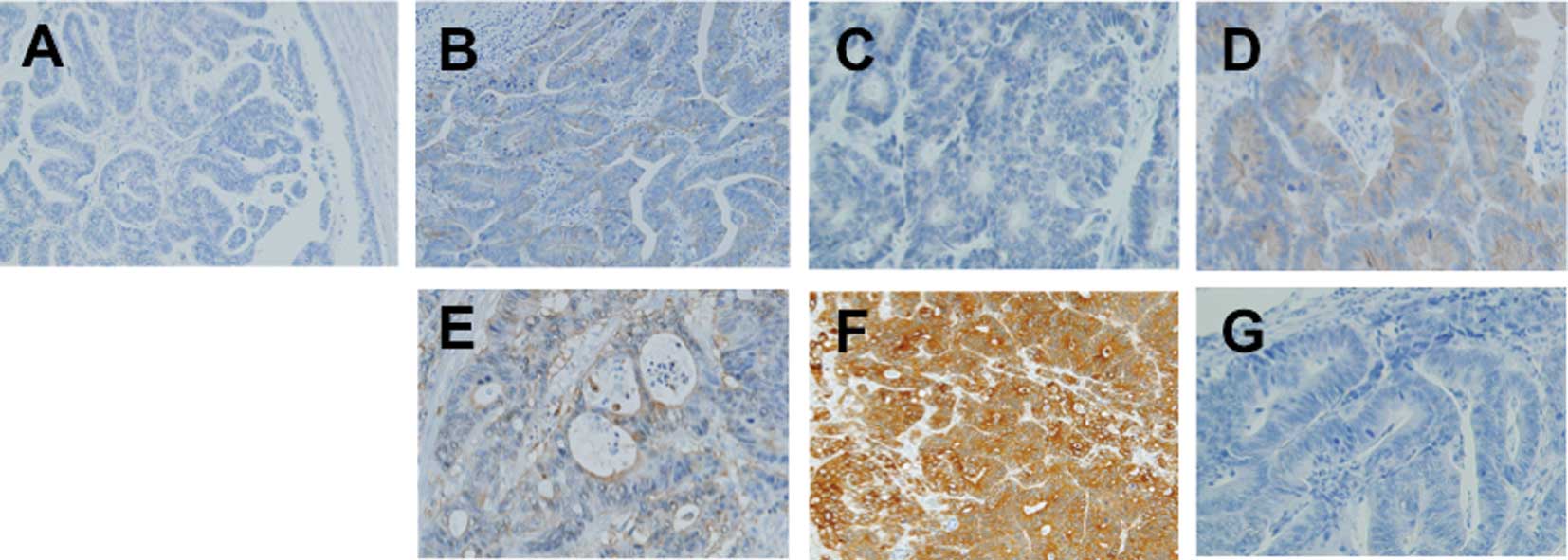
Immunohistochemical analyses of EGFR,
KRAS and GSTP
Immunopositivity for EGFR was observed at the
primary site in 4 out of the 9 cases (cases 2, 3, 4 and 9)
(Table I). A corresponding
immunopositivity was observed at the metastatic sites in these 4
cases. However, a different immunopositivity was observed for cases
7 and 8, where the immunoreacitivity for EGFR was negative at the
primary site but positive at the metastatic site (Fig. 2A and B). No immunopositivity was
observed at the primary or metastatic sites in the remaining
cases.
Immunoreactivity for KRAS is apparently
not dependent on the mutational status of KRAS (Table I, Fig.
2C and D)
Moreover, a correlation between the
immunoreactivities or mutational status was not observed between
KRAS and GSTP in this study (Fig. 2E-G). Therefore, we were unable to
diagnose the mutational status of KRAS by GSTP IHC in a
clinical setting.
Case presentation
In this observational study, a difference in the
KRAS gene status between the primary and metastatic sites
was observed in 1 (case 8) out of 9 cases (11.1%). This was
independently confirmed by a separate analysis. Furthermore, the
same KRAS mutation was detected in the resected mediastinal
lymph node in case 8. Differences in immunopositivity for EGFR were
observed in 2 (cases 7 and 8) out of 9 cases (22.2%). Case 7 was a
71-year-old male with ascending colon cancer. Following the primary
resection, a 5-fluorouracil (5-FU) regimen (RPMI regimen) was
administered for 6 months as adjuvant chemotherapy but 1,652 days
following resection of the primary site, metastasis was evident in
one lung and the site was resected (13). Modified leucovorin, fluorouracil and
oxaliplatin (mFOLFOX6) was then administered as adjuvant
chemotherapy for 180 days following resection until completion
(April, 2011). Case 8 was a 72-year-old male with transverse colon
cancer. Following primary resection, adjuvant chemotherapy was
similarly administered for 6 months. However, 2,321 days after the
primary resection, metastasis was detected at one site in the liver
and in one mediastinal lymph node. The two sites were resected and
mFOLFOX6 initiated as adjuvant chemotherapy (14). However, on day 159, mFOLFOX6 was
terminated due to lung and abdominal lymph node metastases. A
folinic acid-fluorouracil-irinotecan (FOLFIRI) regimen was then
initiated and continued for 232 days up to the time of writing
(15).
Discussion
In this study, we identified a possibility that
acquired or intratumoral mutations may occur in the EGFR signaling
pathway during CRC progression. Regarding KRAS, mutations in
codons 12 and 13 were observed in 2 out of 9 cases at the primary
site, and an acquired mutation was found in 1 case at a distal
metastatic site. In previous reports, the mutation frequency of
KRAS at codons 12 and 13 has ranged from 27 to 53% in CRC,
which is similar to our finding (30%). The mutation frequencies of
BRAF (V600E) and PIK3CA (exons 9 and 12) have been
reported as 5–22% and 15%, respectively, in CRC. In our study, no
oncogenic mutations of BRAF or PIK3CA were observed
at either the primary or the metastatic sites. Differences in EGFR
immunoreactivity were observed between the primary and metastatic
sites in two instances, cases 7 and 8. In these two cases, the
duration between the date of resection of the primary site and the
date of metastatic recurrence was much longer (1,652 and 2,321
days, respectively) than that for the other cases (7 synchronous
and 7 metachronous metastatic sites). In the remaining cases, the
duration between the date of resection of the primary site and the
date of onset of metastatic recurrence ranged from 217 to 952 days
(median, 395). Since protein is easily degraded, the IHC analysis
of EGFR may be affected by long-term storage. Therefore, the
failure to detect immunoreactivity at the primary sites in cases 7
and 8 may be due to protein degradation during long-term storage.
However, the direct sequencing of KRAS was successfully
performed using DNA obtained from the archived specimens of the
primary sites for these cases (Fig.
1). DNA is more stable than protein over longer periods;
therefore, the quality of DNA in this study was sufficient for
direct sequencing. In case 8, the possibility of an acquired or
intratumoral mutation was suspected. The overall incidence of
acquired or intratumoral mutations of KRAS was approximately
10% in this study, which is nearly identical to that of previous
reports. Bouchahda et al reported acquired KRAS
mutations (G12D and G13D) in 2 out of 13 cases (15.4%) (11). Richman et al reported
intratumoral KRAS mutations at codons 12 and 13 in 5 out of
68 cases (7.4%) and an intratumoral BRAF mutation (V600E) in
2 cases (2.9%). Thus, in total, mutations in the EGFR pathway were
identified in 7 out of 68 cases (10.3%) in their study (12). Although only 9 cases were analyzed
in our study, each case had at least one resectable metastatic site
and the total number of sites (combining primary and metastatic
sites) was 18. Thus, it may be better to report an acquired
mutation rate of approximately 11.1% (2/18). In conclusion, when
metastatic recurrence occurs after a long interval, it is likely
that acquired KRAS mutations may be identified.
Acknowledgements
This study was supported by the Ministry of Health,
Labour, and Welfare.
References
|
1
|
Vincenzi B, Zoccoli A, Pantano F, Venditti
O and Galluzzo S: Cetuximab: from bench to bedside. Curr Cancer
Drug Targets. 10:80–95. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Giusti RM, Cohen MH, Keegan P and Pazdur
R: FDA review of a panitumumab (Vectibix) clinical trial for
firat-line treatment of metastatic colorectal cancer. Oncologist.
14:284–290. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Ross JS, Torres-Mora J, Wagle N, Jennings
TA and Jones DM: Biomarker-based prediction of response to therapy
for colorectal cancer. Am J Clin Pathol. 134:478–490. 2010.
View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Garnett MJ and Marais R: Guilty as
charged: B-RAF is a human oncogene. Cancer Cell. 6:313–319. 2004.
View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Garcia Z, Kumar A, Marques M, Cortes I and
Carrera AC: Phosphoinositide 3-kinase controls early and late
events in mammalian cell division. EMBO J. 25:655–661. 2006.
View Article : Google Scholar : PubMed/NCBI
|
|
6
|
De Roock W, Claes B, Bernasconi D, et al:
Effects of KRAS, BRAF, NRAS, and PIK3CA mutations on the efficacy
of cetuximab plus chemotherapy in chemotherapy-refractory
metastatic colorectal cancer: a retrospective consortium analysis.
Lancet Oncol. 11:753–762. 2010.PubMed/NCBI
|
|
7
|
Samuels Y, Diaz LA Jr, Schmidt-Kittler O,
et al: Mutant PIK3CA promotes cell growth and invasion of human
cancer cells. Cancer Cell. 7:561–573. 2005. View Article : Google Scholar
|
|
8
|
Aliya S, Reddanna P and Thyagaraju K: Does
glutathione S-transferase Pi (GST-Pi) a marker protein for cancer?
Mol Cell Biochem. 253:319–327. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Miyanishi K, Takayama T, Ohi M, et al:
Glutathione S-transferase-pi overexpression is closely associated
with K-ras mutation during human colon carcinogenesis.
Gastroenterology. 121:865–874. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Jones S, Chen WD, Parmigiani G, et al:
Comparative lesion sequencing provides insights into tumor
evolution. Proc Natl Acad Sci USA. 105:4283–4288. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Bouchahda M, Karaboué A, Saffroy R, et al:
Acquired KRAS mutations during progression of colorectal cancer
metastases: possible implications for therapy and prognosis. Cancer
Chemother Pharmacol. 66:605–609. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Richman SD, Chambers P, Seymour MT, Daly
C, Grant S, Hemmings G and Quirke P: Intra-tumoral heterogeneity of
KRAS and BRAF mutation status in patients with advanced colorectal
cancer (aCRC) and cost-effectiveness of multiple sample testing.
Anal Cell Pathol. 34:61–66. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Haller DG, Catalano PJ, Macdonald JS,
O’Rourke MA, Frontiera MS, Jackson DV and Mayer RJ: Phase III study
of fluorouracil, leucovorin, and levamisole in high-risk stage II
and III colon cancer: final report of Intergroup 0089. J Clin
Oncol. 23:8671–8678. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
André T, Boni C, Navarro M, et al:
Improved overall survival with oxaliplatin, fluorouracil, and
leucovorin as adjuvant treatment in stage II or III colon cancer in
the MOSAIC trial. J Clin Oncol. 27:3109–3116. 2009.PubMed/NCBI
|
|
15
|
Tournigand C, André T, Achille E, et al:
FOLFIRI followed by FOLFOX6 or the reverse sequence in advanced
colorectal cancer: a randomized GERCOR Study. J Clin Oncol.
22:229–237. 2004. View Article : Google Scholar : PubMed/NCBI
|