Introduction
Circulating tumor cells (CTCs) are present in the
blood of patients with malignant tumors and are strongly correlated
with the prognosis of patients. CTCs are formed when certain tumor
cells escape from the solid tumor cell nests and gain access to the
blood circulation. Thus, it is likely that any touching or crushing
of the tumor during surgery may initiate this process. The issue of
whether surgical manipulation of pulmonary lobectomy promotes blood
micrometastasis, and whether different sequences of pulmonary
artery (PA) and vein (PV) ligations have different effects on blood
micrometastasis of pulmonary carcinoma remain controversial. Kurusu
et al observed the mRNA expression of carcino-embryonic
antigen (CEA) in the blood at early, middle and late periods during
surgery and concluded that surgery could promote blood
micrometastasis (1). Conversely,
Refaely concluded that different sequences of PA and PV ligations
bore no correlation with the prognosis of the patients (2). However, in the previous studies, the
comparisons of related gene expression were made between those in
the pulmonary venous blood during surgery and those in the
peripheral blood before and after surgery, and thus certain errors
may have been caused due to different blood samples. Therefore, to
clarify the investigation of whether different sequences of PA and
PV ligations have different effects on blood micrometastasis,
errors caused by different blood samples should be avoided by
making a comparison between gene expression in pulmonary venous
blood at early and late periods during surgery (3). Thus, to perform a rigorous comparison,
blood samples at early and late periods during surgery should both
be drawn from the PV.
In this study, we aimed to assess whether the
process of surgical manipulation itself affects blood
micrometastasis. We randomly divided 30 patients suffering from
non-small cell lung cancer (NSCLC) into PA-first and PV-first
groups. Fluorescent quantitative-RT-PCR (FQ-RT-PCR) was used to
detect the mRNA expression of CK19 and CD44v6 in the pulmonary
venous blood at early and late periods during each operation.
Materials and methods
Patients
From January 2009 to January 2010, a total of 30
NSCLC patients underwent lobectomy for NSCLC in the thoracic
surgery department of Shandong Tumor Hospital, China. The
post-operative pathologic tumor-node-metastases (TNM) stage was
determined according to the grading criteria of UICC. The diagnosis
of lung cancer was histologically confirmed on each resected
specimen where the tumor size was measured. Eligible patients had
no history of previous anticancer therapy (including radiotherapy
and chemotherapy) or other malignancy. The 10 cases in the control
group were healthy volunteers with no history of malignancy. The
study was approved by the ethics committee of Shandong Cancer
Hospital and Institute, Jinan, China. Written informed patient
consent was obtained from the patient’s family with warrant of
attorney.
Blood samples
All NSCLC patients were randomly divided into two
groups: PV-first (15 cases) and PA-first (15 cases). For the
PV-first group, the PV was separated following anesthesia and
opening of the chest, 10 ml blood was drawn from the proximal part
and then the vein was immediately ligated (but not cut off) at the
distal part. Then, routine operative procedures were performed.
After 30 min, another 10 ml blood was drawn from the proximal part
of the PV (as distant from the ligated spot as possible) and then
the vein was cut off. For the PA-first group, the PV was separated
following anesthesia and opening of the chest, 10 ml blood was
drawn from the proximal part and soon afterwards the ligation of
the PA was carried out. After 20–45 min, 10 ml blood was drawn from
the proximal part of the vein. All patients underwent routine
mediastinal lymphadenectomy following pulmonary lobectomy and
recovered well after the operation. Peripheral vein blood samples
were drawn from the controls. All blood samples were added into
EDTA anticoagulation tubes and blood monocytes were obtained by
Ficoll density gradient centrifugation, rinsing with PBS and
centrifuging twice. Then, they were dissolved by adding 1 ml TRIzol
reagent for the extraction of total RNAs.
Extraction of total RNAs
Total RNAs were extracted by adding 0.25 ml TRIzol™
reagent to Ficoll-isolated cells, mixing thoroughly and maintaing
at room temperature for 5 min. Then, the homogenate was transferred
into a 1.5 ml EP tube to which 0.05 ml choloroform was added,
shaken vigorously for 15 sec and then maintained at room
temperature for 2–3 min. This was centrifuged at 10,000 × g for 15
min at 2–8°C. The upper aqueous phase in the EP tube was
transferred into a fresh tube, to which 0.125 ml isopropanol was
added, and then maintained at room temperature for 10 min. This was
centrifuged at 10,000 × g for 10 min at 2–8°C. Supernatants were
discarded. RNA precipitate was washed twice with 0.5 ml 75%
ethanol, centrifuged at 7,500 × g for 5 min at 2–8°C, dehumidified
in air and then dissolved by adding RNase-free H2O. The
absorbance of 260 nm (A260) was measured by nucleoprotein
quantitative analyzer and the ratio of A260/A280 was used to
measure RNA purity (the ratios were 1.8/2.0 in this study). All the
samples were preserved at −80°C.
Real-time PCR
RT reaction was carried out using PrimeScript™ RT
kit (Perfect Real Time, Applied Biosystems, Carlsbad, CA, USA). The
reaction system (10 μl) contained 2 μl 5X PrimeScript
Buffer, 0.5 μl PrimeScript RT Enzyme Mix I, 0.5 μl
Oligo dT Primer (50 μM), 0.5 μl random 6 primer (100
μM) and 1 μg RNA. The reaction conditions were 37°C
for 15 min, followed by 85°C for 5 sec. Subsequently, cDNA samples
were preserved in a −80°C refrigerator.
SYBR® Premix Ex Taq™ (Perfect Real Time)
kit was used for real-time PCR. A quantitative PCR system (25
μl) contained 12.5 μl 2X SYBR Premix Ex Taq, 0.5
μl forward primer (10 μM), 0.5 μl reverse
primer (10 μM) and 100 ng cDNA. The primer sequences of
CD44v6 were 5′-AGCAACCCTACTGATGATGACG-3 (forward) and
5′-GGAGTCTTCTCTGGGTGTTTGG-3 (reverse), and those of CK19 were
5′-CTTCCGAACCAAGTTTGAGACG-3 (forward) and
5′-CCTCAGCGTACTGATTTCCTCCT-3 (reverse). An ABI PRISM 7700 system
was used for PCR. The amplification conditions were a cycle of
pre-denaturation at 95°C for 30 sec, 40 cycles of 95°C for 5 sec
and 60°C for 30 sec. β-actin was used as an internal standard. All
the samples were repeated three times and the values of ΔCt were
calculated. The Ct value was calculated by determining the point at
which the fluorescence exceeded an arbitrary threshold limit. The
value of ΔCt was obtained from the formula: Ct = Ct (target gene) −
Ct (β-actin). A higher ΔCt value indicated a lower target gene
content and gene expression was lower with more amplification.
Conversely, a lower ΔCt value indicated a greater target gene
content and gene expression was higher with less amplification.
Statistical analysis
The Ct data of the genes were analyzed by SDS
software (ABI). All the data were analyzed by SPSS 11.5 software.
Student’s t test was used. Differences were considered significant
when P<0.05.
Results
mRNA expression of CD44v6 and CK19
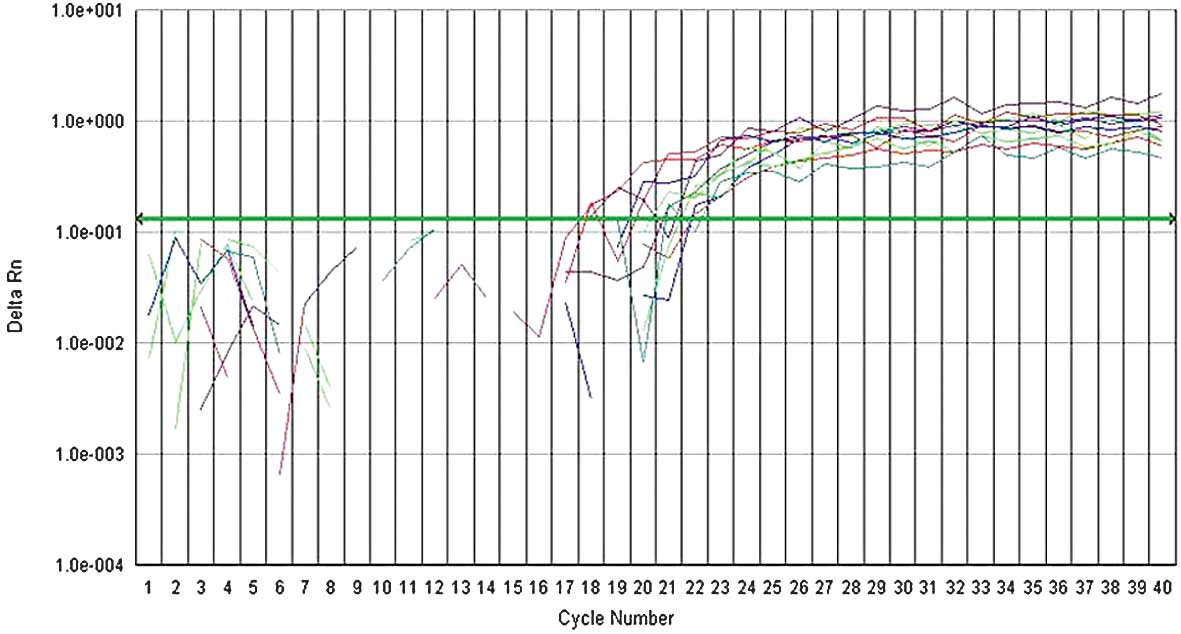
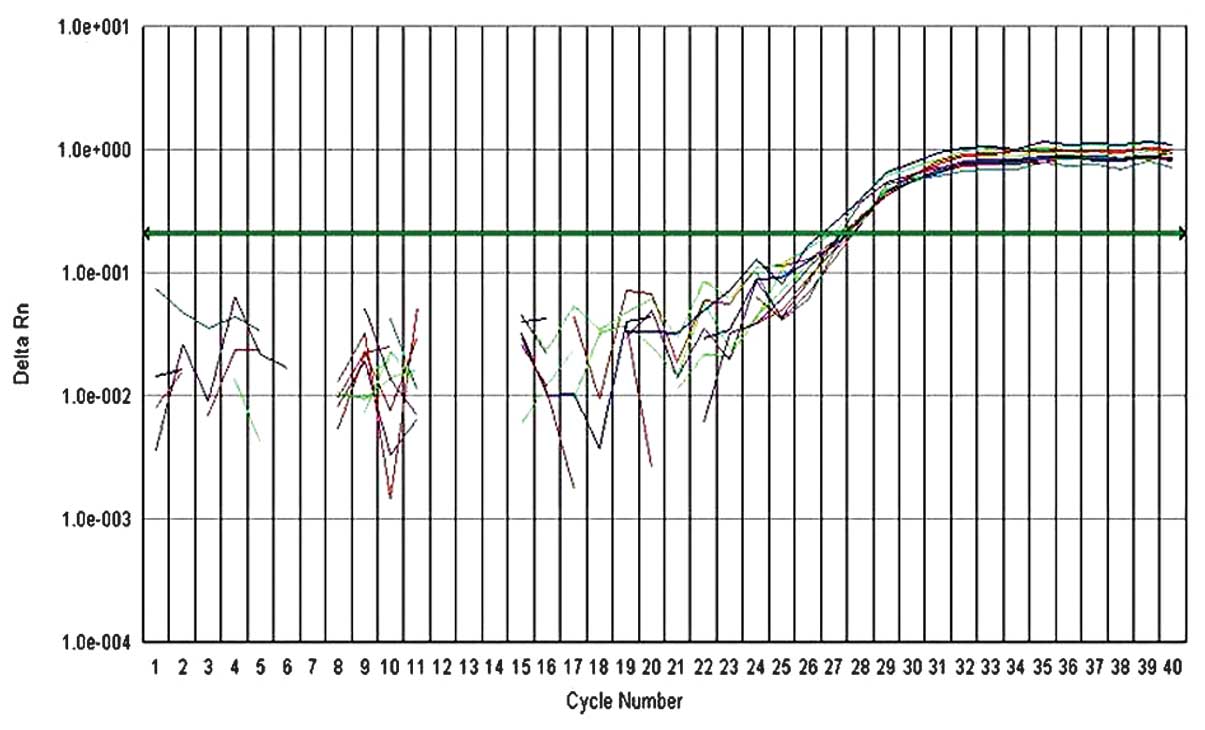
Fluorescent quantitative PCR was used to detect the
mRNA expression of CK19 and CD44v6 in the pulmonary venous blood
before and after venous ligation. For each reaction tube, the
fluorescence signal of the reporter dye (FAM) was divided by the
fluorescence signal of the passive reference dye (ROX), to obtain a
ratio defined as the normalized reporter signal (Rn). DRn
represents the normalized reporter signal (Rn) minus the baseline
signal. The results indicated that ΔCt values of CD44v6 and CK19 of
NSCLC groups at the early period during surgery were 7.83±1.70 vs.
10.76±2.74, respectively, while those of the control group were
9.17±1.04 vs. 12.76±2.36. The mRNA expression of CD44v6 and CK19 in
NSCLC groups was significantly higher than that of the control
group (P<0.05) (Table I,
Figs. 1–3).
 | Table I.Differences in mRNA expression between
CD44v6 and CK19 in pulmonary venous blood of NSCLC groups and those
in the control group. |
Table I.
Differences in mRNA expression between
CD44v6 and CK19 in pulmonary venous blood of NSCLC groups and those
in the control group.
| Group | Number of cases | CD44V6 | CK19 |
|---|
| NSCLC | 30 | 7.83±1.70 | 10.76±2.74 |
| Control | 10 | 9.17±1.04 | 12.76±2.36 |
| P-value | | 0.006 | 0.039 |
Patient characteristics and the
expression of CD44v6 and CK19
There was a clear difference in CD44v6 mRNA level
between squamous cell carcinoma and adenocarcinoma at late periods
during surgery (7.95±1.81 vs. 5.81±2.23; P=0.008). No significant
correlation was identified between the expression of CD44v6 and
CK19 and any other clinicopathological characteristics, at early
and late periods during surgery (Table
II).
 | Table II.Patient characteristics and the
expression of CD44v6 and CK19. |
Table II.
Patient characteristics and the
expression of CD44v6 and CK19.
| | Early period
| Late period
|
|---|
| Patient
characteristics | No. | CD44v6 | P-value | CK19 | P-value | CD44v6 | P-value | CK19 | P-value |
|---|
| Gender | | | 0.875 | | 0.266 | | 0.552 | | 0.271 |
| Male | 14 | 7.78±2.13 | | 11.43±3.04 | | 7.08±2.46 | | 10.41±3.52 | |
| Female | 16 | 7.89±1.93 | | 10.17±3.02 | | 6.57±2.16 | | 8.90±3.81 | |
| Smoking | | | 0.890 | | 0.293 | | 0.241 | | 0.133 |
| Yes | 20 | 7.86±2.28 | | 9.83±3.56 | | 6.41±1.97 | | 8.88±3.66 | |
| Non | 10 | 7.77±1.40 | | 11.22±2.73 | | 7.61±2.77 | | 11.04±3.49 | |
| Histology | | | 0.652 | | 0.377 | | 0.008 | | 0.242 |
| Squamous cell
carcinoma | 14 | 8.01±2.26 | | 10.29±2.46 | | 7.95±1.81 | | 8.85±3.60 | |
| Adenocarcinoma | 16 | 7.67±1.82 | | 11.29±3.62 | | 5.81±2.23 | | 10.46±3.75 | |
| Site of primary
tumor | | | 0.965 | | 0.142 | | 0.082 | | 0.133 |
| Hilar | 11 | 7.85±2.02 | | 9.67±3.24 | | 5.86±2.14 | | 8.26±3.96 | |
| Peripheral | 19 | 7.82±2.05 | | 11.38±2.82 | | 7.36±2.24 | | 10.38±3.40 | |
| Pathological
stage | | | 0.331 | | 0.496 | | 0.059 | | 0.159 |
| I | 9 | 8.47±2.06 | | 11.51±3.25 | | 7.96±1.43 | | 10.59±3.67 | |
| II | 13 | 7.89±2.05 | | 10.00±2.92 | | 6.91±2.37 | | 10.23±2.93 | |
| IIIA | 8 | 7.01±1.82 | | 11.14±3.12 | | 5.36±2.17 | | 7.47±4.38 | |
Effects of different ligation sequences
on the expression of CD44v6 and CK19
In the PA-first group, ΔCt values of CD44v6 and CK19
at early vs. late periods during surgery were 7.92±1.97 vs.
5.67±2.11 (P= 0.008) and 11.21±3.14 vs. 8.60±4.02 (P= 0.05),
respectively. Both CD44v6 and CK19 values in the late period were
significantly higher than those in the early period (P≤0.05). In
the PV-first group, ΔCt values of CD44v6 and CK19 before and after
ligation were 7.74±2.10 vs. 7.95±1.91, and 10.30±2.98 vs.
10.60±3.15, and ΔCt values of CD44v6 and CK19 before vs. after
ligation were similar, exhibiting no statistically significant
differences (P>0.05; Table III).
The results indicated that mRNA expression of CD44v6 and CK19 in
the PA-first group in the late period during surgery was
significantly higher than that in the early period.
 | Table III.Effects of different sequences of
ligation during surgery on the mRNA expression of CD44v6 and
CK19. |
Table III.
Effects of different sequences of
ligation during surgery on the mRNA expression of CD44v6 and
CK19.
| | CD44v6
| CK19
|
|---|
| Group | Number of cases | Early period | Late period | P-value | Early period | Late period | P-value |
|---|
| PA-first | 15 | 7.92±1.97 | 5.67±2.11 | 0.008 | 11.21±3.14 | 8.60±4.02 | 0.050 |
| PV-first | 15 | 7.95±1.91 | 7.74±2.10 | 0.558 | 10.60±3.15 | 10.30±2.98 | 0.532 |
Discussion
The basic principles for tumor surgery advise that
all procedures should be performed gently and any touching or
crushing of the tumor should be minimized to reduce (or even avoid)
the possibility that tumor cells may escape from the solid tumor
cell nests and enter the circulation, thus causing blood
micrometastasis. According to Turnbull et al and Hayashi
et al(5,6), the application of a non-contact
technique in colon carcinoma operations could reduce the formation
of CTCs and improve the survival rate of patients. It was highly
recommended that surgeons treat the tumor gently and avoid turning
over and squeezing the mass as much as possible.
There has been emerging evidence to suggest that
CK19 mRNA detection is strongly associated with the presence of
lung cancer metastases or recurrence, particularly after surgery
(6). CD44v6, the v6 variant of
CD44, is mainly expressed in a subset of adenocarcinomas and the
expression of adhesion molecule CD44v6 could well reflect the
invasiveness and adhesiveness of malignant tumor cells. In this
study, NSCLC patients were randomly divided into PA-first and
PV-first groups, and blood samples from the early and late periods
during surgery were both drawn from the vein in order to make an
objective comparison between the effect of either PA or PV first.
According to traditional theories, it is clearly required that
ligation of the PV should be performed prior to that of the PA
during lobectomy, to prevent the occurrence of CTCs entering the
systemic circulation via pulmonary venous blood. No significant
differences were identified between the expression of CD44v6 and
CK19 in PV-first group at early and late periods during surgery,
while significant differences were revealed in the PA-first group
with a higher expression of CD44v6 and CK19 in the early period. It
suggested that the operative procedures may play a promoting role
in CTCs shedding off from the primary tumor and ingressing into the
pulmonary venous blood, and that ligation of the PV first during
surgery may help prevent the dissemination of CTCs. Ge et al
detected the pre-, intra- and post-operative mRNA expression of
CK19/CEA in peripheral venous blood of 23 NSCLC patients using
fluorescent quantitative PCR (7).
All patients were divided into either PV-first or PA-first groups
at random. Results revealed that the intraoperative mRNA expression
of CK19 was significantly higher than the pre- or post-operative
expression (P<0.05); the highest mRNA expression of CEA was
identified after surgery (P<0.05) and the ratio of CK19/CEA in
the PA-first group was higher than that in the PV-first group (but
without statistical significance). Yamashita also revealed that
video-assisted thoracoscopic surgery (VATS) lobectomy was
associated with a higher risk of seeding of tumor cells into the
circulation during operation (8).
Based on these results, it appears that surgical manipulation is
capable of promoting the release of tumor cells into the
bloodstream, and ligation of the PV prior to ligation of the PA may
partly prevent such release during surgery.
Although numerous studies appear to support the
opinion that the PV should be ligated prior to the PA during
surgical intervention and that this order of vessel ligation may
improve the prognosis of patients with NSCLC, there are still
various opinions. According to Refaely et al, different
sequences of PA and vein ligations bore no correlation with tumor
recurrence and prognosis (2). In
the study, a total of 279 NSCLC patients were randomly divided into
PV-first (133 patients, 48%) and PA-first (146 patients, 52%)
groups. The follow-up results revealed that the total recurrence
rates in the two groups were similar and multivariate analysis
(controlling for the effect of the performing surgeon) revealed
that sequence of vessel interruption was not a risk factor. The
results revealed that the sequence of vessel interruption during
lobectomy did not play a role in tumor recurrence.
It is conceivable that most of the cancer cells shed
into the blood stream during surgery are ultimately likely be
destroyed by natural defense mechanisms, and extremely few of the
tumor cells succeed in establishing secondary tumors. As the
content of tumor cells in the blood circulation was extremely low,
the sensitivity and specificity of detection is commonly required
so that even one tumor cell can be detected in
105–107 cells. At present, the detection
methods for tumor micrometastasis include immunohistochemistry,
flow cytometry and RT-PCR, among which RT-PCR has been well
accepted by virtue of its high sensitivity and specificity in
detecting one tumor cell among 105–107 cells
(9,10).
Numerous studies confirmed that the detection of
CTCs in peripheral blood was associated with poor prognosis of the
patient. Using RT-PCR, Yamashita (11) analyzed CEA mRNA expression in
peripheral blood from 103 patients with NSCLC at the time of
diagnosis, prior to surgery, and 2–3 weeks later, following
surgery. The results revealed that patients with high mRNA
expression of CEA in the pre-operative blood samples had a poor
survival rate when compared with those without CEA mRNA expression.
Similarly, Yoon et al (12)
demonstrated that expression of CTCs in pulmonary peripheral blood
was correlated with poor prognosis of the patient.
In this study, both CK19 and CD44v6 were used as
markers to monitor the fluctuation in CTCs of patients. Whether
micrometastasized cells in the blood of malignant tumor patients
leads to the formation of metastatic foci depends on the
invasiveness and adhesiveness of micrometastasized cells. CD44v6 is
mainly expressed in a subset of adenocarcinomas and may be a useful
marker for tumor screening. Studies demonstrated that the
expression of adhesion molecule CD44v6 may reflect the invasiveness
and adhesiveness of malignant tumor cells (13,14).
Thus, the expression of CD44v6 in pulmonary venous blood was
detected in this study, and the results revealed that the level of
CD44v6 was closer to the experimental expectation than that of
CK19. The expression of CD44v6 may be a good indicator of CTCs.
However, this requires further investigation.
Our results suggested that ligation of the PV should
be performed first during lobectomy. It was demonstrated that
surgical manipulation itself may stimulate the occurrence of blood
micrometastasis. Thus, ligation of the PV first during surgery may
help to prevent blood micrometastasis. To clarify the clinical
significance of different sequences of pulmonary vessel
interruption, a prospective study with randomized selection of the
method for each patient and with long-term follow-up should be
conducted.
Acknowledgements
This study was supported by the
Natural Science Foundation of Shandong (ZR2010HM067, ZR2011HM077)
and the Provincial Science and Technology Foundation of Shandong
(2011GGH21819).
References
|
1.
|
Kurusu Y, Yamashita J, Hayashi N, Mita S,
Fujino N and Ogawa M: The sequence of vessel ligation affects tumor
release into the circulation. J Thorac Cardiovasc Surg.
116:107–113. 1998. View Article : Google Scholar : PubMed/NCBI
|
|
2.
|
Refaely Y, Sadetzki S, Chetrit A, Simansky
DA, Paley M, Modan B and Yellin A: The sequence of vessel
interruption during lobectomy for non-small cell lung cancer: is it
indeed important? J Thorac Cardiovasc Surg. 125:1313–1320. 2003.
View Article : Google Scholar : PubMed/NCBI
|
|
3.
|
Okumura Y, Tanaka F, Yoneda K, Hashimoto
M, Takuwa T, Kondo N and Hasegawa S: Circulating tumor cells in
pulmonary venous blood of primary lung cancer patients. Ann Thorac
Surg. 87:1669–1675. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
4.
|
Peck K, Sher YP, Shih JY, Roffler SR, Wu
CW and Yang PC: Detection and quantitation of circulating cancer
cells in the peripheral blood of lung cancer patients. Cancer Res.
58:2761–2765. 1998.PubMed/NCBI
|
|
5.
|
Turnbull RB Jr, Kyle K, Watson FR, Watson
FR and Spratt J: Cancer of the colon: the influence of the no-touch
isolation technic on survival rates. Ann Surg. 166:420–427. 1967.
View Article : Google Scholar : PubMed/NCBI
|
|
6.
|
Hayashi N, Egami H, Kai M, Kurusu Y,
Takano S and Ogawa M: No-touch isolation technique reduces
intraoperative shedding of tumor cells into the portal vein during
resection of colorectal cancer. Surgery. 125:369–374. 1999.
View Article : Google Scholar
|
|
7.
|
Ge MJ, Shi D, Wu QC, Wang M and Li LB:
Observation of circulating tumour cells in patients with non-small
cell lung cancer by real-time fluorescent quantitative reverse
transcriptasepolymerase chain reaction in perioperative period. J
Cancer Res Clin Oncol. 132:248–256. 2006.
|
|
8.
|
Yamashita JI, Kurusu Y, Fujino N, Saisyoji
T and Ogawa M: Detection of circulating tumor cells in patients
with non-small cell lung cancer undergoing lobectomy by
video-assisted thoracic surgery: a potential hazard for
intraoperative hematogenous tumor cell dissemination. J Thorac
Cardiovasc Surg. 119:899–905. 2000. View Article : Google Scholar
|
|
9.
|
Sawabata N, Okumura M, Utsumi T, Inoue M,
Shiono H, Minami M, Nishida T and Sawa Y: Circulating tumor cells
in peripheral blood caused by surgical manipulation of
non-small-cell lung cancer: pilot study using an immunocytology
method. Gen Thorac Cardiovasc Surg. 55:189–192. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
10.
|
Tanaka F, Yoneda K, Kondo N, Hashimoto M,
Takuwa T, Matsumoto S, Okumura Y, Rahman S, Tsubota N, Tsujimura T,
Kuribayashi K, et al: Circulating tumor cell as a diagnostic marker
in primary lung cancer. Clin Cancer Res. 15:6980–6986. 2009.
View Article : Google Scholar : PubMed/NCBI
|
|
11.
|
Yamashita J, Matsuo A, Kurusu Y, Saishoji
T, Hayashi N and Ogawa M: Preoperative evidence of circulating
tumor cells by means of reverse transcriptase-polymerase chain
reaction for carcinoembryonic antigen messenger RNA is an
independent predictor of survival in non-small cell lung cancer: a
prospective study. J Thorac Cardiovasc Surg. 124:299–305. 2002.
View Article : Google Scholar
|
|
12.
|
Yoon SO, Kim YT, Jung KC, Jeon YK, Kim BH
and Kim CW: TTF-1 mRNA-positive circulating tumor cells in the
peripheral blood predict poor prognosis in surgically resected
non-small cell lung cancer patients. Lung Cancer. 71:209–216. 2011.
View Article : Google Scholar : PubMed/NCBI
|
|
13.
|
Amirghofran Z, Jalali SA, Hosseini SV,
Vasei M, Sabayan B and Ghaderi A: Evaluation of CD44 and CD44v6 in
colorectal carcinoma patients: soluble forms in relation to tumor
tissue expression and metastasis. J Gastrointest Cancer. 39:73–78.
2008. View Article : Google Scholar
|
|
14.
|
Chen Y, Huang K, Li X, Lin X, Zhu Z and Wu
Y: Generation of a stable anti-human CD44v6 scFv and analysis of
its cancer-targeting ability in vitro. Cancer Immunol Immunother.
59:933–942. 2010. View Article : Google Scholar : PubMed/NCBI
|