Introduction
Myelolipoma is a rare benign tumor composed of bone
marrow elements admixed in an adipose tissue neoplasm, commonly
originating from the adrenal gland (1). This type of tumor is typically
discovered incidentally in the adrenal gland and occasionally in
other regions, by pathologists (2).
One of the rare anatomical sites of this tumor is the mediastinum.
Approximately half of the extra-adrenal tumors originate from the
presacral space, with the remainder arising from the perirenal,
mediastinal, hepatic and gastric regions in decreasing order of
frequency (3). We report a case of
non-encapsulated mediastinal myelolipoma which was presented as a
string-of-pearls-type, and diagnosed by pathological analysis. The
study was approved by the Ethics Committee of Beijing Chaoyang
Hospital, Capital Medical University, Beijing, China. Informed
consent was obtained from the patient.
Case report
A 68-year-old female with a history of anemia and
well-controlled type 2 diabetes was admitted to the Beijing
Chaoyang Hospital due to the presence of dull back pain and a cough
for 8 months. There were no other symptoms or physical signs
revealed by physical examination. The blood test results were as
follows: Red blood cells, 2.57×1012/l; hemoglobin, 80
g/l; hematocrit, 23.80%; white blood cells, 5.67×109/l
and platelets, 206×109/l. A bone marrow aspiration and
biopsy demonstrated normal results.
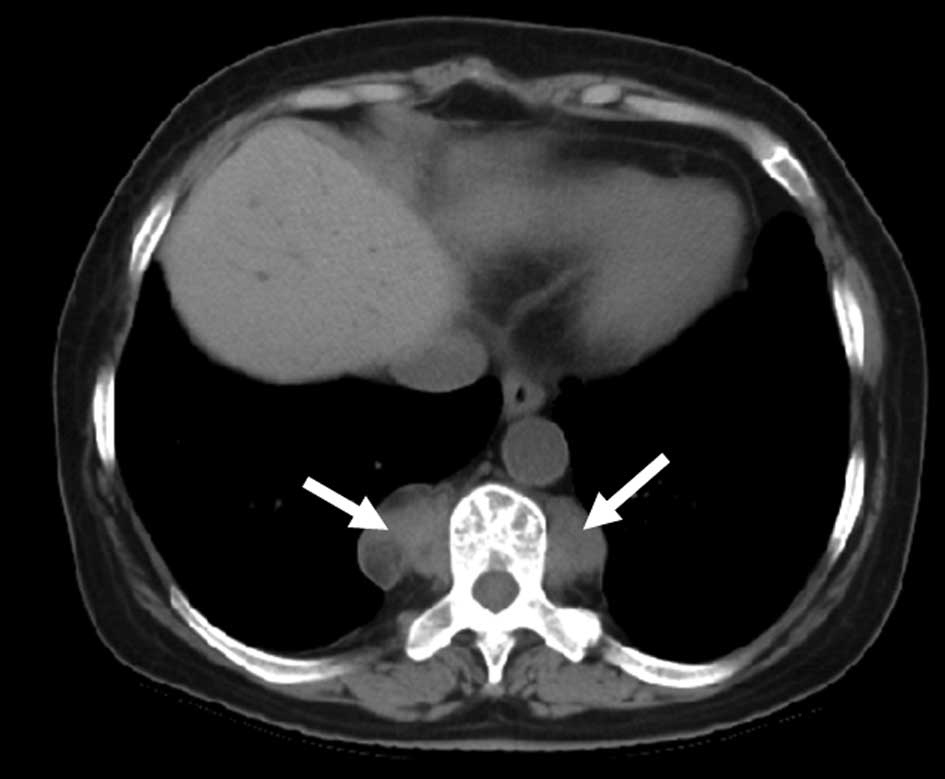
A chest computed tomography (CT) scan revealed two
posterior mediastinal masses. The masses were lobulated at the
paravertebral region between the inferior lobes of the lung. The
right posterior mediastinal mass measured ∼3.1×10 cm and the left
was ∼2.5×9 cm. No evidence of bony erosion, pleural effusion or
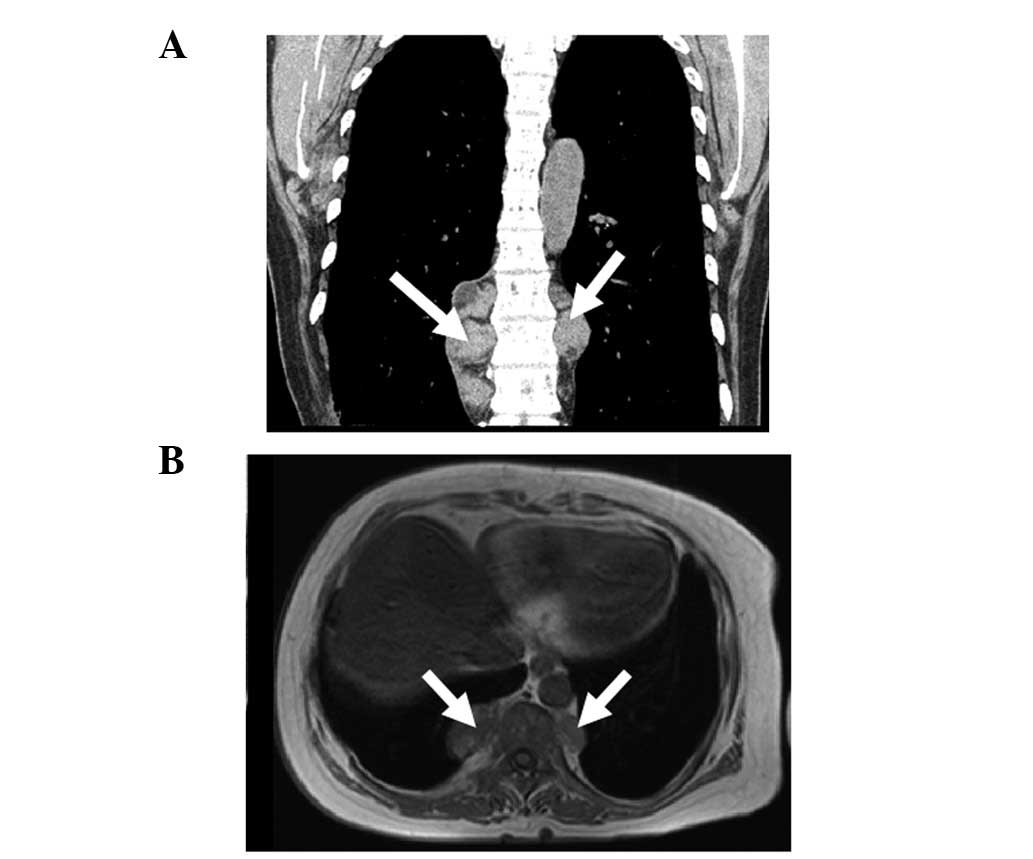
surrounding tissue infiltration was observed (Fig. 1). Magnetic resonance imaging (MRI)
demonstrated a mass extending from levels T9-11 in the coronal
planes. Mixed-signal lesions, mainly equal to a T1/T2 signal, were
observed. In the marginal regions, a cystic lesion exhibited longer
T1 and T2. There was no involvement of the vertebral canal and the
bony structure was normal (Fig. 2).
A CT scan revealed no abnormalities in the renal and adrenal
glands.
A standard left thoracotomy was performed and the
intraoperative findings included string-of-pearls-type
manifestation. The mass resembled fish flesh; it was not completely
encapsulated and had clear boundaries. Tumor invasion of the
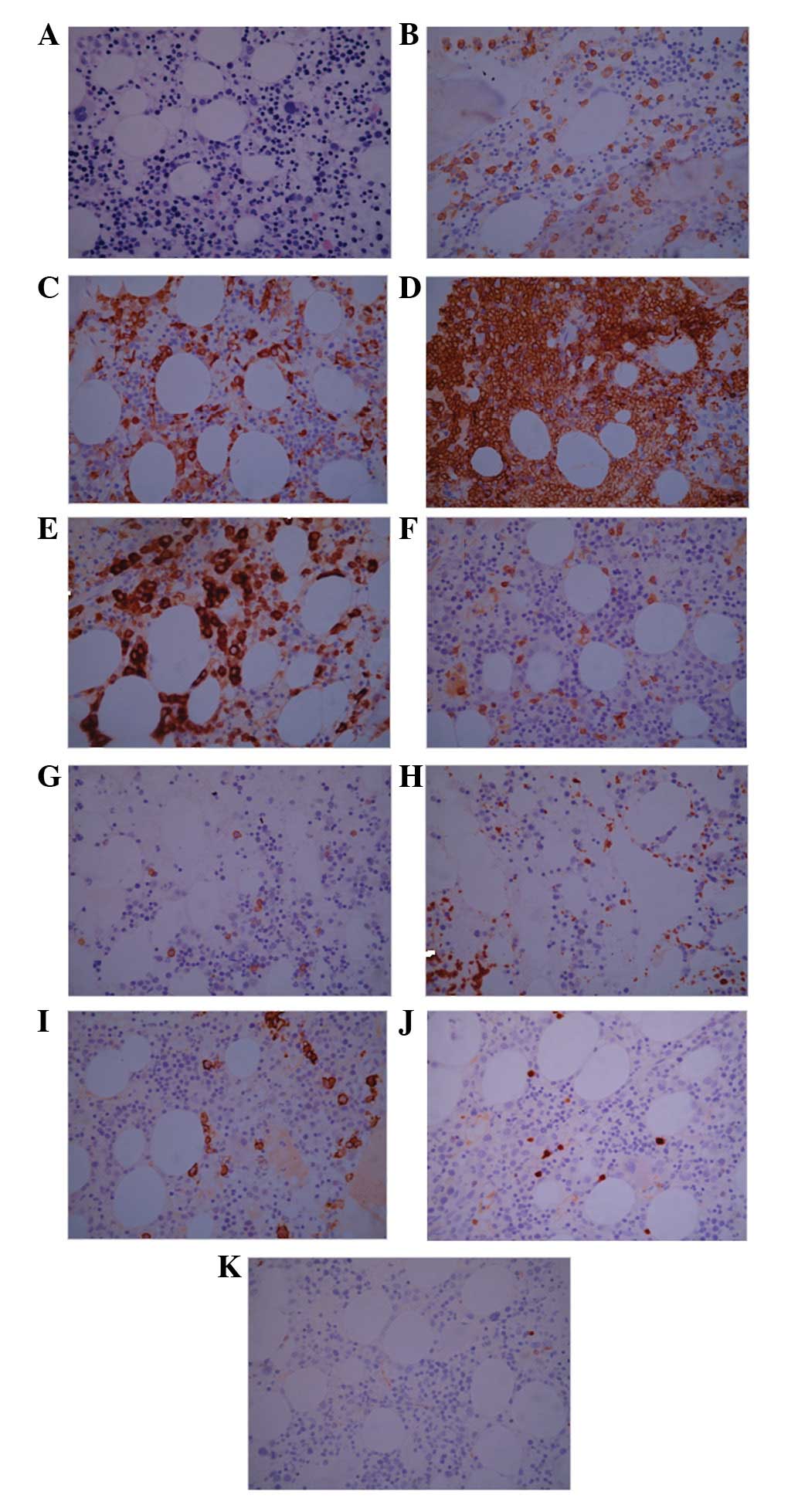
vertebra was not observed. The pathological analysis indicated that
the tumor was benign and a complete excision of the tumor was
achieved. Pathological results revealed predominant mature adipose
tissue with hematopoietic tissue. Microscopical analysis also
demonstrated that the tumor comprised adipose tissue, together with
hematopoietic tissue; features typical of myelolipoma (Fig. 3A). The pathological findings were
consistent with a diagnosis of mediastinal extra-adrenal
myelolipoma, and no signs of malignancy were observed. The
immunohistochemistry results demonstrated that partial cells
expressed CD15, CD235a, CD68 and MPO; minute cells expressed CD3,
CD20, CD61 and CD138; district minority cells expressed TdT and no
cells expressed CD34 (Fig. 3B-K).
The patient was followed up over a 3-year period post-surgery, and
has had no relapses at present.
Discussion
Myelolipoma is a rare, benign neoplasm composed of
mature adipocytes and hematopoietic tissue (4–7). The
disease was first described in 1905, and was given the name
‘myelolipoma’ in 1929 (8).
Myelolipomas mainly occur in the adrenal glands, where they are
typically non-functioning and asymptomatic. The occurrence of the
majority of extra-adrenal myelolipomas has been noted to be in the
presacral region, while primary mediastinal myelolipoma is
rare.
Myelolipomas are mesenchymal tumors composed of a
mixture of adipose and hemopoietic tissue. Usually, myelolipomas
are unilateral and asymptomatic. Myelolipomas are often <4 cm in
diameter; however, larger lesions are capable of causing symptoms
such as a mass effect or a hemorrhage (9). Symptoms associated with large
myelolipomas are typically vague and include back or abdominal
pain. At present, ultrasonography, CT and MRI are useful diagnostic
tools and the incidental detection of myelolipoma has become more
common (10). Although CT and MRI
are effective in diagnosing myelolipoma, it is difficult to make a
confident conclusion. Fine-needle aspiration (FNA) combined
pathology is able to definitively rule out malignancy.
At present, there is no standard method of treatment
for this disease. Daneshmand et al(10) suggested that small asymptomatic
tumors (<4 cm in size) should be monitored, while symptomatic
tumors or large myelolipomas (>7 cm in size) should be removed.
The majority of myelolipomas are incidentally diagnosed by imaging
detection and are not malignant. Therefore, treatment is not
required and patients only need to be monitored regularly.
When myelolipomas grow in particular sites where
they affect the function of important organs or induce certain
symptoms that patients are not able to endure, surgical treatment
is required to remove the myelolipomas. Myelolipomas are frequently
resected by thoracoabdominal incision and may also be removed by
laparoscopic surgery in certain experienced centers (11). Surgical excision is a useful method
for treating myelolipomas, and the tumors generally do not
recur.
In the present case, the patient was an elderly
female who presented with dull back pain and a cough that had
existed for 8 months. CT and MRI scans revealed two posterior
mediastinal masses which presented as a string-of-pearls-type.
However, no characteristics of extra-adrenal myelolipoma were
pre-operatively observed. The patient exhibited symptoms and so the
tumors were removed by thoracic surgery. Surgical resection
followed by pathological analysis is an effective method for
diagnosing rare tumors. The presence of megakaryocytes is essential
for the diagnosis of myeloma (12).
Pathological and immunohistochemical examination demonstrated that
the mass of this patient was myelolipoma. In addition, the patient
suffered from chronic moderate anemia for a further 20 years and
the anemia did not improve following removal of the myelolipoma.
The cause of the anemia was not clear; it may have been induced by
immune factors.
We described a patient with two mediastinal
myelolipomas that had been diagnosed by pathological analysis.
Although the myelolipomas were not particularly large in diameter,
they were both long and they stretched along the spine. Surgical
treatment was effective, and the patient had no relapses for three
years. Although primary mediastinal myelolipoma is rare,
understanding its diagnosis and treatment are important. If a
patient is suspected to have primary mediastinal myelolipoma by CT
or MRI scans, this may be clarified it by pathological analysis.
Subsequently, the tumor may be modified or removed by surgery,
according to its effects on the body.
In conclusion, the present case demonstrates that CT
and MRI scans are able to indicate the presence of mediastinal
myelolipoma. Pathological analysis is an effective method to
clarify the diagnosis. Observation and surgery are two regular
treatment methods. Small, asymptomatic tumors should be monitored,
while large tumors that cause unendurable symptoms may be removed
by surgery.
Acknowledgements
This study was supported by the
National Natural Science Foundation of China (General Program,
Grant No. 81172252).
References
|
1
|
Kenney PJ, Wagner BJ, Rao P and Heffess
CS: Myelolipoma: CT and pathologic features. Radiology. 208:87–95.
1998. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Kim K, Koo BC, Davis JT and Franco-Saenz
R: Primary myelolipoma of mediastinum. J Comput Tomogr. 8:119–123.
1984. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Kawanami S, Watanabe H, Aoki T, Nakata H,
Hayashi T, Kido M, et al: Mediastinal myelolipoma: CT and MRI
appearances. Eur Radiol. 10:691–693. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Dan D, Bahadursingh S, Hariharan S, Ramjit
C, Naraynsingh V and Maharaj R: Extra-adrenal perirenal
myelolipoma. A case report and review of literature. G Chir.
33:62–65. 2012.PubMed/NCBI
|
|
5
|
Akamatsu H, Koseki M, Nakaba H, Sunada S,
Ito A, Teramoto S and Miyata M: Giant adrenal myelolipoma: report
of a case. Surg Today. 34:283–285. 2004. View Article : Google Scholar
|
|
6
|
Heylen S, Hubens G and Vaneerdeweg W:
Giant adrenal myelolipoma: a case report. Acta Chir Belg.
111:91–93. 2011.
|
|
7
|
Hasan M, Siddiqui F and Al-Ajmi M: FNA
diagnosis of adrenal myelolipoma: a rare entity. Diagn Cytopathol.
36:925–926. 2008. View
Article : Google Scholar : PubMed/NCBI
|
|
8
|
Cha JS, Shin YS, Kim MK and Kim HJ:
Myelolipomas of both adrenal glands. Korean J Urol. 52:582–585.
2011. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Lawler LP and Pickhardt PJ: Giant adrenal
myelolipoma presenting with spontaneous hemorrhage. CT, MR and
pathology correlation. Ir Med J. 94:231–233. 2001.PubMed/NCBI
|
|
10
|
Daneshmand S and Quek ML: Adrenal
myelolipoma: diagnosis and management. Urol J. 3:71–74. 2006.
|
|
11
|
Schaeffer EM and Kavoussi LR: Adrenal
myelolipoma. J Urol. 173:17602005. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Gao B, Sugimura H, Sugimura S, Hattori Y,
Iriyama T and Kano H: Mediastinal myelolipoma. Asian Cardiovasc
Thorac Ann. 10:189–190. 2002. View Article : Google Scholar : PubMed/NCBI
|