Introduction
Although surgical treatment for gastric carcinoma
requires standard surgical techniques, the operative period in
surgical treatment for gastric carcinoma depends, not only on the
experience of the surgeons, but also on tumor-related factors and
the physical condition of the patients including whether or not
they have co-morbidities.
Although the continuous progress in early detection
of tumors and advancement in peri-operative management have
undoubtedly contributed to an improvement in the survival of
patients with gastric carcinoma (1), the number of investigations regarding
the effect of the operative time (OT) on the post-operative outcome
of patients with gastric carcinoma is limited.
It may be speculated that the OT taken for the
surgical treatment of gastric carcinoma is greatly influenced by
the degree of tumor advancement.
The aim of the present study was to analyze the
effect of the OT for surgical treatment on the postoperative
outcome of the patients with gastric carcinoma.
Patients and methods
Patients
In total, 330 patients with gastric carcinoma were
enrolled. These patients had been treated by distal or total
gastrectomy through laparotomy and lymph node dissection in our
institution between 1998 and 2010. These 231 males and 99 females
had a median age of 68 years (range, 27–89).
The study was approved by the ethics committee of
the Fukuoka Higashi Medical Center. Consent was obtained from
either the patient or the patient’s family.
Division of operative time
The OT ranged from 88 to 438 min with a mean of 210
min. Patients whose OT was longer and shorter than this mean length
were classified into groups L (n=138) and S (n=192),
respectively.
Follow-up
Patients were followed-up until they succumbed to
the disease and only patients who died of gastric carcinoma were
included in the tumor-related deaths. The period from the surgery
to the date of death was regarded as the survival time. For
patients who died of other non-tumor disease, the period from the
surgery to the last date when the patient was known to be alive
during the study was regarded as the survival time.
Pathological investigation and TNM tumor
stage
The pathological factors were determined according
to the Japanese Classification of Gastric Carcinoma outlined by the
Japanese Gastric Cancer Association (2). TNM tumor stages were determined by the
TNM classification of malignant tumors prescribed by the
International Union Against Cancer (3).
Statistical analysis
Statistical analysis was conducted using StatView
(SAS Institute Inc, Cary, NC, USA). The Chi-square test was used to
compare the difference of proportion values. The Mann-Whitney test
was used to compare the mean age of patients. Survival curves were
generated using the Kaplan-Meier method and the Mantel-Cox test was
used to compare the survival curves. P<0.05 was considered to
indicate a statistically significant result.
Results
The relationship between OT and
clinicopathological variables of the tumors
The proportion of tumors located in the upper area
of the stomach was significantly higher (P=0.003) and the
proportion of macroscopic type 3 or 4 was also significantly higher
in Group L (P=0.009) (Table I).
 | Table ICorrelation of OT with
clinicopathological variables of patients and tumors. |
Table I
Correlation of OT with
clinicopathological variables of patients and tumors.
| Variables | Group L (n=138) | Group S (n=192) | P-value |
|---|
| Gender |
| Male | 102 (73.9) | 129 (67.2) | 0.189 |
| Female | 36 (26.1) | 63 (32.8) | |
| Age | 67.2±9.4 | 68.2±11.7 | 0.448 |
| Location of
tumors |
| Upper | 38 (27.5) | 24 (12.5) | 0.003 |
| Middle | 67 (48.6) | 114 (59.4) | |
| Lower | 33 (23.9) | 54 (28.1) | |
| Gross typea |
| 0 | 47 (34.1) | 97 (50.5) | 0.009 |
| 1, 2 | 35 (25.4) | 41 (21.4) | |
| 3, 4 | 56 (40.5) | 54 (28.1) | |
| Histologyb |
| Well | 24 (17.4) | 52 (27.1) | 0.114 |
| Moderately | 37 (26.8) | 48 (25.0) | |
|
Undifferentiated | 77 (55.8) | 92 (47.9) | |
| Depth of tumors |
| T1 | 44 (31.9) | 98 (51.0) | 0.035 |
| T2 | 12 (8.7) | 25 (13.0) | |
| T3 | 51 (37.0) | 58 (30.2) | |
| T4 | 31 (22.4) | 11 (5.8) | |
| Lymph node
metastasis |
| No | 60 (43.5) | 119 (62.0) | 0.0009 |
| Yes | 78 (56.5) | 73 (38.0) | |
| N1 | 20 | 28 | |
| N2 | 20 | 23 | |
| N3 | 38 | 22 | |
| Lymphatic
invasion |
| No | 46 (33.3) | 104 (54.2) | 0.0002 |
| Yes | 92 (66.7) | 88 (45.8) | |
| Venous invasion |
| No | 88 (63.8) | 153 (79.7) | 0.001 |
| Yes | 50 (36.2) | 39 (20.3) | |
| Tumor stage |
| I | 49 (35.5) | 106 (55.2) | <0.0001 |
| II | 29 (21.0) | 47 (24.5) | |
| III | 49 (35.5) | 37 (19.3) | |
| IV | 11 (8.0) | 2 (1.0) | |
A significant difference was observed between the
two groups with respect to such tumor-related factors as depth of
tumor (P=0.035), lymph node metastasis (P=0.0009), lymphatic
permeation (P=0.0002), venous invasion (P=0.001) and tumor stage
(P<0.0001).
Correlation of OT with surgery-related
factors and postoperative complications
The proportion of patients undergoing total
gastrectomy was significantly higher in Group L (P<0.0001)
(Table II). Moreover, the number
of dissected lymph nodes was also significantly higher in the Group
L (P=0.032). Occurrence of postoperative complications
(P<0.0001) was significantly higher in the Group L.
 | Table IIRelationship between OT and clinical
background of patients. |
Table II
Relationship between OT and clinical
background of patients.
| Group L (n=138) | Group S (n=192) | P-value |
|---|
| Operative
procedure | | | |
| Distal | 69 (50.0) | 152 (79.2) | <0.0001 |
| Total | 69 (50.0) | 40 (20.8) | |
| Number of dissected
nodes | 27.1±11.7 | 24.5±9.6 | 0.032 |
| Post-operative
complications | | | |
| No | 107 (77.5) | 180 (93.8) | <0.0001 |
| Yes | 31 (22.5) | 12 (6.2) | |
| Anastomotic
leaks | 14 | 8 | |
| Others | 17 | 4 | |
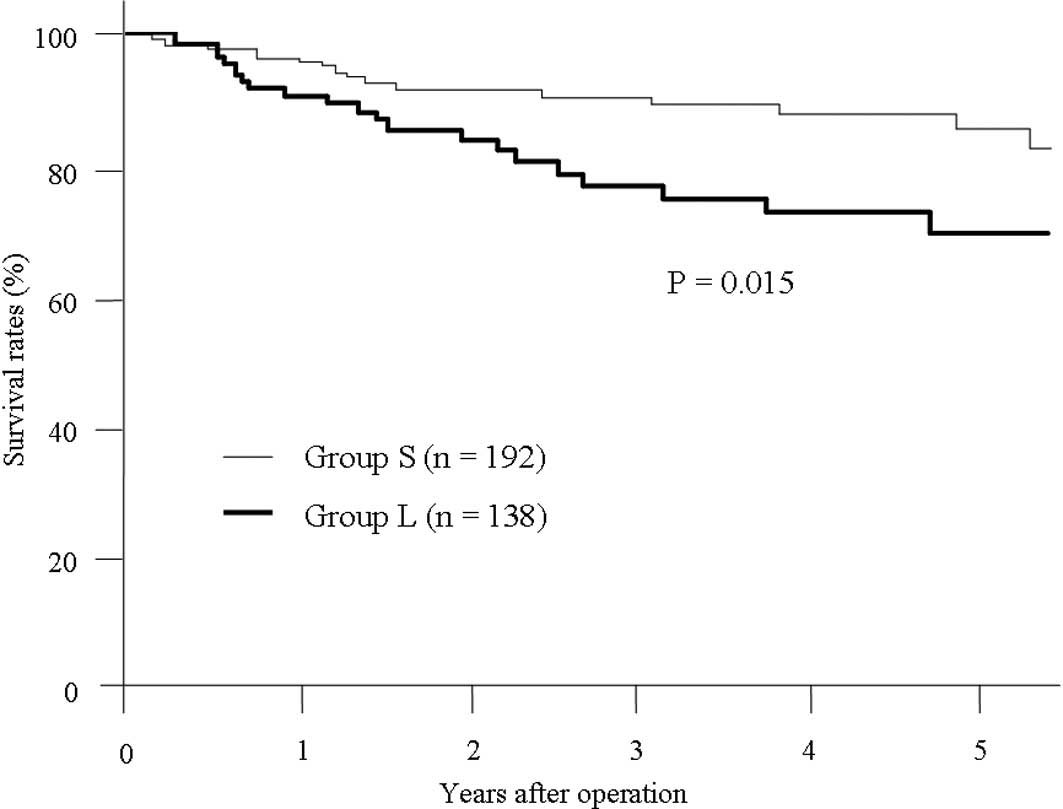
Results of the univariate analysis revealed the 1-,
3- and 5-year survival rates of patients in group L to be 90.4,
76.3 and 69.0%, respectively. The survival rates were significantly
worse that those of patients in group S (96.4, 90.4 and 85.4%,
respectively, P=0.015) (Fig.
1).
Multivariate analysis demonstrated that the TNM
stage of the tumor (P<0.0001) was the only factor independently
associated with a worse prognosis for the patients.
Discussion
Although it is reasonable to assume that a shorter
OT would result in a decrease in incidence of postoperative
complications following surgery for malignant tumors including
gastric carcinoma, the effect of prolongation of OT on subsequent
prognosis of the patients has not been fully discussed.
A standard or permissible OT for performing standard
surgical treatment for gastric carcinoma has not been definitively
established; thus, the average length of the OT among the study
population was selected to dichotomize the patient cohort in the
present study as longer or shorter OT.
The OT may be heavily influenced by the extent of
tumors including their depth, extent of nodal metastasis and
invasion of surrounding tissues. In the present study, tumors of
patients whose OT was longer were found to be significantly more
advanced. Accordingly, the proportion of patients experiencing
postoperative complications was higher in patients who had a longer
OT.
The surgical procedure for a total gastrectomy is
usually more time-consuming compared with that for distal
gastrectomy. Gastric tumors for which total gastrectomy is required
were found to be significantly more advanced compared to those that
could be treated with distal gastrectomy. As such, the OT for
patients who had undergone total gastrectomy was significantly
longer than that for patients treated with distal gastrectomy.
Our results demonstrated that only the stage of the
tumor but not the prolongation of OT was found to be a factor
independently associated with prognosis of the patients with
gastric carcinoma. Correlation of postoperative complications
including anastomotic leakage with subsequent outcome of the
patients with gastric carcinoma remains controversial (4,5). In
the present study, although incidence of postoperative
complications was significantly correlated with prolongation of OT,
postoperative complications were found not to be a prognostic
indicator in gastric carcinoma.
In conclusion, an effort to shorten the operative
period might result in a decrease in postoperative complications,
which may improve the clinical outcome of patients with gastric
carcinoma. Thus, in spite of the non-significance indicated by the
multivariate analysis, the prolongation of OT may indirectly and
eventually worsen the outcome of patients with gastric
carcinoma.
References
|
1
|
Yeoh KG: How do we improve outcomes for
gastric cancer? J Gastroenterol Hepatol. 227:970–972. 2007.
View Article : Google Scholar
|
|
2
|
Japanese Gastric Cancer Association.
Japanese Classification of Gastric Carcinoma. 2nd English edition.
Gastric Cancer. 1:10–24. 1998. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Sobin L, Gospodarowicz M and Wittekind C:
International Union Against Cancer. TNM Classification of Malignant
Tumours. 7th edition. Wiley-Blackwell; New York: pp. 73–77.
2009
|
|
4
|
Yoo HM, Lee HH, Shim JH, Jeon HM, Park CH
and Song KY: Negative impact of leakage on survival of patients
undergoing curative resection for advanced gastric cancer. J Surg
Oncol. 104:734–740. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Sierzega M, Kolodziejczyk P and Kulig J:
Polish Gastric Cancer Study Group: Impact of anastomotic leakage on
long-term survival after total gastrectomy for carcinoma of the
stomach. Br J Surg. 97:1035–1042. 2010. View Article : Google Scholar : PubMed/NCBI
|