Introduction
Surgical wounds are given local care when healing;
for example, by maintaining a moist wound environment to foster
healing (1). There are numerous
types of dressings (including gauze and bandages) and topical
agents (including antiseptics and enzymes) available for surgical
wound management. The ideal dressing for healing wounds has a
number of features, including the ability to absorb and contain
exudate without leakage, impermeability to water and bacteria, lack
of particulate contaminants that may be left in the wound, and
avoidance of wound trauma on dressing removal. However, dressings
and topical agents are occasionally used inappropriately and
uneconomically.
The scientific literature regarding the care of
surgical wounds describes numerous advanced wound care modalities
developed over the past 40 years. Among them, evidence-based
guidelines for the prevention of surgical site infection (SSI) have
been published by the U.S. Centers for Disease Control and
Prevention (CDC) (2). This
organization provides recommendations concerning the reduction of
SSI risk. Each recommendation is classified on the basis of
existing scientific data, theoretical rationale and applicability.
According to these guidelines, the type of postoperative incision
care is determined by whether the incision is closed primarily
(i.e., the skin edges are re-approximated at the end of the
operation), left open to be closed later, or left open to heal by
second intention (2). When a
surgical incision is closed primarily, as is usually the case, the
incision is usually covered with a sterile dressing for 24 to 48 h.
Beyond 48 h, it is unclear whether an incision should be covered by
a dressing, or whether showering or bathing is detrimental to
healing (2).
Most surgically sutured wounds are acute wounds that
heal without complication in an expected time frame. When the
incision is closed primarily, the wounds proceed through a specific
cell and biochemical sequence of healing that comprises overlapping
stages of hemostasis, inflammation, granulation and
epithelialization within 48 h (2).
Previously in our department, surgical wounds were sterilized and
gauze was changed once daily until postoperative day 7 (7POD). This
form of management for surgical wounds was inconsistent with the
CDC guidelines, which raises the question of whether it is
necessary to sterilize surgical wounds and change gauze once daily
until 7POD.
In this study, patients were stratified into two
groups for analysis: patients whose surgical wound was sterilized
and whose gauze was changed once daily until 7POD; and patients
whose surgical wound was sterilized and whose gauze was changed
once daily until 2POD. We evaluated the incidence of SSI, nursing
hours and cost implications.
Patients and methods
Patients
A prospective study of all patients who underwent
operative treatment between May 1 and October 31, 2003, was
performed. These patients were selected from all patients who were
treated during that time period at the Nippon Medical School Main
Hospital, Japan. Study patients were all treated by surgeons in the
surgery department. This was an institutional review board-approved
study, with patient consent obtained for all study patients. Study
inclusion criteria included diagnosis of gastroenterological
disease, breast cancer, inguinal hernia, clinical stability, and
adequate postoperative follow-up documentation. Exclusion criteria
included coexisting diseases, steroid use, complications (including
diabetes mellitus, hypertension, hyperlipidemia and pneumonia),
aged <15 years and failure to return for postoperative
follow-up. Data were collected on age, gender, surgical procedure,
hospital charges and follow-up. Patients were stratified into two
groups for analysis: group A, patients whose surgical wound was
sterilized and whose gauze was changed once daily until 7POD; and
group B, patients whose surgical wound was sterilized and whose
gauze was changed once daily until 2POD.
The surgical wounds of group B were not managed but
were carefully observed beyond 48 h. The gauze surrounding the
drainage tube was changed properly until the drainage tube was
removed. Patient characteristics are shown in Table I. The two groups of patients were
similar in terms of age, gender and diseases. The material cost per
operation and nursing hours for changing the gauze were compared
between the two groups. The prices of consumables, such as gauze,
10% isoGln liquid TM®, 0.2% Welpas® and
sterilized gloves, were obtained from the national medical aids
reimbursement price list. The sterilized gauze was changed an
average of once daily in this study. If a wound infection was
suspected based on the appearance or odor of the wound or systemic
signs (such as fever or tachycardia), the gauze dressing was
removed and the wound was inspected. Using a sterile technique, the
wound was lavaged using saline.
 | Table IPatient characteristics. |
Table I
Patient characteristics.
| Group A (n=40) | Group B (n=41) |
|---|
| Male/female | 26/14 | 28/13 |
| Age (yrs.), mean ±
SD | 61.3±20.1 | 63.2±14.9 |
| Opened
gastrointestinal tract |
| Gastric cancer | 8 | 10 |
| Colon cancer | 5 | 7 |
|
Cholangiocarcinoma | 1 | 1 |
| Hepatocellular
carcionoma | 1 | 3 |
| Pancreatic
cancer | 1 | 3 |
| Appendicitis | 4 | 3 |
| Gallstone | 4 | 4 |
| Closed
gastrointestinal tract |
| Breast cancer | 4 | 3 |
| Inguinal hernia | 12 | 7 |
Results
Rates of surgical site infection
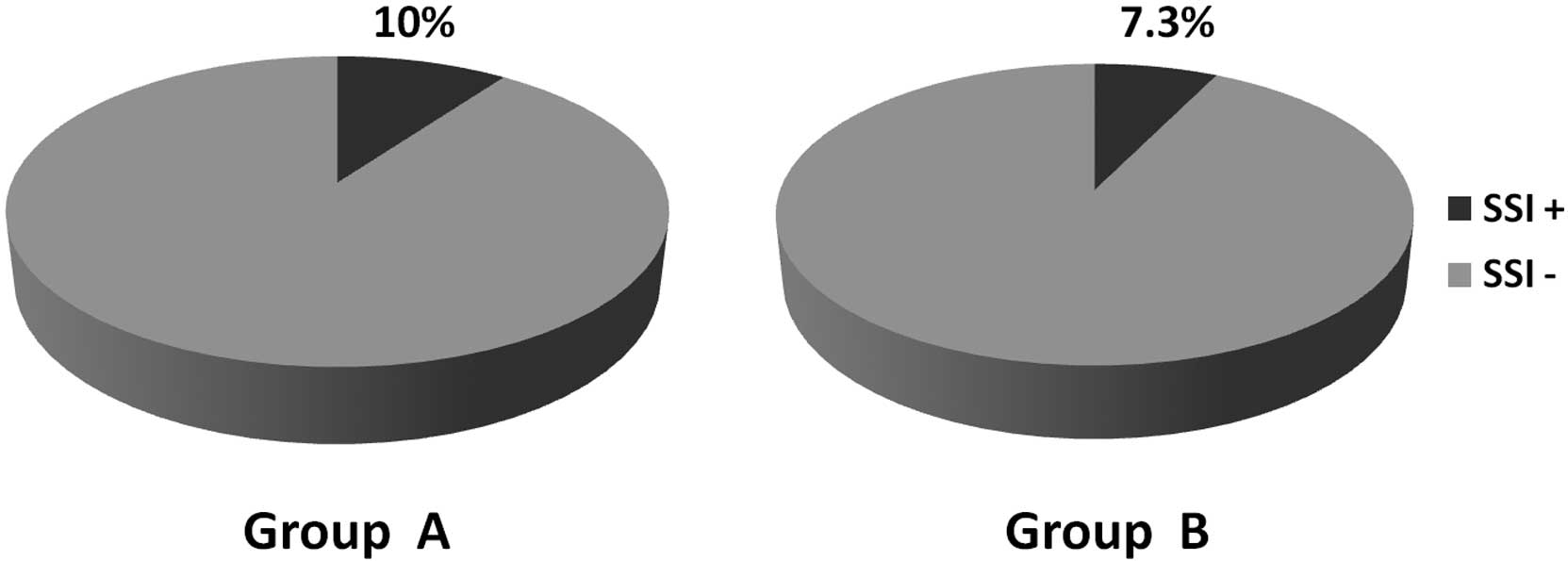
In group A, there were 4 wound infections (10%), all
of which occurred in the midline wound with erythema and induration
(Fig. 1). In group B, there were 3
wound infections (7.3%), all of which occurred in the midline wound
(Fig. 1). These wounds were
reopened and lavaged. There was no significant difference in SSI
occurrence between the two groups.
Clinical outcomes and treatment
costs
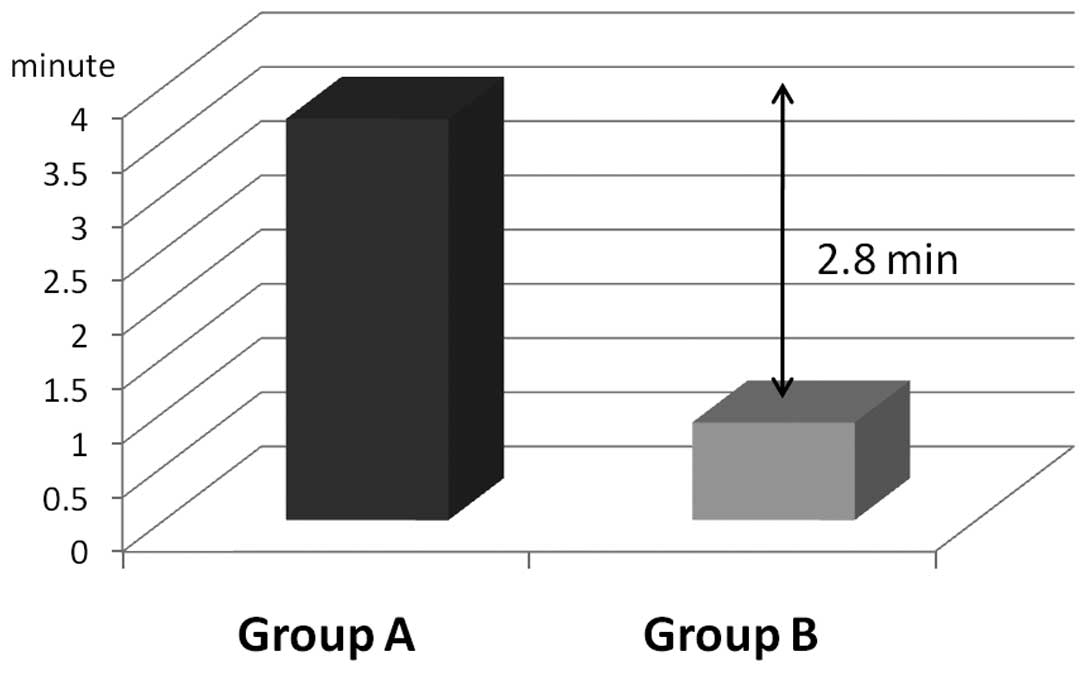
It was anticipated that the implementation of
evidence-based guidelines for wound management would lead to
improved clinical outcomes. The average nursing time was reduced by
2.8 min (71.1%)-3.7 min for group A patients compared with 0.9 min
for group B patients (Fig. 2).
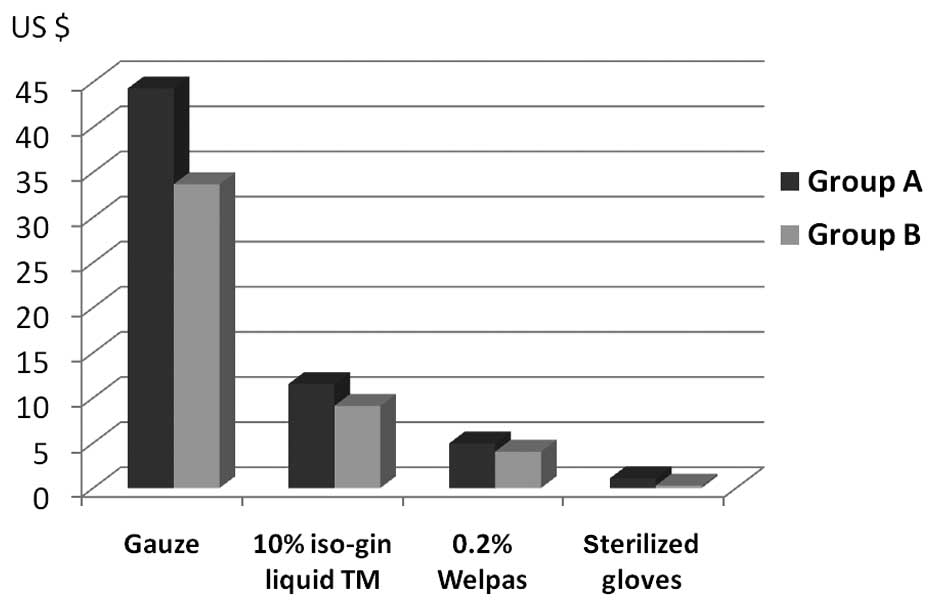
Wound management for 48-h was also expected to reduce material
costs. The material costs per patient were $61.80 (gauze, $44.3;
10% isoGln liquid TM, $11.50; 0.2% Welpas, $4.90; sterilized
gloves, $1.10) in group A and $47.10 (gauze, $33.70; 10% isoGln
liquid TM, $9.10; 0.2% Welpas, $4.00; sterilized gloves, $0.30) in
group B (Fig. 3). The difference in
material costs was $14.70 (a 23.8% reduction).
Discussion
The increasing healthcare expenditure covered by the
National Medical Insurance system has been a critical problem in
Japan. Thus, the costs and consequences of surgical wound
management should be considered a significant healthcare priority
due to its prevalence and the amount of associated healthcare
resource use. Surgical wounds are managed by clinicians, nurses and
caregivers with essential systems of support, including specialized
clinical training, links to allied health care professionals,
established best practice guidelines, measuring and monitoring
tools and focused commitment from health care organizations. The
CDC guidelines do not recommend wound management using gauze-based
dressings beyond 48 h. The development of such guidelines is
occasionally complicated by the heterogeneous nature of SSIs, which
makes it difficult to generalize findings from a study of a
specific patient population to a wider setting, and by the fact
that the impact of various routine practices (such as wearing
surgical gloves) cannot be evaluated for ethical or logistical
reasons (2). This is the reason for
the recent development in wound management not being
well-recognized among patients and health care institutions at
present.
To the best of our knowledge, this is the first
prospective study comparing two principles of surgical wound
management, i.e., conventional 7-day vs. 48-h wound management, in
surgical patients with primary wound closure. Patients were only
recruited from the surgical wards of the hospital for a number of
reasons. First, selecting surgical patients limited patient and
wound heterogeneity. Second, the nursing staff of these wards were
most familiar with the two regimens of surgical wound care. The
evidence from our study shows that, in this clinical setting, 48-h
wound management does not lead to greater SSI or patient discomfort
than conventional 7-day wound management and is likely to be more
cost-effective. In closed surgical wounds, the main function of the
gauze-based dressing is to absorb blood or hemoserous fluid in the
immediate postoperative phase. By contrast, gauze-based dressings
potentially cause avoidable pain and trauma on removal and
typically harden in the wound, requiring softening by bathing prior
to extraction (3). Such pain may
impact on the health-related quality of life of the patient
involved. Early removal of the gauze causes less pain and improved
comfort on removal. It also allows surgical patients to take a
shower or bath since the material had served as a protection of the
wound from environmental influences (4). Moreover, it enables not only the
clinician but also nurses to assess wound healing, the condition of
the surrounding skin, exudate handling and the presence of
infection at any time. These factors also contribute to the quality
of life of the patient.
Forty-eight hour wound management requires fewer
nursing hours for the changing of the gauze, which may lead to
nursing staff being re-assigned to more appropriate duties. In
addition, it contributes to a reduction in the overall cost of
wound management. However, our results showed that a wound can be
healed at a cost of $47.10, assuming that the healing rate is
constant throughout the process. This amount is low compared with
the estimated cost using conventional management, which is at
$61.80. Although there are certain differences in health insurance
systems among countries, this low cost of treating primary closed
surgical wounds is likely to be of considerable interest to medical
insurers and hospitals alike.
To promote the prevalence of evidence-based
guidelines, certain institutes have an identified physician
champion and coordinator. Theoretically, these roles differ in the
way they may exert influence to achieve desired changes, but
function as change agents, using interpersonal contact and strong
communication skills to build trust, promote the use of new
practices, and thus affect behavior (5). The ability of opinion leaders to
change practices is known to be somewhat limited, in part because
studies evaluating this intervention have not described consistent
methods for identifying or engaging opinion leaders (6). The cooperative structure between
clinicians and nurses has resulted in the adoption of all
recommended evidence-based guidelines.
There are a number of limitations to our study. One
involved the difficulty in analyzing the use of antibiotics, since
antibiotics were used not only for serious underlying
intra-abdominal infections, where the duration and type of
antibiotics in part depended on the clinical response in each
patient, but also for a variety of concomitant indications (such as
pneumonia or line sepsis). Therefore, it was not ethical to
restrict the use of antibiotics in accordance with a specified
protocol. Second, it is more likely that other factors played a
more significant role in determining the hospital stay than
surgical wound management. This is the reason for the length of
stay not being taken into consideration in this study. Third, the
investigators evaluating the wounds could not be masked, and this
may have introduced a potential bias depending on each
investigator’s preference for skin closure. Future studies may
benefit from the use of independent assessors who are blinded to
study treatment allocation.
In conclusion, we applied previous knowledge of the
evidence-based CDC guidelines to determine whether 48-h wound
management can be made easier, more uniform, and more
cost-effective compared with conventional wound management. The
results of the present study showed that surgical wound management
methods can be more convenient and inexpensive. Guidelines also
change over time as new methods are adopted. Adaptation and
re-evaluation may therefore be required when new evidence regarding
surgical wound management is published.
Acknowledgements
The authors thank the hospital committees for
endorsing this study.
References
|
1
|
Schultz GS, Sibbald RG, Falanga V, et al:
Wound bed preparation: a systematic approach to wound management.
Wound Repair Regen. 11(Suppl 1): 1–28. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Mangram AJ, Horan TC, Pearson ML, Silver
LC and Jarvis WR: Guideline for prevention of surgical site
infection, 1999. Centers for Disease Control and Prevention (CDC)
Hospital Infection Control Practices Advisory Committee. Am J
Infect Control. 27:97–132, Quiz 133–134; Discussion 196.
1999.PubMed/NCBI
|
|
3
|
Hollinworth H and Collier M: Nurses’ views
about pain and trauma at dressing changes: results of a national
survey. J Wound Care. 9:369–373. 2000.
|
|
4
|
Hermans MH: Clinical benefit of a
hydrocolloid dressing in closed surgical wounds. J ET Nurs.
20:68–72. 1993.PubMed/NCBI
|
|
5
|
Thompson GN, Estabrooks CA and Degner LF:
Clarifying the concepts in knowledge transfer: a literature review.
J Adv Nurs. 53:691–701. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Lansisalmi H, Kivimaki M, Aalto P and
Ruoranen R: Innovation in healthcare: a systematic review of recent
research. Nurs Sci Q. 19:65–72. 2006. View Article : Google Scholar
|