Introduction
In clinical practice, patients who present with
metastases but without a known primary cancer are often
encountered. It is essential to determine the primary tumor and to
treat it accordingly (1). However,
occasionally it is difficult to identify the primary tumor site.
Therefore, it is only possible to resect or treat the metastases.
We report a case of a 43-year-old female patient with a giant
origin-unidentified mucinous adenocarcinoma, measuring 143×430×180
mm, penetrating from the pelvic cavity to the subcutaneous tissue.
The study was approved by the ethics committee of Wuhan General
Hospital of Guangzhou Command, and consent was obtained from the
patient involved.
Case report
A 43-year-old female patient was referred to our
hospital with a giant mass on the left buttock (Fig. 1). The mass was of negligible size
when the patient first noticed it (approximately five years ago)
and the mass gradually grew to the size of a quail’s egg, without
evident symptoms, including pain or limited activity. In November
2008, a percutaneous needle biopsy revealed metastatic mucinous
adenocarcinoma. Pelvic CT and MRI scans demonstrated two
solid-cystic lesions at the bottom of the pelvis, which were
further confirmed by pelvic ultrasound to be a complex mass in the
left adnexa and a right ovarian cyst. The patient underwent a left
ovariectomy and right oophorocystectomy in another hospital, but
the mass on the left buttock was not treated. No malignant changes
were identified upon histological examination of any of the
resected specimens. Following examination, the mass continued to
increase in size and limited the patient’s quality of life, with
symptoms of local discomfort due to pressure stimuli.
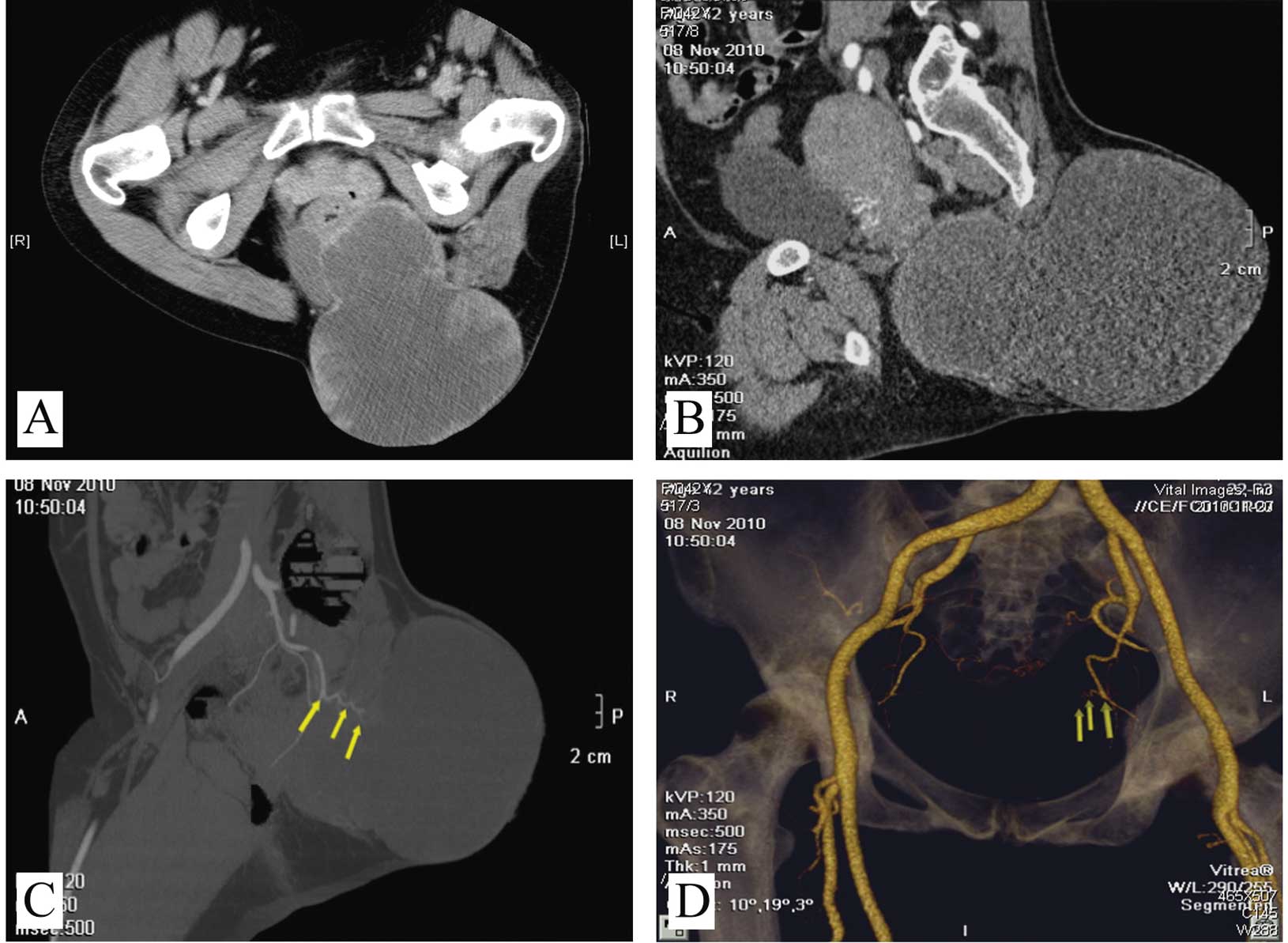
In November 2010, a contrast-enhanced CT scan
revealed a giant solid-cystic mass with a size of 143×430×180 mm,
penetrating from the pelvic cavity to the subcutaneous tissue of
the left buttock, in which part of the mass was enhanced by
contrast medium (Fig. 2A and B). CT
angiography revealed that the mass was fed by the tertiary branches
of the left internal iliac artery (Fig.
2C and D). No adjacent bone destruction or lymph node
metastasis was identified. Clinical examination revealed a large
mass measuring 150×180 mm in the left buttock that was soft,
painless, fluctuant, without skin redness, pigmentation or
increased temperature.
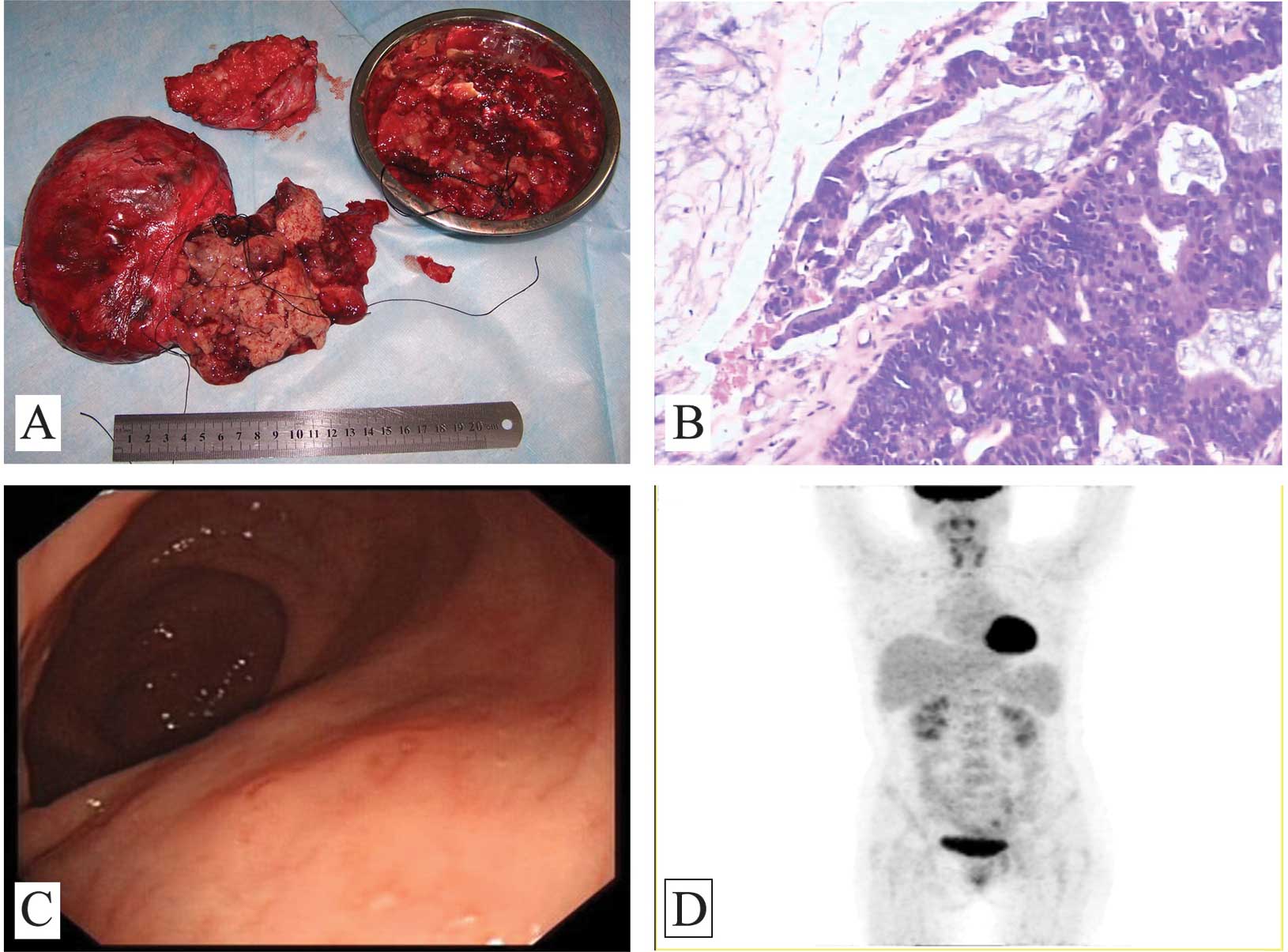
In mid-November 2010, surgery was performed to
remove the mass (Fig. 3A).
Intraoperative examination revealed that the mass was solid-cystic,
with a capsule adhering to the surrounding tissues. Inside the
mass, mucus-like liquid and grape-like tumors were observed.
Postoperative pathological examination revealed mucinous
adenocarcinoma (H&E staining) (Fig.
3B). Immunohistochemical examination using CDX2 (+++), Ki-67
(++60%), CA125 (−), TTF1 (−) and Villin (+++) indicated that the
mass originated from the epithelial tissues of the digestive tract,
but gastrointestinal endoscopes and a postoperative PET-CT scan
demonstrated no evidence of cancer of the digestive tract (Fig. 3C and D). Following surgery, the
patient received six cycles of adjuvant chemotherapy with
oxaliplatin and 5-FU/LV (oxaliplatin 135 mg/m2 day 1;
5-FU 375 mg/m2/day civ 120 h; LV 100 mg/m2
day 1–5). Pelvic conformal radiotherapy was performed at a dose of
2.0 Gy and a total of 60 Gy over six weeks. However, following
surgery, the residual tumor was not reduced as expected, nor did it
progress. At present, the patient remains under observation.
Discussion
In approximately 3 to 5% of all new cancer cases, it
is difficult to determine the primary tumor site, even following
extensive imaging and pathology tests (1,2). This
difficulty is particularly frequent for large or invasive tumors in
the female pelvic region, not only since it is a complex part of
the body, but also because it is an area suitable for the
acceptance of metastasis (3). In
the present case, we were not able to determine the origin of the
mass based on imaging information. The origin may be ovarian,
uterine, rectum or metastatic. Clinical molecular pathology tests
play an increasingly critical role in the differential diagnosis of
a tumor of uncertain origin. With regard to metastatic tumors,
pathology tests may also provide valuable insights to guide the
search for the primary tumor site (4). In the present study, pathological
examination of the resected tissue indicated that the mass was a
metastatic mucinous adenocarcinoma, which was most likely of
gastrointestinal origin. Therefore, we performed gastrointestinal
endoscopes, but no malignant change was detected. PET-CT was
subsequently performed for whole-body imaging. With the exception
of the residual tumor tissue, no other possible tumor was
revealed.
Surgical resection was performed on this patient.
However, due to the complex anatomy of the pelvis and the
difficulty of the surgical approach, the tumor was not completely
resected. Therefore, following surgery, the patient was referred
for chemotherapy and radiotherapy. In accordance with the results
of the pathology tests, combination chemotherapy with oxaliplatin
and 5-FU/LV (oxaliplatin 135 mg/m2 day 1; 5-FU 375
mg/m2/day civ 120 h; LV 100 mg/m2 day 1–5),
which is commonly used to treat gastrointestinal cancer, was
administered (5). During
chemotherapy, pelvic conformal radiotherapy was performed using a
daily dose of 2.0 Gy and a total dose of 60 Gy over six weeks. The
response to adjuvant therapy was evaluated with pelvic CT after
every two cycles. As previously mentioned, comparison of the pre-
and post-treatment CT images indicated no significant changes in
the size of the residual tumor. Notably, in terms of growth rate
and invasion, the tumor may be diagnosed as low-grade malignant, or
even benign. Prior to surgery, the tumor grew continuously at a
relatively slow rate, while following surgery and adjuvant therapy
the residual tumor almost stopped growing. To date, the mass has
existed for over five years and no other metastasis has since been
observed. This may be the reason that the residual tumor was not
sensitive to postoperative chemotherapy and radiotherapy (6).
In China, due to the limitation of the economic
development level and the influence of the coverage of social
security, a number of patients are unable to receive immediate and
adequate treatment. In terms of the present case, if in 2008 when
the patient underwent the first pelvic surgery the mass had been
treated properly, it would not have developed to such a huge
volume. It is possible that the patient may receive a third surgery
in the foreseeable future for the residual tumor following the
second surgery at our hospital.
In conclusion, we have reported the case of a giant
mucinous adenocarcinoma of unknown origin, which penetrates from
the pelvic cavity to the subcutaneous tissue. Since the anatomy
surrounding the tumor is complex, surgery was unable to excise the
tumor completely. Therefore, further observations and/or treatments
are necessary for this patient.
Acknowledgements
This study was partially supported by the National
Foundation of Natural Sciences, China (No. 81101533) and the China
Postdoctoral Science Foundation (No. 20100481468).
References
|
1
|
Pavlidis N, Briasoulis E, Hainsworth J and
Greco FA: Diagnostic and therapeutic management of cancer of an
unknown primary. Eur J Cancer. 39:1990–2005. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Monzon FA, Medeiros F, Lyons-Weiler M and
Henner WD: Identification of tissue of origin in carcinoma of
unknown primary with a microarray-based gene expression test. Diagn
Pathol. 5:32010. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Roblick UJ, Bader FG, Lenander C, et al:
Undifferentiated pelvic adenocarcinomas: diagnostic potential of
protein profiling and multivariate analysis. Int J Colorectal Dis.
23:483–491. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Natoli C, Ramazzotti V, Nappi O, et al:
Unknown primary tumors. Biochim Biophys Acta. 1816:13–24. 2011.
|
|
5
|
McRee AJ, Cowherd S, Wang AZ and Goldberg
RM: Chemoradiation therapy in the management of gastrointestinal
malignancies. Future Oncol. 7:409–426. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Patrone MV, Hubbs JL, Bailey JE and Marks
LB: How long have I had my cancer, doctor? Estimating tumor age via
Collins’ law. Oncology (Williston Park). 25:38–43. 2011.PubMed/NCBI
|