Introduction
In Europe and America, prostate cancer is the most
common type of cancer diagnosed and is the second leading cause of
mortality in male cancer patients. In China, prostate cancer is the
most rapidly increasing type of cancer in males, which has led to
the widespread prostate-specific antigen (PSA) testing and prostate
biopsy. Radical prostatectomy is the standard treatment used to
cure prostate cancer. Severe hemorrhage following prostatectomy is
a rare and serious complication. In a number of patients bleeding
cannot be adequately controlled by conservative measures, including
continuous bladder irrigation, balloon catheter traction or
intermittent blood transfusion. In this study, we report a case in
which superselective internal iliac arterial embolization was used
for the minimally invasive management of severe hemorrhage
following radical prostatectomy.
Case report
A 63-year-old male with a serum PSA concentration of
9.0 ng/ml underwent successful suprapubic radical prostatectomy for
clinical stage T1c prostate cancer (Gleason score, 3+3). The
operative time was 130 min and the blood loss during the procedure
was 300 ml without transfusion.
Within the first 7 days following surgery, the
patient recovered well without experiencing postoperative bleeding
or urine leakage. However, on the eighth postoperative day, the
patient suffered from excessive hematuria and bloody output from
the pelvic drain following defecation. This bleeding was not
controlled by conservative management methods, including continuous
bladder irrigation and balloon catheter traction. In this period,
the patient's hemoglobin was 6.9g/dl, hematocrit level was 19.9%,
blood pressure (bp) was 85/55 mmHg and pulse rate was 110 beats per
min (bpm). Following a large transfusion (4 units of blood, 400 ml
of human plasma), the patient's hemoglobin was 6.3 g/dl, hematocrit
level decreased to 17.6%, bp was 85/55 mmHg and pulse rate was 110
bpm. However, large transfusions were unable to replace the
patient's blood loss and hypovolemic shock was unavoidable.
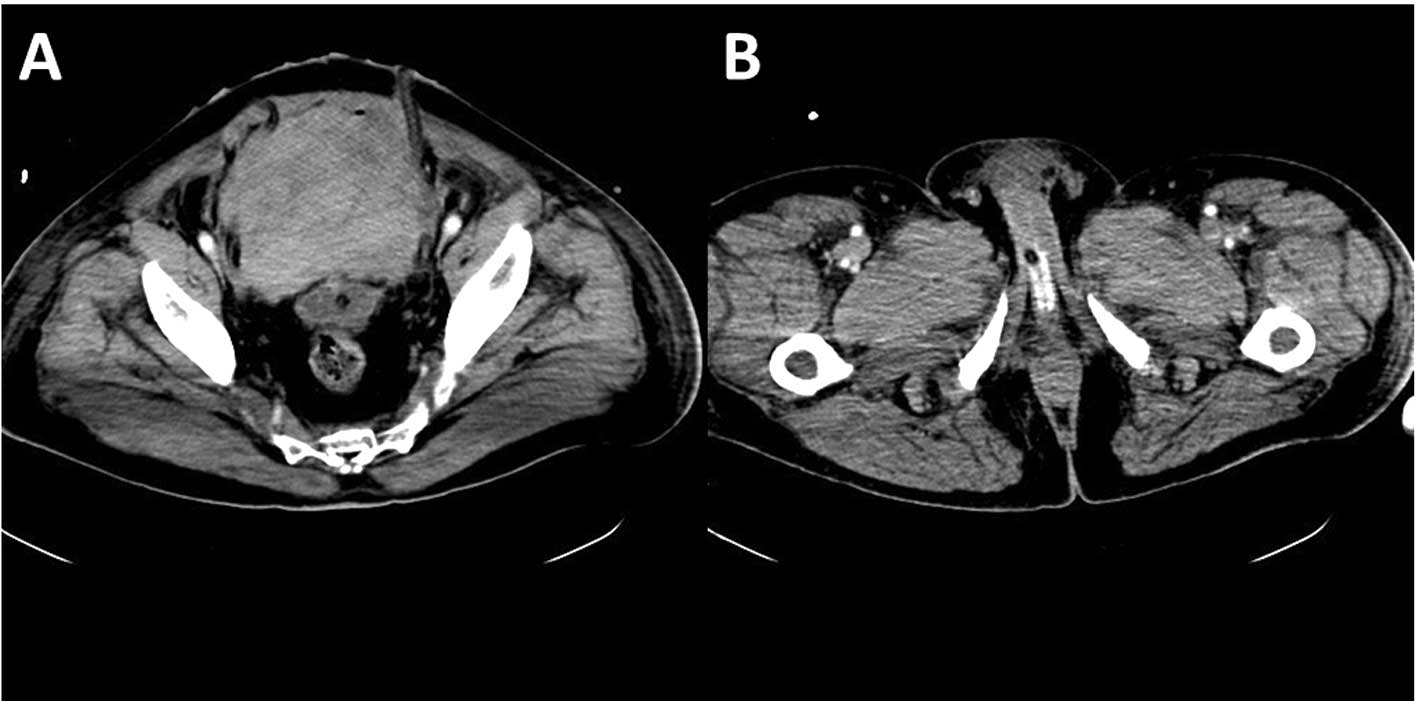
Computed tomography angiography (CTA) identified a
large pelvic hematoma and active bleeding sites close to the
urethrovesical anastomosis (Fig.
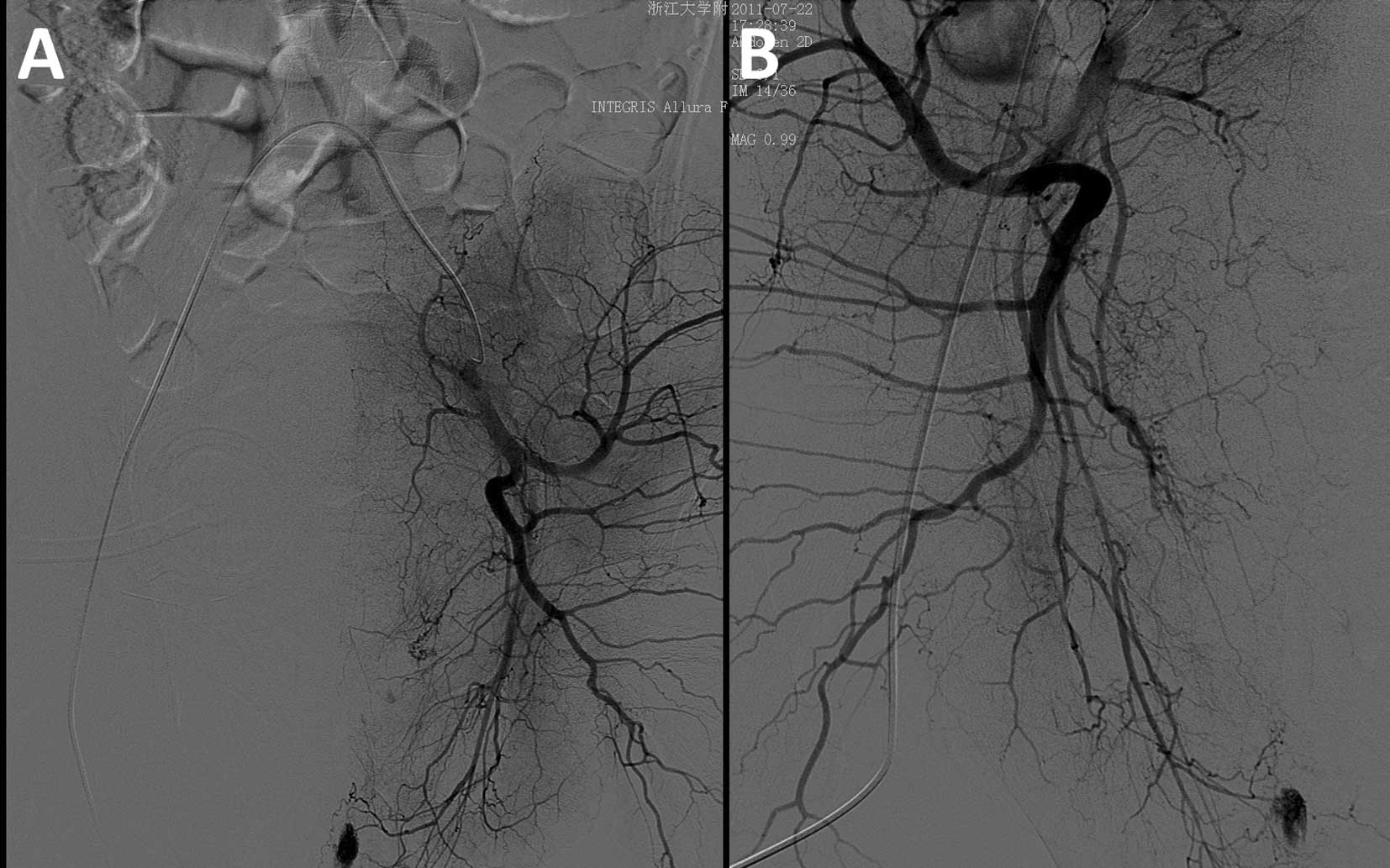
1). Digital subtraction angiography (DSA) of the lower
abdominal aorta was conducted via a transfemoral approach using a
angiographic catheter (5 Fr) and revealed contrast extravasation
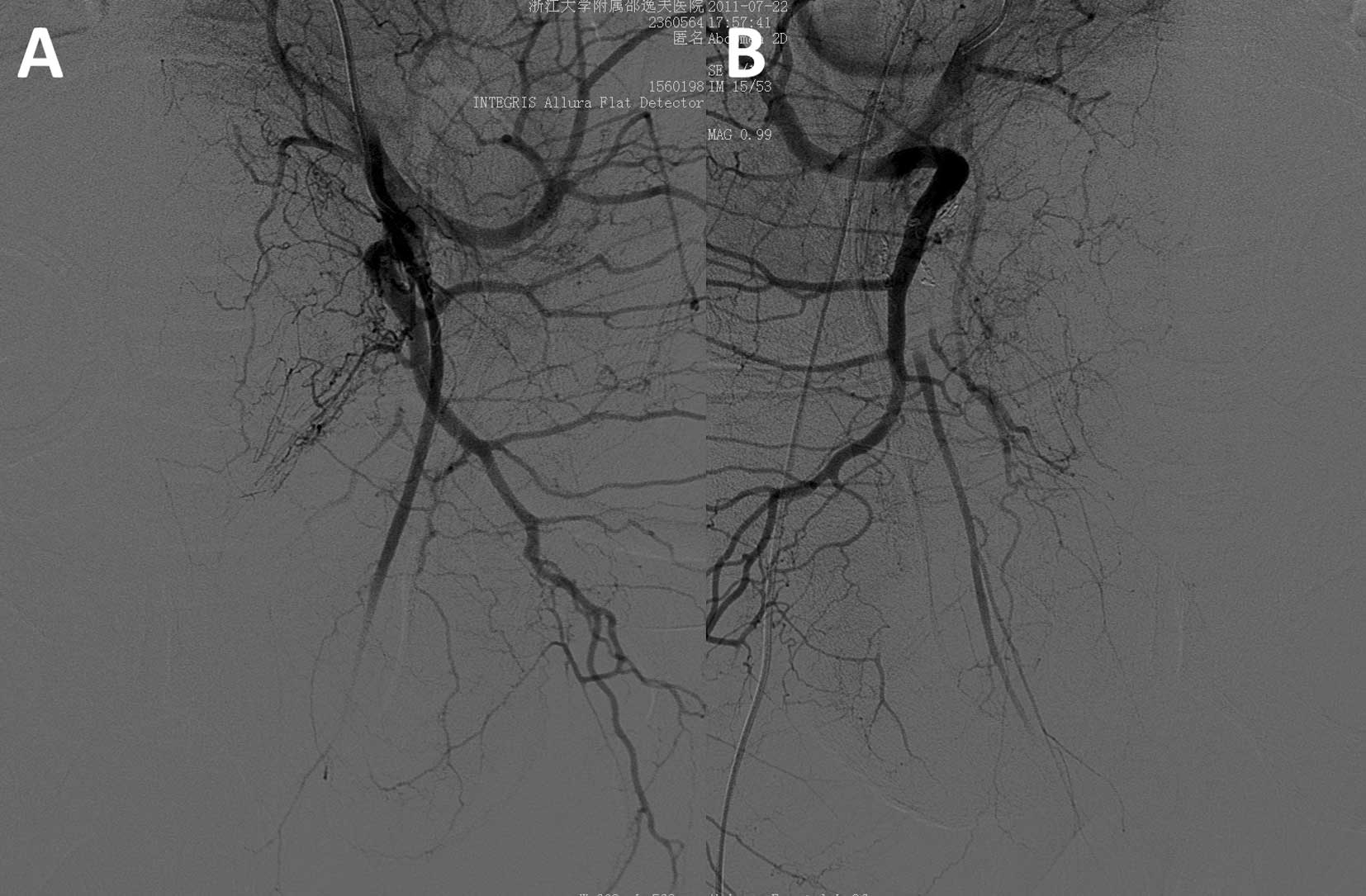
from branches of the bilateral internal iliac artery (Fig. 2). Superselective angiography of the
internal iliac artery was used to further confirm the bleeding
sites (Fig. 3). Using a
microcatheter tracker (2.5 Fr) with a guidewire (0.014 inch),
superselective embolization was conducted using different sized
microcoils (5 mm × 5 cm × 2, 2 mm × 3 cm × 2 for 2 arterial
branches derived from the left internal iliac artery; 2 mm × 3 cm ×
2, 3 mm × 3cm × 2 and 4 mm × 3 cm × 2 for 3 arterial branches
derived from the right internal iliac artery) (Fig. 4).
The procedure was successful as there were no
post-procedure complications or further bleeding. The hemoglobin
and hematocrit levels remained stable and the patient was
discharged on the 14th postoperative day. At 6 months follow-up,
the patient had recovered well, regained excellent urinary
continence and the pelvic hematoma was absorbed using ultrasound
examination.
Discussion
Historically, major bleeding has been a significant
problem associated with radical retropubic prostatectomy. Since the
anatomy of the dorsal venous complex and a technique for its early
control during radical retropubic prostatectomy were described
(1), the incidence of
intraoperative and postoperative bleeding has decreased.
Life-threatening hemorrhage following a radical prostatectomy is a
rare event (2,3). When conservative measures are unable
to stop the bleeding, more invasive measures, including open
surgical exploration or bilateral extraperitoneal internal iliac
ligation have been proposed (3,4).
Although open surgical exploration has been the
standard treatment in this situation, there is a continuing search
for a minimally invasive procedure to reduce complications.
Transcatheter arterial embolization (TAE) has gained an increasing
role in controlling life-threatening hemorrhage from various
bleeding sites. Since the introduction of internal iliac
embolization in 1974 by Hald and Mygind (5), it has been successfully used in
controlling pelvic bleeding. Appleton et al (6) reported their experience with
embolization of the internal iliac artery in eight patients with
severe bladder hemorrhage and in two with severe bleeding following
a prostatectomy. Effective control of the bleeding was achieved in
six patients with bladder hemorrhage and in the two patients with
postprostatectomy bleeding. Nabi et al (7) described the successful management of
intractable hematuria due to bladder and prostatic tumor using
embolization of the anterior division of the internal iliac artery
with no recurrence at a mean follow-up of 22 months. Effective
embolization of prostatic vessels following transurethral resection
of the prostate (TURP) or prostatic biopsy has also been reported
(8–10).
With the continuous development of microcatheters,
embolic materials and DSA, superselective embolization has become a
possible management technique for the treatment of severe
hemorrhage. De Berardinis et al (11) reported a successful case of
superselective embolization of the bladder arteries in the
treatment of a severe bladder hemorrhage due to radiation cystitis
following radiotherapy. Superselective embolization has also been
conducted in 2 cases of a pseudoaneurysm of the internal pudendal
artery with arteriovenous fistula following extraperitoneal
laparoscopic radical prostatectomy (12). Jeong et al (13) also described the successful
treatment of 4 patients who had severe immediate postoperative
bleeding following radical prostatectomy using superselective
embolization. In the present study, superselective embolization was
conducted by introducing a microcatheter tracker (2.5 Fr) with a
guide wire (0.014 inch) into the branches of the internal iliac
arteries. Non-absorbable microcoils were used as embolization
material.
When managing postoperative bleeding following a
radical prostatectomy, another important factor to consider is the
preservation of urethrovesical anastomosis. In the present study,
if open surgical exploration had been used, reworking of the
urethrovesical anastomosis would have been extremely difficult.
This is due to the severe inflammation and edema that was
identified on the eighth postoperative day and the active bleeding
sites which are close to the urethrovesical anastomosis. Therefore,
we selected the TAE technique to maintain the urethrovesical
anastomosis. At 6 months follow-up, the patient recovered well and
regained excellent urinary continence.
Compared to selective embolization and other methods
(14), the advantages of
superselective embolization include a lower recurrence rate with
regards to bleeding and fewer side-effects, including
postembolization gluteal pain, claudication and tissue necrosis,
which require necessitating frequent morphine injections (15). Superselective embolization not only
immediately controls the problems associated with severe
hemorrhage, but also minimizes the complications.
In conclusion, in the present study, we described a
case in which superselective embolization was used to control a
severe hemorrhage, which occurred following radical prostatectomy.
We concluded that a rapid diagnosis by CTA and an early
superselective embolization of the internal iliac artery should be
considered as the treatment of choice in severe hemorrhage cases
following radical prostatectomy.
References
|
1
|
Reiner WG and Walsh PC: An anatomical
approach to the surgical management of the dorsal vein and
Santorini's plexus during radical retropubic surgery. J Urol.
121:198–200. 1979.
|
|
2
|
Hedican SP and Walsh PC: Postoperative
bleeding following radical retropubic prostatectomy. J Urol.
152:1181–1183. 1994.PubMed/NCBI
|
|
3
|
Kaufman JD and Lepor H: Reoperation versus
observation in men with major bleeding after radical retropubic
prostatectomy. Urology. 66:561–565. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Rao MS, Rao KM, Vaidyanathan S, et al:
Massive venous hemorrhage after bilateral internal iliac artery
ligation following retropubic prostatectomy. Eur Urol. 4:465–467.
1978.
|
|
5
|
Hald T and Mygind T: Control of
life-threatening vesical hemorrhage by unilateral hypogastric
artery muscle embolization. J Urol. 112:60–63. 1974.PubMed/NCBI
|
|
6
|
Appleton DS, Sibley GN and Doyle PT:
Internal iliac artery embolisation for the control of severe
bladder and prostate haemorrhage. Br J Urol. 61:45–47. 1988.
View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Nabi G, Sheikh N, Greene D and Marsh R:
Therapeutic transcatheter arterial embolization in the management
of intractable haemorrhage from pelvic urological malignancies:
preliminary experience and long-term follow-up. BJU Int.
92:245–247. 2003. View Article : Google Scholar
|
|
8
|
Suzuki Y, Nakada T, Ishigooka M, et al:
Pelvic arteriovenous aneurysm caused by transurethral resection of
the prostate: successful management by intra-arterial embolization.
Urol Int. 60:191–193. 1998. View Article : Google Scholar
|
|
9
|
Kaneko T, Suzuki T, Matsushita N and
Yoshida I: Transcatheter arterial embolization for bleeding of
prostatic artery after prostate biopsy. Nihon Hinyokika Gakkai
Zasshi. 94:693–695. 2003.PubMed/NCBI
|
|
10
|
Barbieri A, Simonazzi M, Marcato C, et al:
Massive hematuria after transurethral resection of the prostate:
management by intra-arterial embolization. Urol Int. 69:318–320.
2002. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
De Berardinis E, Vicini P, Salvatori F,
Sciarra A, Gentile V and Di Silverio F: Superselective embolization
of bladder arteries in the treatment of intractable bladder
haemorrhage. Int J Urol. 12:503–505. 2005.
|
|
12
|
Lopes RI, Mitre AI, Rocha FT, Piovesan AC,
da Costa OF and Karakhanian W: Case report: late recurrent
hematuria following laparoscopic radical prostatectomy may predict
internal pudendal artery pseudoaneurysm and arteriovenous fistula.
J Endourol. 23:297–299. 2009. View Article : Google Scholar
|
|
13
|
Jeong CW, Park YH, Ku JH, Kwak C and Kim
HH: Minimally invasive management of postoperative bleeding after
radical prostatectomy: transarterial embolization. J Endourol.
24:1529–1533. 2010. View Article : Google Scholar
|
|
14
|
Pisco JM, Martins JM and Correia MG:
Internal iliac artery: embolization to control hemorrhage from
pelvic neoplasms. Radiology. 172:337–339. 1989. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Greenstein A, Merimsky E, Papo J and Braf
Z: Persistent gluteal pain after embolization of the hypogastric
arteries. An unexpected complication. J Urol (Paris). 89:595–596.
1983.PubMed/NCBI
|