Introduction
Burkitt’s lymphoma (BL) is a high-grade mature
B-cell neoplasm which represents 8–10% of all tumors in individuals
younger than 15 years old. It is composed of monomorphic
medium-size B cells with basophilic cytoplasm and numerous mitotic
figures (1–3). BL may occur as an abdominal tumor,
which in rare cases may include gastric mucosa (less than 2%),
although in most cases, the tumor is located in the ileum or cecum.
Primary gastric lymphoma constitutes 1.48% of all gastric cancers
in children (4–7). We report the case of a 4-year-old male
presenting with discontinuous abdominal pain, weight loss,
constipation and irritability with a diagnosis of gastric BL. This
study focuses on the significant possibility of BL in children with
gastric mass. The patient’s family consented to this study.
Case report
A 4-year-old male, with discontinuous abdominal
pain, anorexia and weight loss of approximately 3 kg, constipation
and irritability, was admitted to our clinic. The patient had
presented recurrent spasmodic abdominal pain for approximately one
month and usually the individual felt better following gas
emission. His familial history was negative for lymphoma, gastric
carcinoma or other gastrointestinal malignancies. On physical
examination the patient presented with pallor and edema of the left
eye. There was no respiratory distress, lymphadenopathy, jaundice,
abdominal masses or hepatosplenomegaly. The laboratory tests showed
the following: anemia (hb 9.8 l/dl), elevated white blood cell
count (WBC) [13x109cells/l (of which N 59%, L 29%, M
7.6%, E 3.5% and B 0.5%)] and platelet counts
534x109cells/l. Tests also showed elevated levels of
serum lactate dehydrogenase (LDH) 966 U/l (normal value, 150/500),
sedimentation rate 37 mm/h and ferritin 5 ng/ml; occult blood in
the stool was positive.
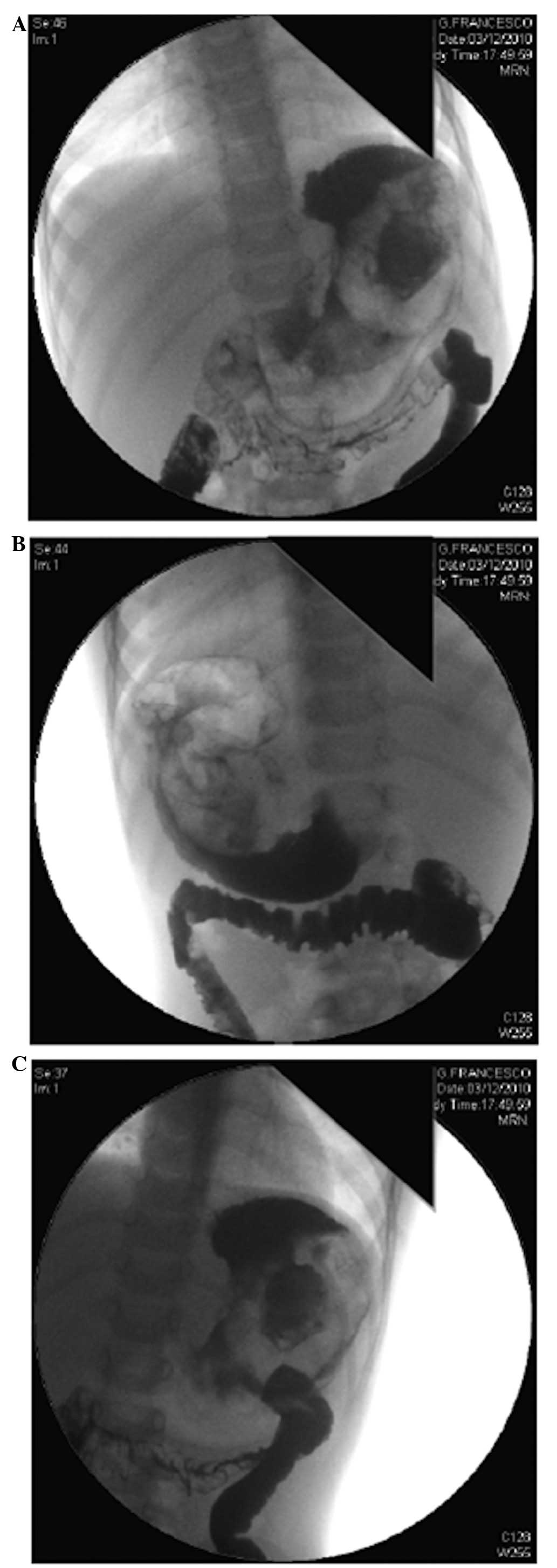
The abdominal X-ray with contrast showed an
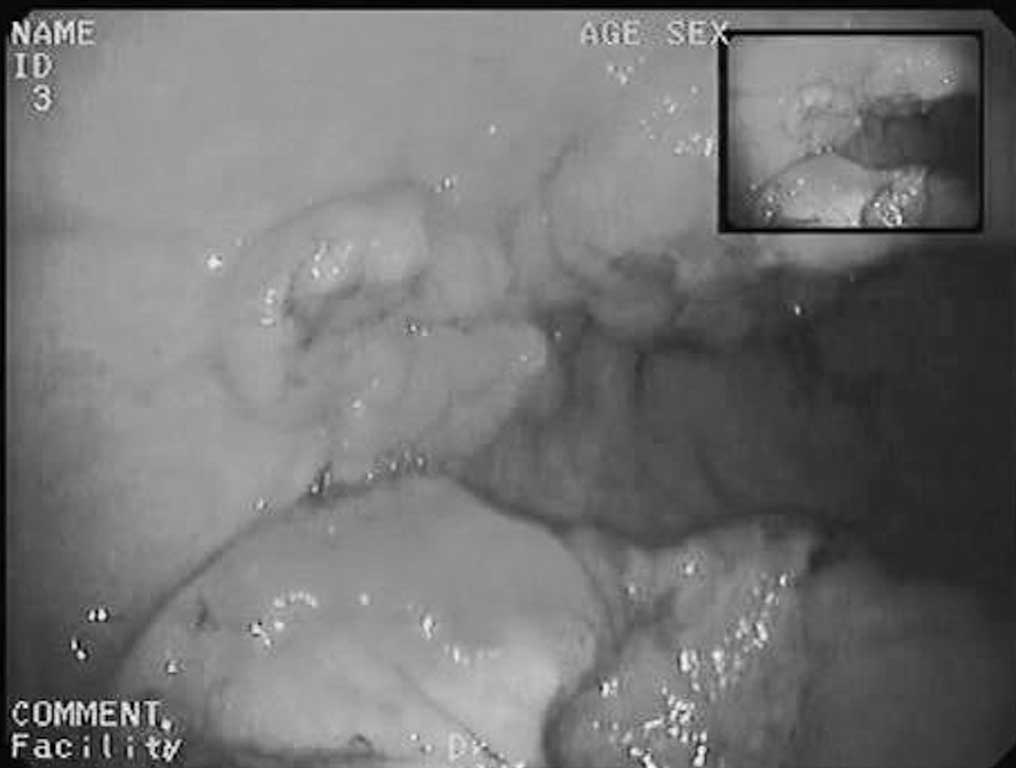
exophitic lesion in the stomach with central ulceration (Fig. 1). A gastroduodenal endoscopy was
performed under general anesthesia, which showed an ulcerated
masses along the anterior and posterior walls of the gastric body;
the remaining gastric wall appeared normal. The morphological
features were consistent with the diagnosis of non-epithelial
neoplasia (Figs. 2 and 3). Gastric biopsies were performed and
histological examination confirmed the diagnosis of gastric BL.
Immunohistochemistry revealed that lymphoid cells were positive for
CD20, CD10 and CD38 and negative for CD44 and Bcl2. Abdominal,
neck, head and testicular ultrasound scans and total body magnetic
resonance imaging (MRI) scans were performed. Total body positron
emission tomography revealed a large gastric hyper-metabolic mass
and increased uptake in the bowel, thigh bone and bone marrow. Bone
marrow aspirate and cerebrospinal fluid were positive for lymphoma.
These examinations showed the presence of diffuse disease. Based on
the results of the examinations, the patient was graded as fourth
risk group (R4) since LDH levels were greater than 1000 U/l (1,214
U/l) and bone marrow was involved. The patient was discharged and
referred to the Pediatric Oncology Center for chemotherapy.
Discussion
Non-Hodgkin’s lymphoma (NHL) is the third most
common cancer (10%) and accounts for approximately 60% of all
lymphomas in children and adolescents. The four major pathological
subtypes of childhood and adolescents NHL are BL (40%),
lymphoblastic lymphoma (30%), diffuse large B-cell lymphoma (20%)
and anaplastic large cell lymphoma (10%) (2).
Two clinical variants of BL have been recognized by
the World Health Organization classification (WHO): endemic and
sporadic, which are indistinguishable by histology, but have a
different geographical distribution. The etiology of endemic BL is
correlated with the Epstein-Barr virus (EBV) and frequently
presents with tumors of the head and neck in a population in
equatorial Africa. Translocation involving the C-MYC gene is a
consistent feature of BL. BL cases have a translocation involving
the C-MYC gene at 8q24 with the immunoglobulin heavy chain gene
(IGH) at 14q32, or, less commonly, with κ light chain locus (IGK)
at 2q11 or λ light chain locus (IGL) at 22q11 (8,9). The
etiology of sporadic BL is unknown; the disease has an abdominal
presentation and is the most common type of lymphoma occurring in
young children in the USA; the presenting symptoms include: an
abdominal mass, intestinal obstruction, intussusceptions and acute
abdominal pain. In most cases, the abdominal mass is located in the
ileum or cecum, however, in rare cases it can include the gastric
mucosa (less than 2%) (7). Primary
gastric lymphoma constitutes as low as 1.48% of all gastric cancers
in children (4–6). At present, surgery has a minimal role
in the treatment of this pathology since chemotherapy is the
mainstay treatment for all variants of BL, due to its extreme
sensitivity. A good prognosis has been reported for these patients,
however, treatment depends on the stratification of patients into
four risk groups (R1–4). R1 includes patients with completely
resected disease and a negative histopathological exam of lymph
nodes; R2, incompletely resected or unresected disease and
extra-abdominal disease localization or abdominal and LDH levels
less than 500 IU/l; R3, unresected abdominal lymphoma and LDH
levels between 500 and 1,000 IU/l and patients with bone marrow
without CNS (central nervous system) involvement; and R4, LDH
levels greater than 1,000 IU/l and with bone marrow and/or CNS
involvement (10,11). The present case shows the importance
of considering the possibility of malignancy in children with
gastric neoformation or in patients presenting with discontinuous
abdominal pain, weight loss and irritability. The literature
confirms the rarity of primary gastric lymphoma in children, as
less than 20 children have been described during the last decade
and most of these lymphomas are high-grade lymphoma (7,12).
References
|
1.
|
TW McLeanRS FarberZT LewisMM WoffordMJ
PettenatiT PranikoffAR ChauvenetDiagnosis of Burkitt lymphoma in
pediatric patients by thoracentesisPediatr Blood
Cancer499092200710.1002/pbc.2068316302222
|
|
2.
|
A GenceC SahinAC CelayirH YavuzPrimary
Burkitt lymphoma presenting as a solitary rectal polyp in a
childPediatr Surg
Int2412151217200810.1007/s00383-008-2238-118810465
|
|
3.
|
C BellanS LazziG De FalcoEA RogenaL
LeonciniBurkitt lymphoma versus diffuse large B-cell lymphoma: a
practical approachHematol
Oncol27182185200910.1002/hon.91419670467
|
|
4.
|
GJ HarrisMJ LaszewskiPediatric primary
gastric lymphomaSouth Med
J85432434199210.1097/00007611-199204000-000241566151
|
|
5.
|
JH ChiengJ GarrettSL DingM
SullivanClinical presentation and endoscopic features of primary
gastric Burkitt lymphoma in childhood, presenting as a
protein-losing enteropathy: a case reportJ Med Case
Reports37256200910.4076/1752-1947-3-7256
|
|
6.
|
V KesikM SafaliEC CitakE KismetV
KoseogluPrimary gastric Burkitt lymphoma: a rare cause of
intraabdominal mass in childhoodPediatr Surg
Int26927929201010.1007/s00383-010-2671-920661578
|
|
7.
|
C JacquemartO GuidiI EtienneR DelrezP
ForgetMF DresseG DepasL de LevalC HoyouxPediatric gastric lymphoma:
a rare entityJ Pediatr Hematol
Oncol30984986200810.1097/MPH.0b013e31818c915b19131798
|
|
8.
|
SM MbulaiteyeRJ BiggarK BhatiaMS LinetSS
DevesaSporadic childhood Burkitt lymphoma incidence in the United
States during 1992–2005Pediatr Blood Cancer53366370200919434731
|
|
9.
|
MS CairoE RaetzMS LimV DavenportSL
PerkinsChildhood and adolescent non-Hodgkin lymphoma: new insights
in biology and critical challenges for the futurePediatr Blood
Cancer45753769200510.1002/pbc.2034215929129
|
|
10.
|
M PillonM PiglioneA GaraventaV ConterM
GiulianoG ArcamoneR MuraM CelliniES D’AmoreS VarottoL MussolinA
RosolenAIEOP-NHL CommitteeLong-term results of AIEOP LNH-92
protocol for the treatment of pediatric lymphoblastic lymphoma: a
report of the Italian Association of Pediatric Hematology and
OncologyPediatr Blood
Cancer53953959200910.1002/pbc.2216219621432
|
|
11.
|
AH EldarB FutermanG AbrahamiD AttiasAB
BarakY BursteinR DvirBurkitt lymphoma in children: the Israeli
experienceJ Pediatr Hematol
Oncol31428436200910.1097/MPH.0b013e31819a5d5819648792
|
|
12.
|
M MoschoviD MenegasK StefanakiCV
ConstantinidouF Tzortzatou-StathopoulouPrimary gastric Burkitt
lymphoma in childhood: associated with Helicobacter
pylori?Med Pediatr
Oncol41444447200310.1002/mpo.1031914515383
|