Intruduction
Paragangliomas are extra-adrenal chromaffin tumors
that arise from neuroectodermal cells of the autonomous nervous
system (1). They may be located in
the skull base, neck, chest and abdomen. When found within the
abdomen, a silent paraganglioma may be mistaken for other
retroperitoneal tumors, such as lymphoma and tumors of the pancreas
(2). Futhermore, para-aortic
multiple paraganglioma in the abdomen is an extremely rare disease
(3). In many patients, asymptomatic
paragangliomas were not found until the patient presented with
non-specific symptoms. We report a case of a para-aortic multiple
paraganglioma diagnosed during surgery, which was completely
removed in the operation. The study was approved by the ethics
committee of Anyang Tumor Hospital and Anyang Hygiene Bureau,
China. Consent was obtained from the patient in this study.
Case report
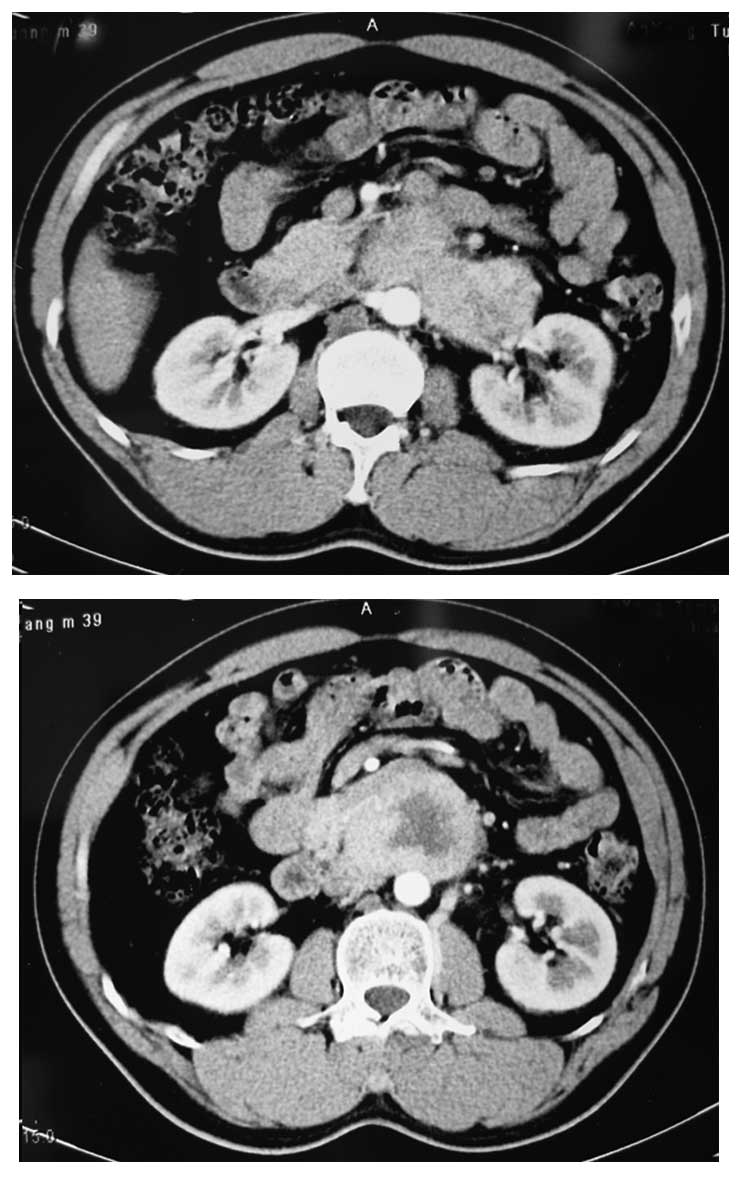
A 39-year-old male originally presented in 2007 with
complaints of upper abdominal pain accompanied with pain radiating
from the waist. In light of this, an abdominal computed tomography
(CT) scan was performed, which demonstrated a mass containing a
necrotic part at its center with peripheral enhancement and
dimensions of 5.3x4.8 cm. The tumor was located at the anterior
part of the interaortocaval region and adhered to the left kidney
pedicle at its base and to the body of the pancreas at the top
(Fig. 1). The case was suspected to
be a lymphoma and the patient was treated with chemotherapy for 2
months. However, the results of chemotherapy were disappointing.
Therefore, the patient was transferred to the Cancer Institute and
Hospital of the Chinese Academy of Medical Sciences, Beijing,
China. Fine needle aspiration of the mass was suggestive of
neuroendocrine tumor originating from the pancreas or adrenal
gland.
For surgical treatment, the patient was admitted to
the Department of Oncosurgery, Anyang Tumor Hospital, Henan, China.
The patient denied symptoms of diarrhea, vomiting, flushing and
palpitations. The patient’s past medical history was insignificant.
No abnormal findings were observed on physical and laboratory
examinations including tumor markers. Therefore, under the
diagnosis of neuroendocrine tumor with unknown malignant potential,
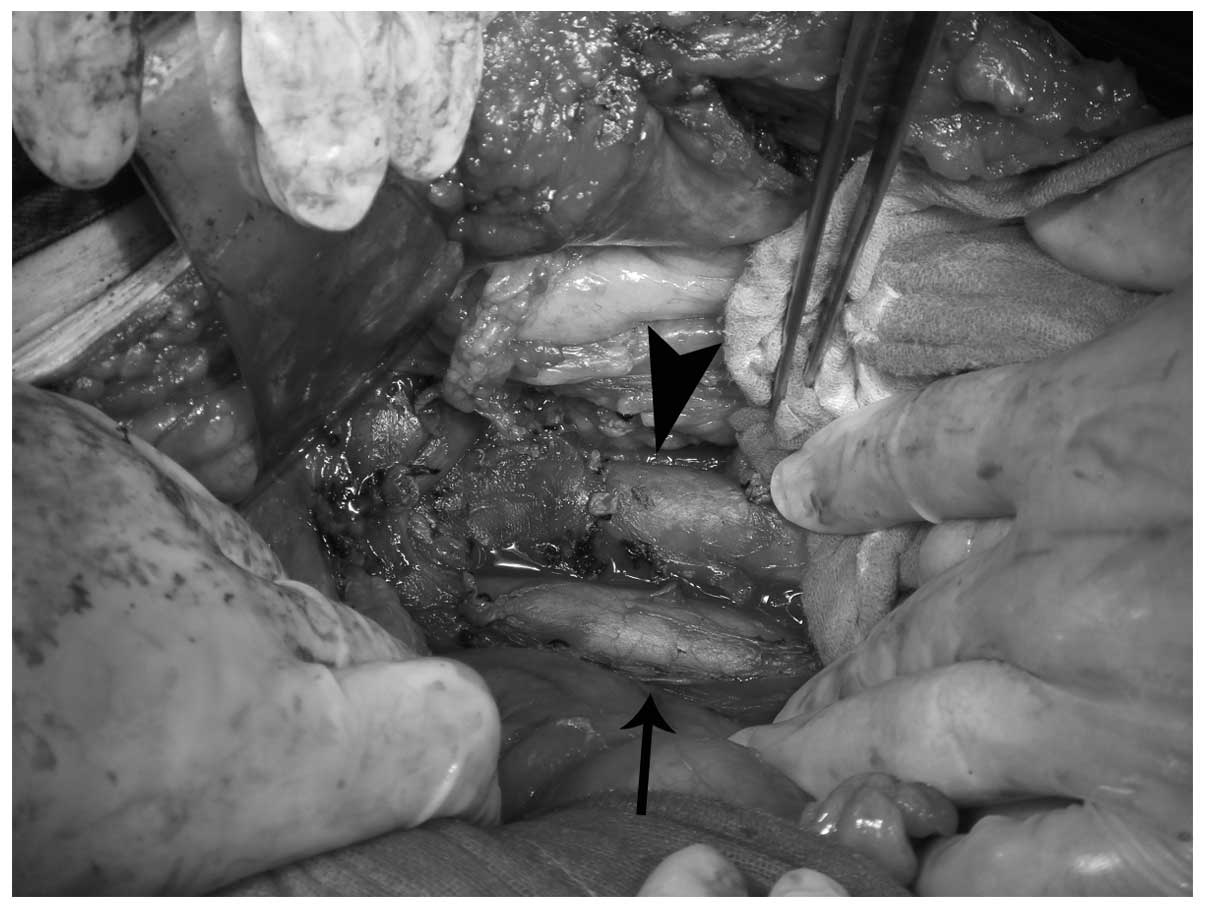
the patient underwent surgical exploration. During surgery, we
observed two retroperitoneal tumors situated at the anterior part
of the anteraortocaval region and the left kidney pedicle, inferior
to the pancreas. A separate lesion was identified in the iliac
bifurcation. However, three masses remained together with a clear
borderline. Unexpectedly, the patient became hypertensive with a
systolic blood pressure reaching 200 mmHg during initial
manipulation of the tumor. Paraganglioma was considered. The blood
pressure was rapidly controlled and the tumor was completely
resected (Figs. 2 and 3).
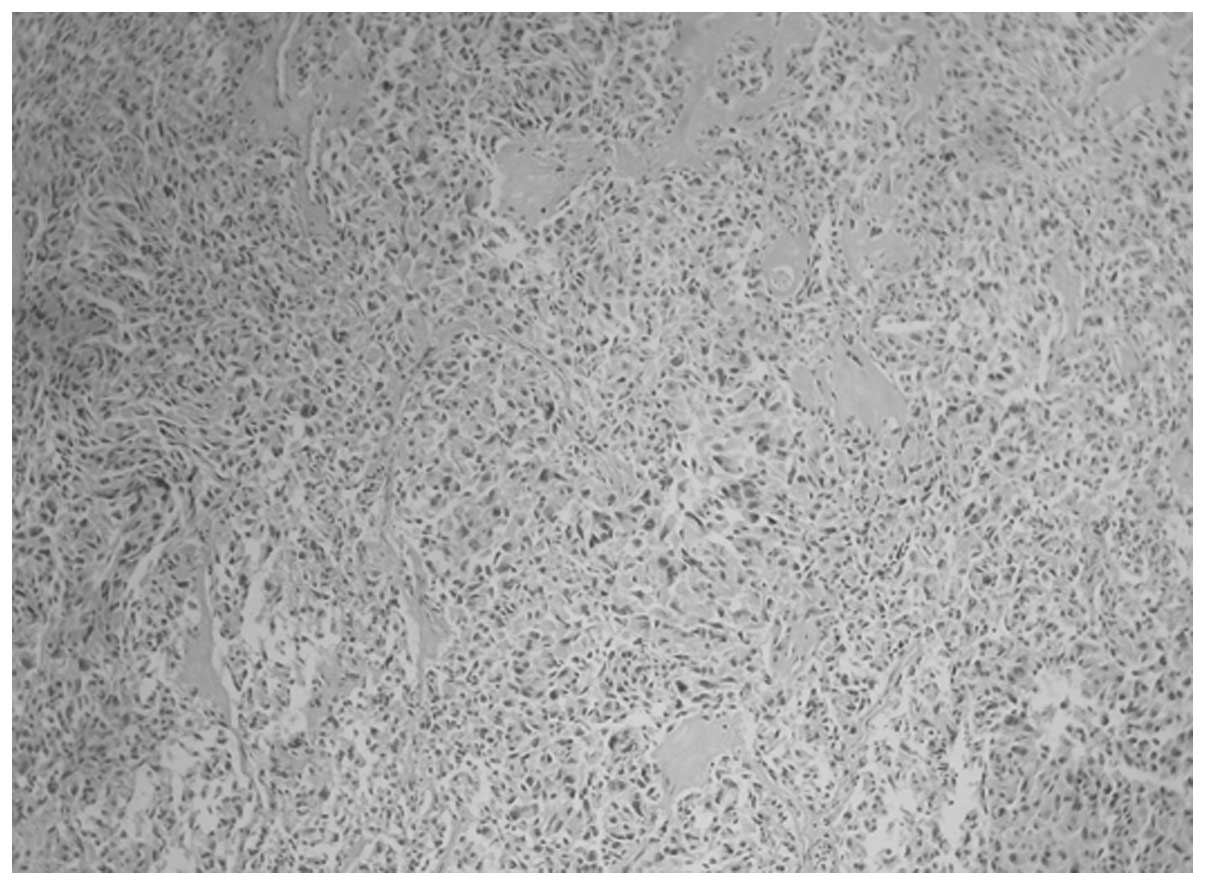
The pathological examination of the specimen
confirmed paraganglioma (Fig. 4).
The patient’s postoperative convalescence was unremarkable, and he
was discharged 10 days after the operation. Thereafter, he has been
followed up. Four years after the operation, the patient remains
asymptomatic and free of disease.
Discussion
Pheochromocytoma are rare endocrine tumors derived
from the neural crest in chromaffin tissue. They are found in the
adrenal medulla, carotid and aortic bodies, organs of Zuckerkandl
and other unnamed paraganglia occurring in the distribution of the
sympathetic and parasympathetic nerves. According to the proposal
offered by Pick in 1912, intra-adrenal chromaffin tumors were named
pheochromocytomas and all extra-adrenal chromaffin tumors were
termed paragangliomas, as described in a previous study (4). However, according to Boedeker et
al (5) the term paraganglioma
should only be used for tumors of neural crest origin that develop
in the head and neck. Although no definite classification of
paragangliomas has been made, paragangliomas can be classified as
being either ‘functional’ or ‘non-functional’, with 15–24% being
functional, and also by the presence of accompanying clinical
symptoms, including hypertension, hyperhidrosis and hyperglycemia,
which are characterized by the secretion of catecholamines
(6). The clinical symptoms vary
according to the amount of catecholamines released. Observable
clinical effects are only obtained if the tumor secretes a
sufficient quantity of catecholamines. However, circulating
catecholamine levels do not have a strong correlation with the
degree of hypertension in paraganglioma. It is considered that 30%
of functional paraganglioma patients have normal blood pressure
(7). The possible reasons for this
have been explained by Agarwal et al (8). In our study, the patient had normal
blood pressure and did not receive a metanephrine examination, with
a diagnosis of retroperitoneal tumor. However, the blood pressure
rose intraoperatively upon touch and mobilization of the tumor.
Once the tumor was removed, the patient’s blood pressure fell.
Histopathology revealed a paraganglioma.
Paragangliomas occur from the upper cervical region
to the pelvis, parallel to the autonomic nervous system. Of these
tumors, 85% are located in the abdomen, usually in the perinephric
and paraaortic spaces. They do not usually invade between the
abdominal aorta and inferior vena cava (9). The incidence of multicentricity of
paragangliomas has been reported as 15–24% in the literature
(10). In the case described here,
a dumbbell-shaped tumor was located at the anterior part of the
interaortocaval region and the left kidney pedicle. A separate
lesion was found in the iliac bifurcation.
It is difficult to make an accurate preoperative
clinical diagnosis of paraganglioma unless there are overt symptoms
related to excess catecholamine secretion. With the advancement of
imaging, contrast-enhanced abdominal CT, MRI and
metaiodobenzylguanidine (MIBG) are useful for diagnosis, location
and delineation of multiple tumors (3). However, no imaging feature unique to
abdominal silent paragangliomas has been found. A definitive
diagnosis of paragangliomas may be reached only by histological and
immunohistochemical evaluation.
As far as the treatment of paragangliomas is
concerned, the best choice is complete surgical resection since
these tumors are potentially malignant. However, it is important to
note that for those with functional paragangliomas, the tumor’s
ability to produce catecholamines may cause abrupt changes in the
blood pressure, which may cause an abnormal cardiac rhythm and even
asystole. Thus, surgery may induce life-threatening complications
as mentioned above. Though pre-medication of symptomatic patients
with positive biological tests has been recommended, the treatment
strategy remains unclear when the patient is asymptomatic and has
low catecholamine levels. In this study, the patient did develop a
hypertensive reaction during surgery although he was asymptomatic.
Only two such cases were found in the literature and those were
isolated paragangliomas (11,12).
In conclusion, paraganglioma is a rare type of
tumor, particularly asymptomatic functional multiple paraganglioma,
with limited cases reported. Recognition of paraganglioma as a
cause of an abdominal mass is essential. Complete surgical
resection is necessary for treatment and histological
assessment.
Acknowledgements
This study was supported by Grants
from the National Natural Science Foundation of China (no.
81071960) and New Teacher Foundation of the Ministry of Education,
China (no. 20100101120129).
References
|
1.
|
A KunitzS PahlP PodrabskyE WardelmannI
SturmLarge paraganglioma of the abdominal cavity: A case report and
review of the
literatureOnkologie33377380201010.1159/00031574920631484
|
|
2.
|
G SangsterD DoC PreviglianoB LiD LaFranceM
HeldmannPrimary retroperitoneal paraganglioma simulating a
pancreatic mass: A case report and review of the literatureHPB
Surg2010645728201010.1155/2010/64572821188160
|
|
3.
|
T YamaguchiM TadaH TakahashiR KagawaR
TakedaS SakataAn incidentally discovered small and asymptomatic
para-aortic paragangliomaEur Surg
Res401418200810.1159/00010761617717420
|
|
4.
|
GI DisickMA PaleseExtra-adrenal
pheochromocytoma: Diagnosis and managementCurr Urol
Rep88388200710.1007/s11934-007-0025-5
|
|
5.
|
CC BoedekerHP NeumannC OffergeldW MaierM
FalcioniA BerlisJ SchipperClinical features of paraganglioma
syndromesSkull Base191725200910.1055/s-0028-1103123
|
|
6.
|
A KudohY TokuhisaK MoritaS HirakiS FukudaN
EguchiMesenteric paraganglioma: Report of a caseSurg
Today35594597200510.1007/s00595-004-2966-315976959
|
|
7.
|
M SvajdlerP BohusP ZávackýM Vol’anskáA
RepovskýE JuskanicováParaganglioma of the mesenterium: A case
reportCesk Patol43153156200718188923
|
|
8.
|
A AgarwalS GuptaAK MishraN SinghSK
MishraNormotensive pheochromocytoma: Institutional experienceWorld
J Surg2911851188200510.1007/s00268-005-7839-416091986
|
|
9.
|
MK DemiragH KahramanK ErzurumluO
DoyurganUA GoksuHT KeceligilInter-aorta-caval located tumor: A case
reportAnn Thorac Cardiovasc
Surg17310312201110.5761/atcs.cr.09.0149621697799
|
|
10.
|
DA GoldfarbAC NovickEL BravoRA StraffonJE
MontieR KayExperience with extra-adrenal pheochromocytomaJ
Urol14293193619892795745
|
|
11.
|
L Menassa-MoussaT SmayraC YaghiC AtallahB
AbboudM GhossainPheochromocytoma: A tumour not to be trustedANZ J
Surg79562563200910.1111/j.1445-2197.2009.04992.x19694670
|
|
12.
|
MS LowenthalPM SadowC RautEC
MetzlerIntraoperative diagnosis of a functional paraganglioma
presenting as a gastrointestinal stromal cell tumor (GIST)J Clin
Anesth215760200910.1016/j.jclinane.2008.06.02619232943
|