Introduction
Treatment for head and neck cancer is usually
performed using a combination of radiotherapy, chemotherapy and
surgery. Following surgery, patients are often left with large
defects in the craniofacial region, with reduced sensory and motor
function in several organ systems (1). Rehabilitation can be performed using
different grafting procedures and/or prosthetic techniques
(2,3). In this case report, the large
craniofacial defect was rehabilitated by a bone-anchored prosthesis
(1).
Case report
In 2002, a 54-year-old male sought care at different
public service centers with a one-year symptom of headaches on the
left side of the cranium, together with nausea and vomiting. He had
no previous history of disease. He was a retired person and was not
aware of any exposure to any hazardous drugs or chemical products
during his working life, although he had smoked for 30 years. At
clinical examination, he presented with rhinorrea and protrusion of
the left eye, although his vision was normal. However, after one
month the patient did not return for follow-up and to receive the
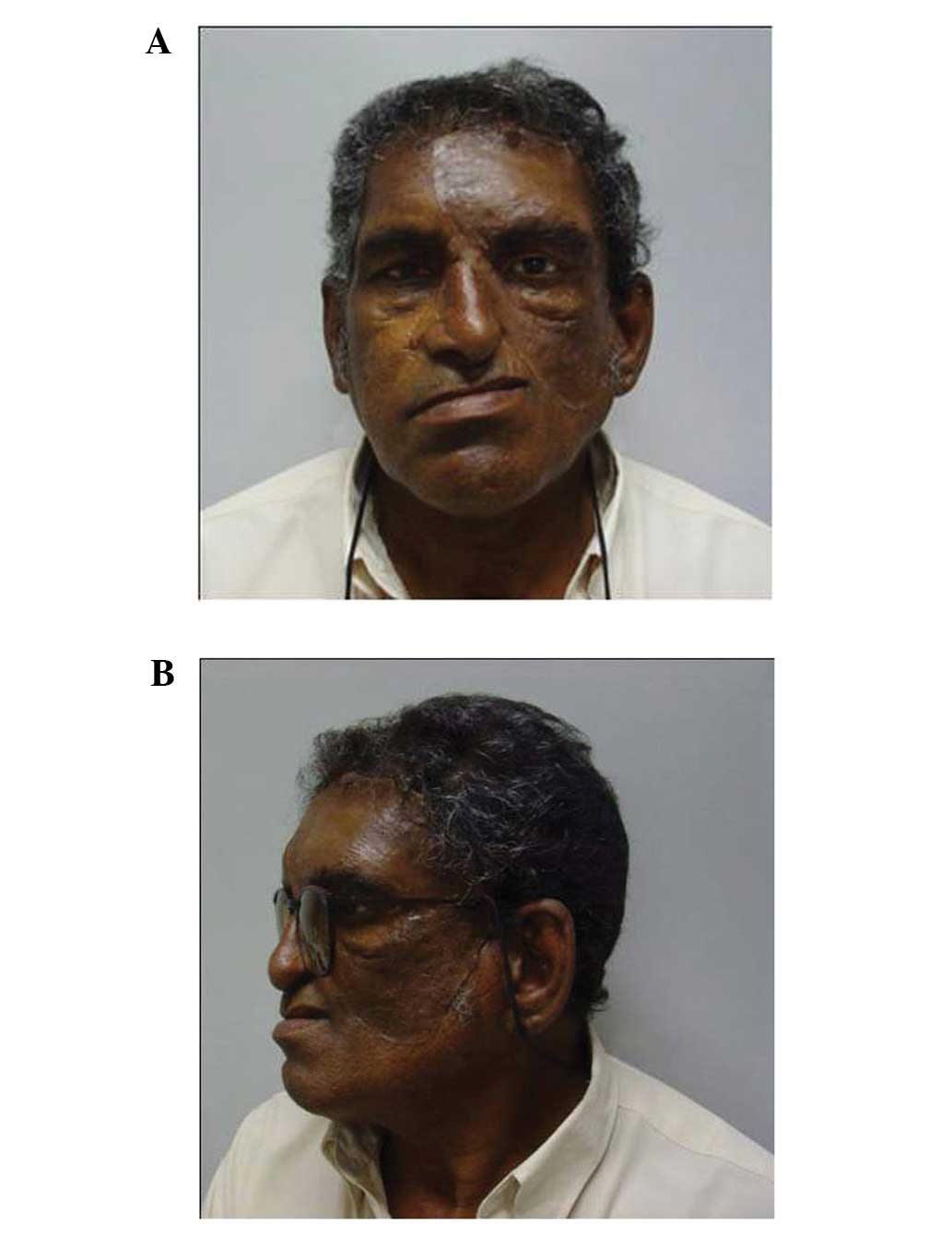
planned treatment. In June 2004, 2 years after the first
consultation, the patient returned with a large tumor on the left
side of the face that had developed extensively since the previous
examination (Fig. 1A). The initial
diagnosis had been a maxillary sinus inverted polyp, which in 10%
of cases transforms into a squamous cell carcinoma (4). After the period of extensive growth,
when the patient returned for consultation, the radiograph of the
maxillofacial region indicated an expansive process in the left
maxilla with destruction of the medial and lateral bone. Following
a biopsy, the histopathological results revealed a malignant
neoplasm which originated in the epithelial cells from the mucosa
of the maxillary left sinus. The malignant cells were thought to be
moderately differentiated. The tumor was invasive and metastases
were observed in certain cervical lymph nodes in the surrounding
areas. The final diagnosis was squamous cell carcinoma (Fig. 1A).
A CT scan, followed by an MRI scan, revealed a solid
tumor measuring 8.5×8.0×7.5 cm. As mentioned previously, the tumor
originated in the left maxillary sinus, where there was a squamous
cell carcinoma invading the orbit and destroying the anterior,
medial and posterior bone of the maxilla, orbital bone walls, nasal
cavity, pterygopalatine fossa, hard palate and masticatory muscles.
There was also a destruction of bone in the anterior cranial fossa,
and the tumor was advancing towards the brain tissue (Fig. 1B).
The tumor classification was: T4, N0, M0, stage 4.
Endoscopy of the nose, epipharynx and oral cavity also revealed a
large squamous cell carcinoma originating in the maxillary sinus
mucosa. Surgery was performed immediately. A pericoronal flap was
used to access the tumor and perform resection.
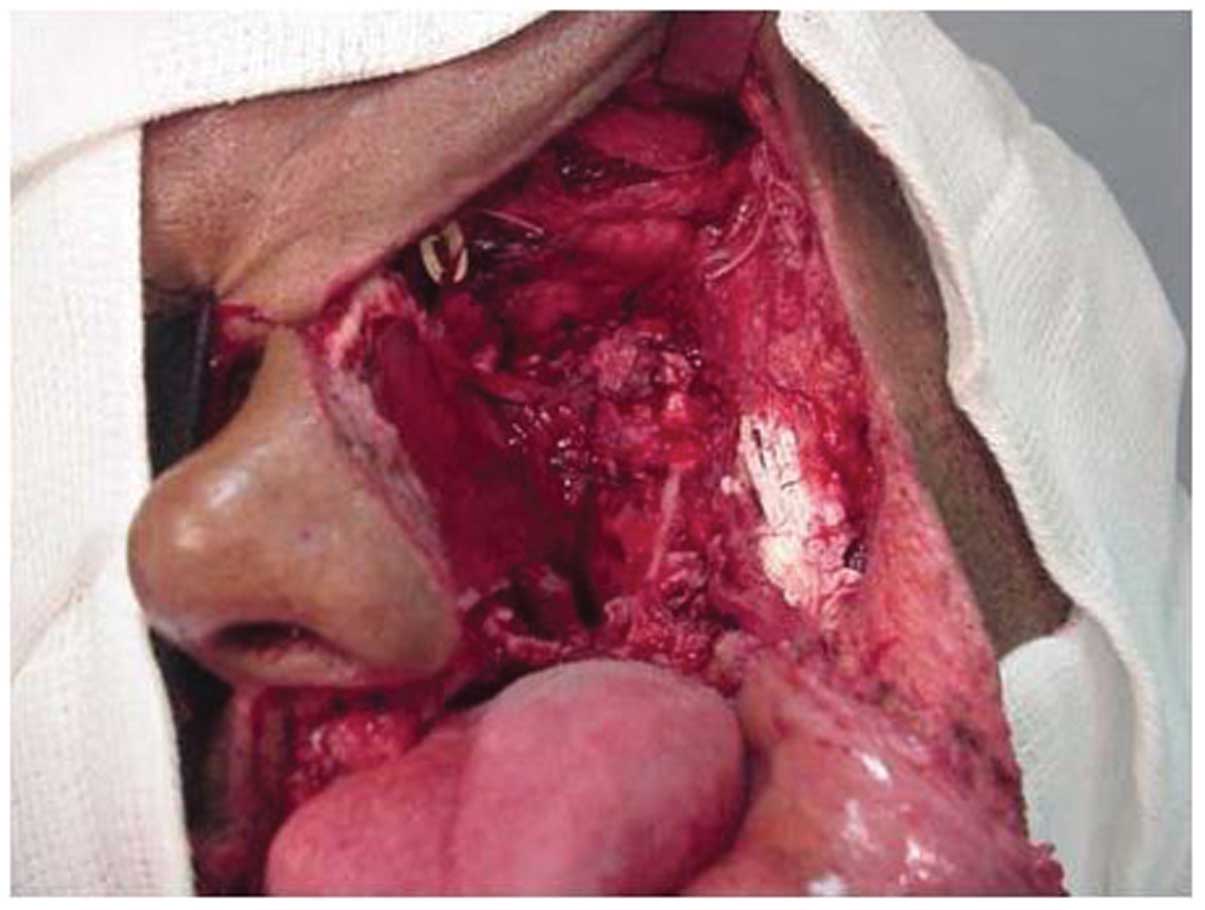
The tumor resection also included a maxillectomy of
the left side, removal of the left orbit and left nasal cavity, and
left side ethymoidectomy (Fig. 2).
The resection of all cervical lymph nodes on the tumor side was
also necessary, as metastasis was detected during the surgery and
also in the frozen biopsies. The left tumor cavity was closed with
skin flaps following resection but a perforation was left in the
hard palate. The surgical result was acceptable.
The patient was administered postoperative
radiotherapy 20 days after surgery. Radiation was performed with
Cobalt60 using a linear accelerator at a total dose of
60 Gy for 30 days. Postoperative chemotherapy was also administered
using cisplatin and 5-fluorouracil, in 3 cycles. The patient had
difficulties with swallowing, eating and drinking during the first
30 days. Following his recovery, a dental prosthesis was
constructed to close the nasopalatal perforation. This prosthesis
was replaced after the postoperative period, as the swelling of the
tissue had diminished. With the new prosthesis, the patient could
eat, swallow and speak without problems. He also regained weight in
the months following the treatment while wearing the full
dentures.
The patient experienced some side effects from the
radiotherapy, including dermatitis in the tumor cavity and mucosal
necrosis of the hard palate. After postoperative healing a facial
reconstructive treatment started. The patient was followed up
regularly for many years considering the possible tumor recurrence.
He was given full dentures with a maxillary obturator to allow him
to eat and speak with greater ease. When the patient remained
tumor-free after 5 years of follow-up, a new facial prosthesis was
planned, to be anchored by titanium implants fixed at the
remanescent bone. A CT scan with 3-D reconstruction was performed
to optimize treatment planning with extra-oral implants and a
special cosmetic prosthesis.
In 2009, the implant surgery was performed. This was
undertaken under general anesthesia. During the surgery, five
fixtures (Conexão Sistema de Proteses®, Sao Paulo,
Brazil), were installed, two in the frontal bone (6 mm in length),
one in the zygoma (7 mm) and two in the temporal bone (3 and 4 mm
in length, respectively; Fig. 3).
Following implant surgery and a healing period of 6 months, the
second phase of surgery was performed using abutment connection.
This surgery was also undertaken under general anesthesia. Standard
abutments 4 mm in length (Conexão Sistema de Proteses) were
attached to the osseointegrated implants and the subcutaneous
tissue thickness was reduced.
Following the implant surgery, there was a healing
period of three weeks, then preparation of the facial prosthesis
started. An impression of the tumor defect was taken and a model
was constructed from plaster of Paris. The prosthesis had an
acrylic base and was attached to the abutments with magnets. The
prosthesis was sculptured in wax and made in one piece. The edges
of the wax model were very thin to facilitate the acquisition of
the skin color, as well as to blend with the silicon prosthesis.
The final prosthesis was made of silicon [LSR-4340 Silicone
Elastomer, Rhodia (Factor II; Lakeside, AZ, USA)]. It was colored
by Functional Intrinsic II Silicone Coloring System (Factor II).
The right side of the patient’s face was used as the model for the
professional to achieve the appropriate colour. Rayon Fiber
Flocking (Factor II) was used to mimic minor blood vessels. The
cosmetic result was good (Figs. 4A and
B). The patient has been followed up since the fitting of the
prosthesis. He is now able to go out and socialize as before. His
functions are also good; he can speak, eat, chew and swallow
without problems and is a good singer. There was no recurrence of
the tumor until the last follow-up some months ago, and he is
wearing the prosthesis daily. Taking into account the treatment for
the malignant tumor as well as the prosthetic reconstruction, we
consider this to be a successful clinical case, particularly given
the extreme nature of the surgery and extent of the tissue
destruction. The prosthesis has allowed the patient to have almost
a normal life. In addition, the patient has survived for over 5
years, which is very uncommon.
Discussion
Head and neck cancer surgery may be mutilating,
leaving the patient with large craniofacial defects; however, such
surgery may be necessary in order to save the patient’s life.
Radiotherapy and chemotherapy contribute to cancer treatment, but
in certain cases these treatments may only be performed following
surgery, as they may affect tissues and alter the healing process
(1,2). Rehabilitation following cancer therapy
may therefore be compromising in several ways, and lead to
complications such as reduced healing capacity, wound infections,
graft necrosis and implant failures.
There are many aspects to be considered when
rehabilitating a cancer patient with large bone and soft tissue
defects. The patient may have a limited life expectancy due to the
cancer, as it may recur and/or metastasize. Also, the patient may
have other diseases that affect rehabilitation. The use of a facial
prosthesis allows inspection of the area to check for possible
cancer recurrence. Anchoring the prosthesis on extra-oral implants
is secure for the patient in comparison to anchoring it by glue
(1,3).
Rehabilitation is not only useful for improved
cosmetic appearance but also helps to promote function and social
rehabilitation (5). In a case such
as this, it was important to close the defect of the hard palate
with a dental prosthesis to improve speech, chewing and swallowing
function. Secondly, it was important to cover the frontal part of
the brain with the facial prosthesis. This can be done in several
ways; for example, by bone grafting or by covering the defect with
a titanium or acrylic plate. By utilizing modern techniques for 3-D
imaging and rapid prototyping, well-fitting plates can be
constructed and implanted (4).
Difficult cases such as the one presented here are
rare and in such cases rehabilitation should not be standardized
but should be planned and performed individually (6). When there is sufficient bone left in
the region, extra-oral osseointegrated implants may be used to
improve the retention of the facial prosthesis. If there is
insufficient bone, different grafting procedures may be performed
to correct the defect (4). One of
the advantages of the prosthetic solution is that it allows the
possibility to inspect the tumor cavity in order to check for
possible future tumor recurrences (7). If such a recurrence occurs, it is
necessary for the patient to undergo complementary treatment for
the tumor. If a patient has been tumor-free for many years, as
happened in the present case, he/she is not disqualified from other
rehabilitation procedures, although this is very uncommon.
Currently, alternatives to reconstructive surgery
and prosthetic rehabilitation could be achieved by partial or total
facial transplantation. A number of cases have been identified in
the last five years, some of which have been published (4). The long-term outcome of these
techniques is yet not clear, and the possible side effects from the
postoperative immunosuppressants are also not known. However, a
patient that has been rehabilitated with bone-anchored prosthesis
is not excluded from receiving a future facial transplantation or
grafting procedure.
References
|
1.
|
P GentileF NicoliR CarusoG GravanteV
CervelliAlternative strategy to reconstruct the nose after
excision: extra-oral implant anchored to boneBr J Oral Maxillofac
Surg475051200910.1016/j.bjoms.2008.03.021
|
|
2.
|
A MüllerKG KrishnanE UhlG MastThe
application of rapid prototyping techniques in cranial
reconstruction and preoperative planning in neurosurgeryJ Craniofac
Surg14899914200314600634
|
|
3.
|
J WolfaardtG WilkesG GranströmCraniofacial
reconstructionThe Osseointegration Book. From Calvarium to
CalcaneusP-I BrånemarkQuintessence Publishing
CoChicago3874182005
|
|
4.
|
JT LeeS BhutaDJ CastroIsolated inverting
papilloma of the sphenoid
sinusLaryngoscope1134144200310.1097/00005537-200301000-0000812514380
|
|
5.
|
RE GliklichMF RoundsML CheneyMA
VarvaresCombining free flap reconstruction and craniofacial
prosthetic technique for orbit, scalp, and temporal
defectsLaryngoscope108482487199810.1097/00005537-199804000-000049546256
|
|
6.
|
G GranströmL AnderssonKE KahnbergMA
PogrelCompromized wound healingOral and Maxillofacial SurgeryL
AnderssonKE KahnbergMA PogrelWiley and Sons1711762010
|
|
7.
|
O Guntinas-LichiusOutcomes 18 months after
the first human partial face transplantationN Engl J
Med3587980200818480214
|