Introduction
Hepatocellular carcinoma (HCC) is among cancers with
the poorest outlook, with fewer than 12% of all patients surviving
at five years (1). Primary liver
cancer most often emerges as a complication of chronic liver
disease, specifically cirrhosis. In western countries, the most
common cause of cirrhosis is presently chronic hepatitis C virus
(HCV) infection and non-alcoholic fatty liver disease (NAFLD) is
emerging as a primary risk factor due to the epidemic of obesity
(2). In a population with
cirrhosis, the most common clinical sequela is HCC (3). The early detection of HCC markedly
improves outcome (4). While the
risk factors for patients at the highest risk for developing HCC
are well characterized, the early detection of liver cancer remains
a challenge. The current screening tools of ultrasonography and
measurement of α-fetoprotein (AFP) in the blood have limitations
(5,6). In clinical practice, AFP is not
elevated in a significant number of patients with HCC (7). While the serological AFP blood test is
non-invasive, inexpensive and reproducible, screening programs that
utilize the test suffer from limitations in this marker’s
sensitivity and specificity. The poor sensitivity of AFP explains
its absence from the AASLD practice guidelines as a test
recommended for screening of HCC (8). This substandard sensitivity underlines
the need for a biomarker that is able to detect HCC at an early
stage.
The immune system employs various defense mechanisms
to inhibit cancer proliferation. However, a hallmark of cancer is
the ability to exploit these defenses and ultimately eclipse tumor
immunity (9). We have identified
soluble CD25 (sCD25) as an immune factor that is part of the
immune-suppressive network of HCC with potential promise as a
biomarker for HCC. sCD25 is produced after proteolytic release from
the membrane-bound α-subunit (CD25) of the interleukin (IL)-2
receptor. When CD25 is present on the T-cell membrane, together
with the β and γ chains it forms the high-affinity IL-2 receptor
that allows optimal IL-2 signaling for T-cell activation and
proliferation (10). We have
previously shown that the level of sCD25 in the serum of patients
with HCC is directly correlated with the degree of tumor burden
(11). In addition to the
correlation with HCC burden, sCD25 also has novel functional
properties with an ability to inhibit, in a dose-related manner,
antitumor T-cell responses. The release of sCD25 with its
immune-inhibitory properties is another level of immune regulation
involved in HCC development and progression (12–14).
In the present study, we evaluated the correlation
between the serum level of sCD25 and liver pathology using a
well-defined cohort of patients with HCC and patients with advanced
liver fibrosis. We hypothesized that sCD25 has the potential to be
an effective biomarker for the presence and early detection of HCC.
We determined the level of sCD25 in healthy subjects (NCs), disease
controls (DCs) with advanced fibrosis and patients with HCC. We
then determined the sensitivity and specificity of sCD25 in order
to distinguish patients with HCC from controls with advanced
fibrosis and cirrhosis. We also evaluated the efficacy of sCD25 in
detecting early HCC. We concluded our study by revisiting the
connection between sCD25 level and tumor burden observed in our
previous study using this larger cohort of patients with HCC.
Materials and methods
Study population
The study protocol was approved by the University of
Florida Institutional Review Board and we obtained written informed
consent from all participants in the study. The study included 143
patients with HCC in the setting of cirrhosis, 61 liver DCs and 30
NCs. Cirrhosis in the HCC patients developed from various primary
etiologies (Table IB). The DC
etiologies included patients with chronic HCV or HBV infection,
chronic HCV- or HBV-related cirrhosis, HCV and HBV co-infection,
alcohol abuse, NAFLD and cryptogenic cirrhosis (Table IA). All DCs were evaluated for stage
of fibrosis with a liver biopsy and serum collection was performed
on the same day as the biopsy. Of the 61 DCs, 54 had cirrhosis and
these patients had a fibrosis stage ≥3 out of 6 (Table IA) (15). All DCs with cirrhosis and patients
with HCC enrolled in this study had well-compensated cirrhosis
compatible with Child-Pugh A classification. No patients had a
performance status >1 and the majority of HCC patients had a
performance status score of 0. Blood samples from gender- and
age-matched NCs (n=30; 15 males, 15 females) were obtained from the
local blood bank (Life South, Gainesville, FL, USA). HCC was
diagnosed according to the non-invasive radiological criteria per
the AASLD guidelines (7). The
staging of HCC was performed using the Barcelona Clinic Liver
Cancer (BCLC) staging system. Patients diagnosed with stage A HCC
had a single lesion <5 cm or 2–3 lesions <3 cm in size.
Multinodular lesions >5 cm were characteristic tumor features in
patients with stage B HCC. Macroscopic vascular invasion or
metastatic disease was established in patients with Stage C HCC
(16).
 | Table I.Baseline clinical characteristics of
HCC (n=143) and disease control patients. |
Table I.
Baseline clinical characteristics of
HCC (n=143) and disease control patients.
| A, Disease controls
(n=61) |
|---|
|
|---|
| Category | n (%), or mean
(range) |
|---|
| Age (years) | 55.9 (45–77) |
| Gender | |
| Male | 42 (68.90) |
| Female | 19 (31.15) |
| Ethnicity | |
| Caucasian | 53 (86.89) |
|
African-American | 5 (8.20) |
| Hispanic | 2 (3.28) |
| Asian | 1 (1.64) |
| Etiology | |
| Cryptogenic
cirrhosis | 2 (3.28) |
| EtOH
cirrhosis | 3 (4.92) |
| HBV | 1 (1.64) |
| HBV
cirrhosis | 1 (1.64) |
| HBV+HCV
cirrhosis | 1 (1.64) |
| HCV | 6 (9.84) |
| HCV
cirrhosis | 44 (72.13) |
| NAFL
cirrhosis | 3 (4.92) |
| AFP | |
| ≤400 ng/ml | 45 (97.83) |
| >400
ng/ml | 1 (2.17) |
| MELD score | |
| <10 | 40 (78.43) |
| ≥10 | 11 (21.57) |
| B, HCC patients
(n=143) |
|---|
|
|---|
| Category | n (%), or mean
(range) |
|---|
| Age (years) | 63.6 (30–92) |
| Gender | |
| Male | 113 (79.02) |
| Female | 30 (20.98) |
| Ethnicity | |
| Caucasian | 117 (81.82) |
|
African-American | 15 (10.49) |
| Hispanic | 8 (5.59) |
| Asian | 3 (2.10) |
| Etiology | |
| Adenoma | 4 (2.80) |
| Cryptogenic
cirrhosis | 19 (13.29) |
| EtOH
cirrhosis | 13 (9.09) |
| HBV
cirrhosis | 7 (4.90) |
| HCV
cirrhosis | 86 (60.14) |
| NAFL
cirrhosis | 13 (9.09) |
| PBC
cirrhosis | 1 (0.70) |
| HCC stagea | |
| A | 48 (33.57) |
| B | 45 (31.47) |
| C | 50 (34.97) |
| AFP | |
| <400
ng/ml | 96 (67.13) |
| >400
ng/ml | 47 (32.87) |
| MELD score | |
| <10 | 106 (74.13) |
| ≥10 | 37 (25.87) |
Within the group of DCs, 44 patients had HCV-related
cirrhosis confirmed by histopathology. The patients with confirmed
HCV-related cirrhosis were enrolled into our surveillance program,
received serial cross-sectional imaging every six months and had no
liver masses on enrollment and 12 months after enrollment. The
following clinical data were obtained for each HCC patient: age,
gender, ethnicity, etiology of HCC, BCLC stage, AFP level and Model
for End-Stage Liver Disease (MELD) score. For the DCs, we obtained
age, gender, ethnicity, etiology of liver disease, MELD score and
AFP data for 46 of the 61 DC patients. AFP was measured in 46 of
the 61 DC patients. Laboratory hepatic function data needed for
MELD score calculation was not obtained for 10 of the 61 DCs at the
time of their enrollment
Serum preparation and sIL-2R ELISA for
sCD25 quantification
Whole blood samples were collected on the clinic
date when patients were diagnosed with HCC and processed for serum
isolation. Then, using sIL-2R ELISA (Bender MedSystems, Vienna,
Austria), we processed fresh samples for sCD25 in duplicate using
our previous approach (11).
Briefly, microtiter plates coated with anti-human sIL-2R antibody
were inculcated with serum containing sCD25 and subjected to
horseradish peroxide, a substrate solution that upon addition
induced a color change. The intensity of the colored product was
directly proportional to the level of sCD25 present in each well.
Plates were read at 450 nm using the SpectraMax 190 reader
(Molecular Devices, Sunnyvale, CA, USA). Measurements of sCD25
above the upper limit of the calibration range (20,000 pg/ml) were
diluted by half using buffer from the manufacturer.
Statistical analysis
Data for sCD25 and AFP levels are expressed as box
plots with medians ± SD. Receiver operator characteristic (ROC)
curves with respective points of maximal accuracy for sensitivity
and specificity were generated to determine biomarker performance.
The multiple regression test was used to evaluate the correlation
between clinical parameters and sCD25 level. We used the
Mann-Whitney U test to assess the significance of group differences
in the level of sCD25. Spearman’s rank correlation coefficient was
used to examine the correlation between HCC stage and the level of
sCD25. P<0.05 was considered to indicate a statistically
significant result. Statistical data were analyzed using MedCalc
version 11.5.1.0 (MedCalc Software, Mariakerke, Belgium).
Results
Clinical characteristics of HCC patients
and DCs
In our study, the majority of HCC patients were male
(79%) and Caucasian (82%). African-Americans, Hispanics and Asians
were less common (Table I). A
near-equal distribution of patients was present across all stages
of HCC, with 48 patients having stage A disease (early HCC), 45
patients being in the stage B subset (intermediate HCC) and 50
patients having stage C cancer (advanced HCC). The average age of
the HCC patients was 63.6 years. Of the HCC patients, 60% had
chronic HCV infection, making HCV the predominant etiology of their
liver disease. Other primary causes of HCC included alcohol-related
cirrhosis (n=13), chronic HBV infection (n=7) and
NAFLD/non-alcoholic steatohepatitis (NASH; n=13). The majority of
HCC patients (97%) had a MELD score <15. Most HCC patients
(67.13%) had an AFP level <400 ng/ml. For the DCs, the main
etiology of their liver disease was chronic HCV infection and
nearly all patients had an AFP level <400 ng/ml (Table IB).
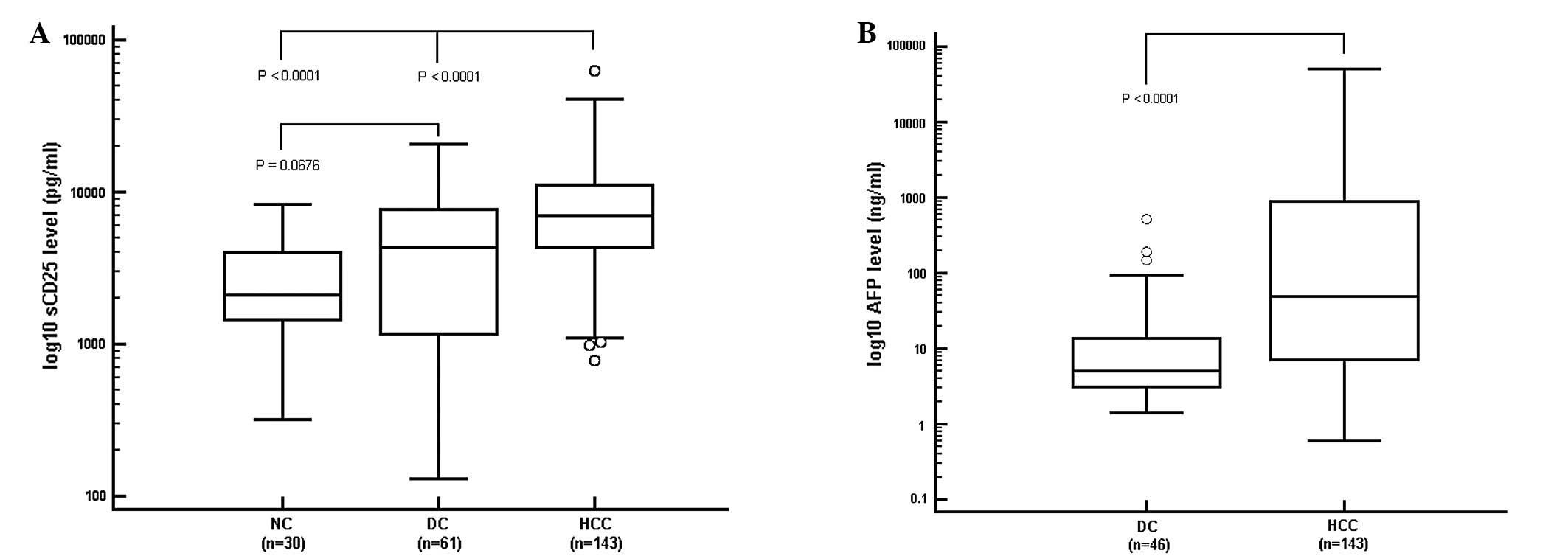
sCD25 levels in HCC patients
The serum levels of sCD25 were detected at a
significantly higher level in HCC patients than NCs and DCs
(Fig. 1A). The median value of
sCD25 in the HCC patients (6,955 pg/ml) was significantly higher
than that of the DCs and NCs (P<0.0001). The median level of
sCD25 in the DC group (4,310 pg/ml) was higher than that in the NCs
(2,098 pg/ml), but the difference was not significant (P=0.0676).
The levels of sCD25 of HCC patients were not correlated with age,
gender or MELD score.
AFP levels in HCC patients
AFP levels were obtained for DC and HCC patients but
not the NCs. The difference between the median AFP level in HCC
patients (49.4 ng/ml) and that in DCs (5.3 ng/ml) was significant
(P<0.0001; Fig. 1B). For the DC
and HCC patients, there was no correlation between the AFP levels
and age, gender or MELD score.
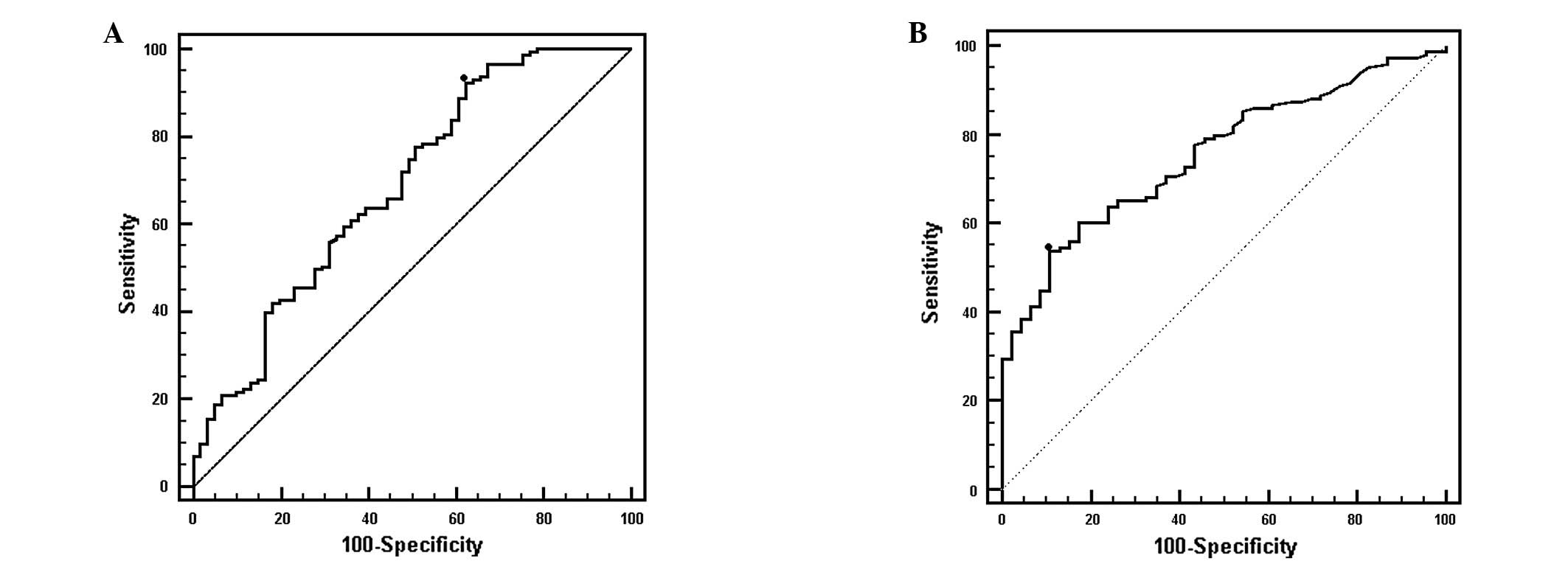
Utility of sCD25 in predicting HCC
presence
After showing that sCD25 was able to differentiate
HCC from controls with cirrhosis (P<0.0001), we then determined
its capacity to detect the presence of HCC. This analysis showed
that at a cut-off value of 2,180 pg/ml, sCD25 had a sensitivity of
92.3% and a specificity of 37.7% for detecting HCC (Fig. 2A). By comparison, AFP had a
sensitivity of 53.8% and a specificity of 86.8% at a cut-off value
of 32.3 ng/ml. The area under the curve (AUC) values for sCD25 and
AFP were 0.685 and 0.755, respectively. At 20 ng/ml, the
recommended clinical cut-off value for AFP used in clinical
practice, the sensitivity of AFP was 60.1% and the specificity was
81.8% (AUC=0.733).
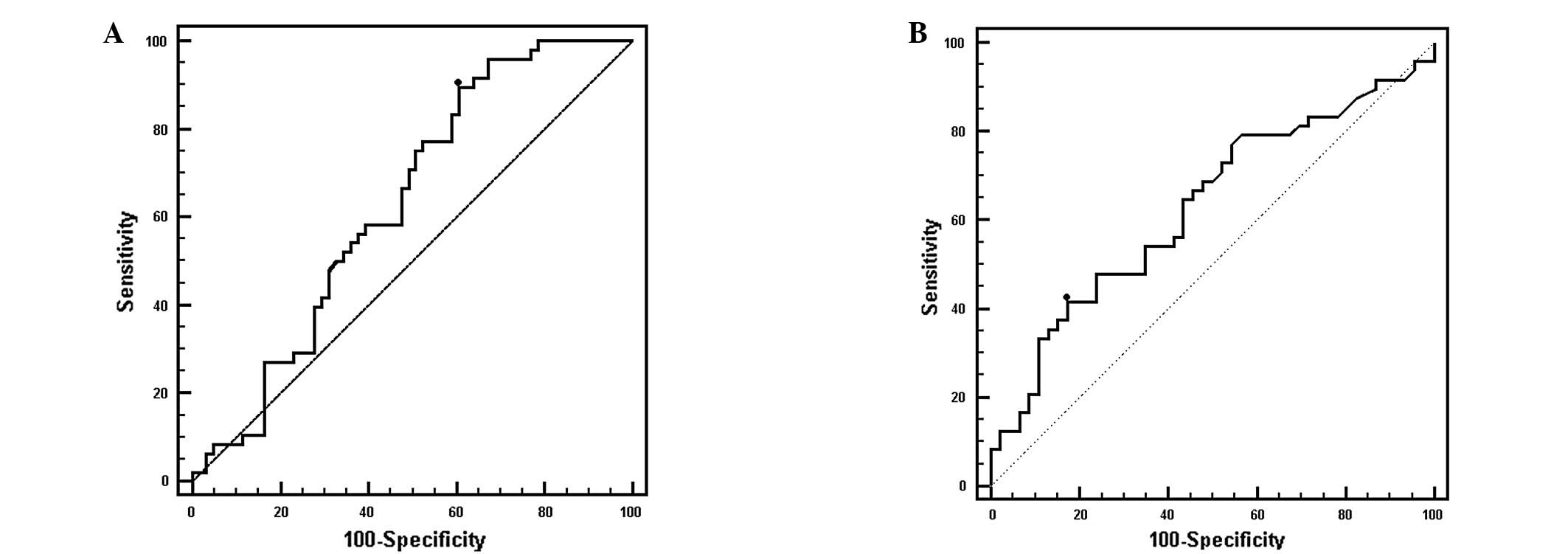
sCD25 as a marker for early stage
HCC
We evaluated the performance of sCD25 in detecting
early HCC by comparing the level of sCD25 in patients with BCLC
stage A HCC with the sCD25 responses of DC patients (Fig. 3A). In this ROC analysis, an optimal
cut-off value of 2,859 pg/ml for sCD25 had a sensitivity of 89.6%
and a specificity of 39.3% with an AUC of 0.630 (P<0.0001). By
comparison, at a cut-off value of 20 ng/ml, AFP had a sensitivity
of 41.7% and a specificity of 82.6% (AUC=0.630, P=0.0257; Fig. 3B).
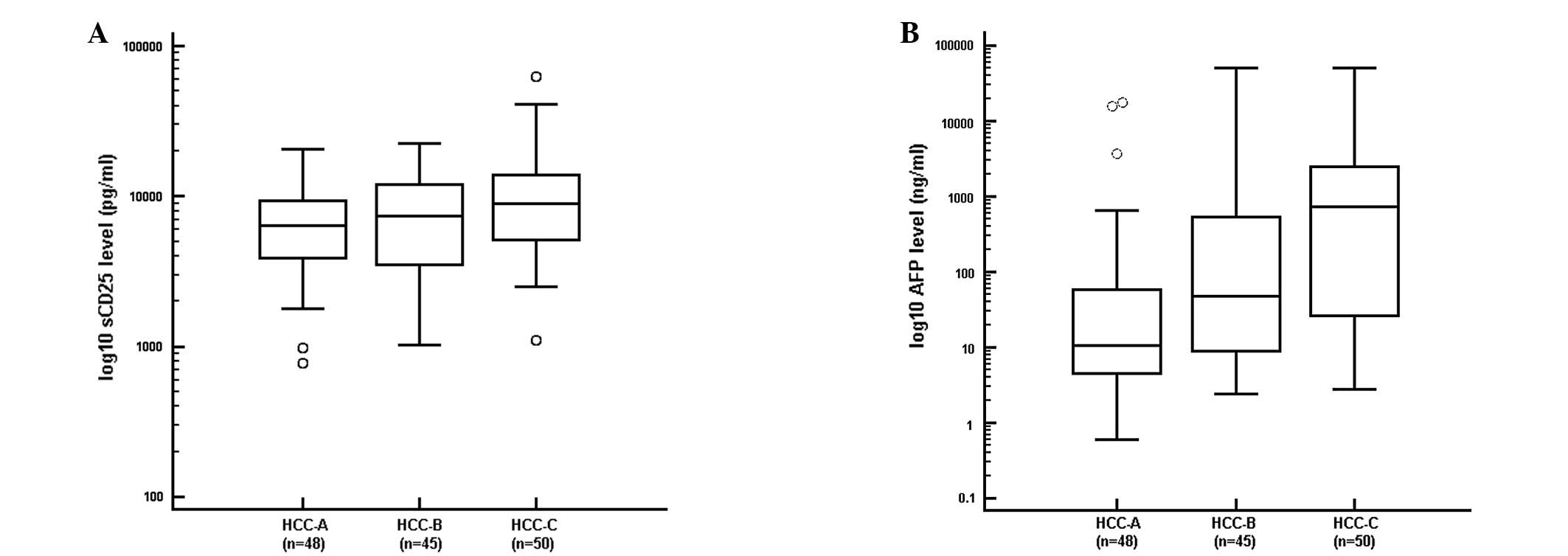
Correlation between tumor burden and
sCD25 level
We evaluated the correlation between levels of sCD25
and tumor burden. We also examined the correlation between AFP and
tumor burden. We observed a progressive elevation in the level of
sCD25 with increasing HCC stage (R= 0.213, P<0.0160). The
patients with early stage HCC (stage A) had the lowest median level
of sCD25 (6,339 pg/ml), while patients with multi-nodular HCC
(stage B) had an intermediate median level of sCD25 (7,365 pg/ml).
The patients with advanced HCC (stage C) had the highest median
level of sCD25 (8,889 pg/ml; Fig.
4A). We also found a strong positive correlation between AFP
level and stage of HCC (Fig. 4B;
R=0.513, P<0.0001).
Using the cut-off value of 2,859 pg/ml for sCD25 and
20 ng/ml for AFP, we evaluated the correlation between sCD25 and
size of HCC in patients with early HCC. In this analysis, we
divided the subset of HCC patients with early HCC into patients
with a single small tumor <2 cm and patients with single tumors
<5 cm in size. In this analysis, sCD25 retained a high
sensitivity in those patients with the smallest lesions (<2 cm)
and in patients with lesions <5 cm (Table II). We also found that the
sensitivity for AFP was low and increased with size of HCC.
 | Table II.Correlation between sCD25 and stage A
HCC tumor size. |
Table II.
Correlation between sCD25 and stage A
HCC tumor size.
| Tumor size
(cm) | Parameter | sCD25a | AFPb |
|---|
| <2 | Sensitivity | 91.7 | 33.3 |
| Specificity | 41.0 | 76.1 |
| <5 | Sensitivity | 92.1 | 47.4 |
| Specificity | 39.3 | 82.6 |
Discussion
Given that the majority of HCC patients present with
advanced disease, there is a pressing need for an effective
biomarker that detects the presence and early stages of HCC at a
better capacity than AFP. In the present study, we found that sCD25
effectively distinguished HCC patients from healthy and DC
subjects. The levels of sCD25 in HCC patients were significantly
higher than those in NCs and DCs with advanced liver fibrosis. This
analysis found that sCD25 possesses a sensitivity of 92% at a
cut-off value of 2,180 pg/ml for the presence of HCC and warrants
additional investigation as a potential screening test.
Furthermore, sCD25 also retained this high sensitivity (90% at a
cut-off value of 2,899 pg/ml) for detecting HCC in a subset of
patients with early stage HCC, highlighting its potential use as a
screening tool in those at high-risk for HCC. When comparing sCD25
with AFP, we found that sCD25 has a higher sensitivity than AFP in
detecting the presence of HCC, particularly in patients with early
HCC. We also observed a positive correlation between the level of
sCD25 and the degree of tumor burden of HCC, with levels of sCD25
progressively increasing from early (stage A) to advanced stage
(stage C) HCC. This correlation was consistent with our previous
study (11), which revealed a
positive correlation between serum levels of sCD25 and tumor
burden. These findings suggest that the measurement of serum levels
of the immune marker sCD25 may improve earlier detection of HCC and
could potentially be a useful novel prognostic marker.
A number of serum markers have been evaluated to
detect HCC, including AFP, lectin-bound AFP (AFP-L3%) and des-γ
carboxy-prothrombin (DCP). The most commonly used sero-logical
assay to detect HCC is the blood test for AFP. However, AFP at the
clinically recommended cut-off value of 20 ng/ml suffers from poor
sensitivity (17). Studies have
suggested DCP and AFP-L3% as potential biomarkers for HCC,
particularly when used in a complementary fashion (18–20).
However, a multicenter phase II biomarker study, using a total of
836 patients with 50% of the patients being controls with cirrhosis
and 50% having HCC, showed the sensitivity of 60% for AFP to be
better than those of DCP and AFP-L3% (21). For those patients with early stage
HCC, the sensitivity of 65% for AFP was more sensitive than DCP and
AFP-L3%. Studies that combined the three markers AFP-L3%, DCP and
AFP have failed to show a substantial improvement in sensitivity,
even when using a cohort of HCC patients with large, unresectable
tumors (22). When patients with
early HCC were analyzed from a nested case-control study of 39 HCC
cases developing during the randomized Hepatitis C Antiviral
Long-term Treatment (HALT-C) trial, the sensitivity dropped to 47%
for DCP and 61% for AFP (23).
Numerous studies have shown that the sensitivity of these markers
drops as a function of decreasing tumor size, highlighting an
insufficient sensitivity for these markers at detecting the onset
of cancer at its earliest stage (24–26).
The need to be able to detect HCC at its earliest stage was further
demonstrated in the HALT-C trial, which analyzed the serum levels
of AFP and DCP for 12 months prior to the diagnosis of HCC. DCP and
AFP had good specificities (94 and 75%, respectively), but
possessed markedly low sensitivities, of 47 and 43%, respectively.
In the present study, sCD25 was more sensitive than AFP in
distinguishing patients with early HCC from cirrhosis control
patients. Moreover, our study showed that AFP level was not
correlated with early stage HCC lesions smaller than 3 cm
(P=0.1148). This finding is consistent with the conclusions of
other studies (27) demonstrating a
lack of sensitivity of the AFP serological test when used in the
screening for early tumors.
While AFP had poor sensitivity in our study, it did
show a high specificity for both HCC presence and early HCC in
comparison to the low specificity of sCD25 in these analyses. The
inadequate specificity of sCD25 is a limitation that requires
further evaluation through the recruitment of a larger HCC cohort,
since an ideal biomarker should possess high sensitivity and
specificity. The addition of complementary markers to sCD25 should
also be considered, since this approach to screening may improve
the capacity of a test to detect cancer in its early stage.
AFP continues to be widely used but concern over its
poor performance as a marker has led to its exclusion as a
recommended test for screening patients at high risk for HCC in the
current practice guidelines from the AASLD (7,28,29).
Currently, the main screening strategy recommended is serial liver
ultrasonography. However, this screening modality is not being
effectively used since the majority of patients at the highest risk
for HCC development are not undergoing surveillance (30). Ultrasonography also poses
significant challenges related to availability and operator
experience in interpreting images from cirrhotic livers and obese
patients (31). The identification
of a novel biomarker for HCC that detects early cancer and is
capable of overcoming these limitations may improve surveillance
efforts and clinical outcomes.
While this study was not designed to evaluate the
influence of the etiology of underlying liver disease or other
clinical factors on sCD25, we did not identify a correlation
between clinical parameters and levels of sCD25 level. Most
importantly, our study controlled for underlying liver function by
enrolling only HCC patients with Child-Pugh A cirrhosis. Biases
were further eliminated through the blind implementation of
bioassay procedures. Our study demonstrated a dose-response
correlation between sCD25 level and tumor burden, suggesting its
potential use as predictor of prognosis at baseline. Future studies
analyzing sCD25 responses in samples obtained during a surveillance
program may provide further insight on the utility of sCD25 in
surveillance for early HCC detection.
We currently lack a reliable serum marker for the
early detection of HCC. In accordance with the phase-specific
biomarker standardization model delineated by Pepe et al, we
highlight the progress of our initial study using the immune marker
of sCD25 (32). Previously, we
assessed the performance of sCD25 in a small group (n=60) of HCC
patients. In the present study, we expanded our analysis to a
larger cohort of HCC patients (n=143) and again observed the
previously shown marked elevation of sCD25 in HCC patients in
comparison to the levels manifested in healthy controls and
controls with cirrhosis (11). Our
findings show that sCD25 distinguished HCC from appropriate
controls and that this marker identified the presence of HCC more
effectively than AFP, particularly in patients with early tumors.
The high sensitivity of sCD25 suggests it holds promise as a marker
for early HCC which is an area of unmet need. To further
characterize the utility of sCD25 in detecting early stages of HCC
tumor development, larger longitudinal and validation studies are
planned.
Acknowledgements
This study was supported by the NIH
KL2 University of Florida Clinical Translational Science Scholar
Award, NIH/NCRR award UL1RR029890 and NIH/NCI award K24CA139570.
The authors thank the participants of this study for their
dedication and commitment.
References
|
1.
|
HB El-SeragHepatocellular carcinomaN Engl
J Med36511181127201110.1056/NEJMra100168321992124
|
|
2.
|
SH CaldwellDM CrespoHS KangAM
Al-OsaimiObesity and hepatocellular
carcinomaGastroenterology127Suppl
1S97S103200410.1053/j.gastro.2004.09.02115508109
|
|
3.
|
G FattovichT StroffoliniI ZagniF
DonatoHepatocellular carcinoma in cirrhosis: incidence and risk
factorsGastroenterology127Suppl
1S35S50200410.1053/j.gastro.2004.09.01415508101
|
|
4.
|
LL WongWM LimmR SeverinoLM WongImproved
survival with screening for hepatocellular carcinomaLiver
Transpl6320325200010.1053/lv.2000.487510827233
|
|
5.
|
HB El-SeragJR KramerGJ ChenZ DuanPA
RichardsonJA DavilaEffectiveness of AFP and ultrasound tests on
hepatocellular carcinoma mortality in HCV-infected patients in the
USAGut60992997201110.1136/gut.2010.23050821257990
|
|
6.
|
S BenowitzLiver cancer biomarkers
struggling to succeedJ Natl Cancer
Inst99590591200710.1093/jnci/djk17417440159
|
|
7.
|
M ShermanCurrent status of α-fetoprotein
testingGastroenterol Hepatol (NY)71131142011
|
|
8.
|
J BruixM ShermanPractice Guidelines
Committee, American Association for the Study of Liver
DiseasesManagement of hepatocellular
carcinomaHepatology4212081236200510.1002/hep.20933
|
|
9.
|
Y NakamotoLG GuidottiCV KuhlenP FowlerFV
ChisariImmune pathogenesis of hepatocellular carcinomaJ Exp
Med188341350199810.1084/jem.188.2.3419670046
|
|
10.
|
NA CacalanoJA JohnstonInterleukin-2
signaling and inherited immunodeficiencyAm J Hum
Genet65287293199910.1086/30251810417270
|
|
11.
|
R CabreraM AraratM CaoHepatocellular
carcinoma immunopathogenesis: clinical evidence for global T cell
defects and an immunomodulatory role for soluble CD25 (sCD25)Dig
Dis Sci55484495201010.1007/s10620-009-0955-519714465
|
|
12.
|
B HoechstLA OrmandyM BallmaierA new
population of myeloid-derived suppressor cells in hepatocellular
carcinoma patients induces CD4(+)CD25(+)Foxp3(+) T
cellsGastroenterology135234243200818485901
|
|
13.
|
B ArunBD CurtiDL LongoElevations in serum
soluble interleukin-2 receptor levels predict relapse in patients
with hairy cell leukemiaCancer J Sci Am62124200010696734
|
|
14.
|
T ManshouriKA DoX WangCirculating CD20 is
detectable in the plasma of patients with chronic lymphocytic
leukemia and is of prognostic
significanceBlood10125072513200310.1182/blood-2002-06-163912446458
|
|
15.
|
RG KnodellKG IshakWC BlackFormulation and
application of a numerical scoring system for assessing
histological activity in asymptomatic chronic active
hepatitisHepatology1431435198110.1002/hep.1840010511
|
|
16.
|
JM LlovetC BrúJ BruixPrognosis of
hepatocellular carcinoma: the BCLC staging classificationSemin
Liver Dis19329338199910.1055/s-2007-100712210518312
|
|
17.
|
F TrevisaniPE D’IntinoAM
Morselli-LabateSerum alpha-fetoprotein for diagnosis of
hepatocellular carcinoma in patients with chronic liver disease:
influence of HBsAg and anti-HCV statusJ
Hepatol34570575200110.1016/S0168-8278(00)00053-211394657
|
|
18.
|
T SassaT KumadaS NakanoT UematsuClinical
utility of simultaneous measurement of serum high-sensitivity
des-gamma-carboxy prothrombin and Lens culinaris agglutinin
A-reactive alpha-fetoprotein in patients with small hepatocellular
carcinomaEur J Gastroenterol
Hepatol1113871392199910.1097/00042737-199912000-00008
|
|
19.
|
Y ShimauchiM TanakaR KuromatsuA
simultaneous monitoring of Lens culinaris agglutinin A-reactive
alpha- fetoprotein and des-gamma-carboxy prothrombin as an early
diagnosis of hepatocellular carcinoma in the follow-up of cirrhotic
patientsOncol Rep72492562000
|
|
20.
|
JA MarreroGL SuW WeiDes-gamma
carboxyprothrombin can differentiate hepatocellular carcinoma from
nonmalignant chronic liver disease in American
patientsHepatology3711141121200310.1053/jhep.2003.50195
|
|
21.
|
JA MarreroZ FengY WangAlpha-fetoprotein,
des-gamma carboxyprothrombin, and lectin-bound alpha-fetoprotein in
early hepatocellular
carcinomaGastroenterology137110118200910.1053/j.gastro.2009.04.00519362088
|
|
22.
|
BI CarrF KankeM WiseS SatomuraClinical
evaluation of lens culinaris agglutinin-reactive alpha-fetoprotein
and des-gamma-carboxy prothrombin in histologically proven
hepatocellular carcinoma in the United StatesDig Dis
Sci52776782200710.1007/s10620-006-9541-2
|
|
23.
|
AS LokRK SterlingJE EverhartHALT-C Trial
GroupDes-gamma-carboxy prothrombin and alpha-fetoprotein as
biomarkers for the early detection of hepatocellular
carcinomaGastroenterology138493502201010.1053/j.gastro.2009.10.03119852963
|
|
24.
|
S NakamuraK NousoK SakaguchiSensitivity
and specificity of des-gamma-carboxy prothrombin for diagnosis of
patients with hepatocellular carcinomas varies according to tumor
sizeAm J
Gastroenterol10120382043200610.1111/j.1572-0241.2006.00681.x16848811
|
|
25.
|
RK SterlingEC WrightTR MorganFrequency of
elevated hepatocellular carcinoma (HCC) biomarkers in patients with
advanced hepatitis CAm J
Gastroenterol1076474201210.1038/ajg.2011.31221931376
|
|
26.
|
AM Di BisceglieRK SterlingRT ChungHALT-C
Trial GroupSerum alpha-fetoprotein levels in patients with advanced
hepatitis C: results from the HALT-C trialJ
Hepatol43434441200516136646
|
|
27.
|
SK YoonNK LimS HaThe human cervical cancer
oncogene protein is a biomarker for human hepatocellular
carcinomaCancer
Res6454345441200410.1158/0008-5472.CAN-03-366515289352
|
|
28.
|
ME el-HouseiniMS MohammedWM ElshemeyTD
HusseinOS DesoukyAA ElsayedEnhanced detection of hepatocellular
carcinomaCancer Control12248253200516258497
|
|
29.
|
MF YuenCL LaiScreening for hepatocellular
carcinoma: survival benefit and cost-effectivenessAnn
Oncol1414631467200310.1093/annonc/mdg40014504044
|
|
30.
|
JA DavilaL HendersonJR KramerUtilization
of surveillance for hepatocellular carcinoma among hepatitis C
virus-infected veterans in the United StatesAnn Intern
Med1548593201110.7326/0003-4819-154-2-201101180-0000621242365
|
|
31.
|
B DanieleA BencivengaAS MegnaV
TinessaAlpha- fetoprotein and ultrasonography screening for
hepatocellular carcinomaGastroenterology127Suppl
1S108S112200410.1053/j.gastro.2004.09.02315508073
|
|
32.
|
MS PepeR EtzioniZ FengPhases of biomarker
development for early detection of cancerJ Natl Cancer
Inst9310541061200110.1093/jnci/93.14.105411459866
|