Introduction
Primary intracranial germ cell tumors (GCTs) are
associated with many unanswered questions due to their low
incidence (approximately 1.8–3.0% of all primary brain tumors)
(1). They include germinomas (65%),
teratomas (18%), embryonal carcinomas (5%), endodermal sinus tumors
(7%) and choriocarcinomas (5%) (2).
While germinomas may be cured by chemotherapy and/or radiotherapy,
non-germinatous malignant GCTs are highly resistant to standard
treatments, and their prognosis is extremely poor. Of these,
primary intracranial choriocarcinomas (PICCCs) are extremely rare.
They have the worst prognosis and high early mortality rates,
particularly due to tumor hemorrhage within the first year
(2,3). The clinical and biological behavior of
PICCCs remains to be fully elucidated and, to date, no therapeutic
strategy has been established. We successfully treated a case of
PICCC with synchronous chemotherapy and radiotherapy followed by
three consecutive chemotherapy courses without surgery. The study
was approved by the ethics committee of Soonchunhyang University
Bucheon hospital, Bucheon, Korea. Written informed patient consent
was obtained from the patient.
Case report
A 19-year-old male patient presented with a two-week
history of diplopia, headache, nausea and vomiting. Neurological
examination revealed visual disturbance, bilateral hearing loss,
bilateral sixth nerve palsy, left skew deviation, downgaze
limitation and clockwise torsional nystagmus on the left upgaze.
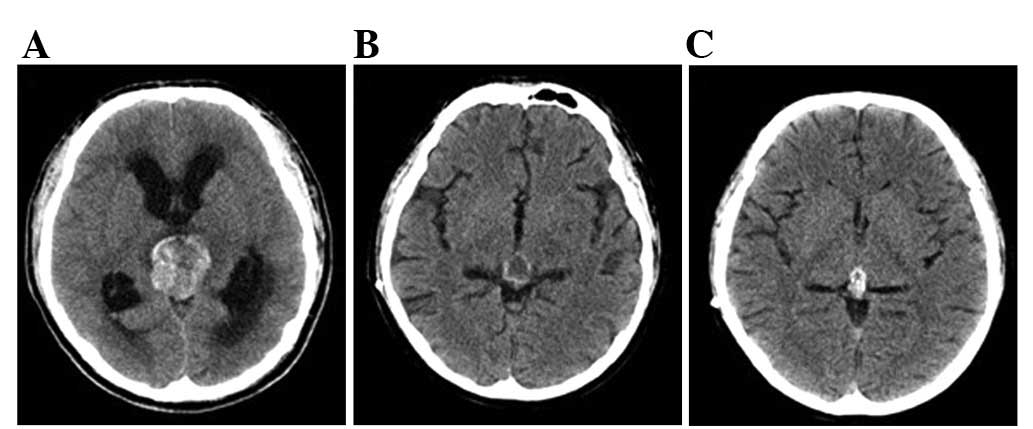
Computed tomography (CT) and magnetic resonance imaging (MRI) scans
revealed acute hydrocephalus and a mass (38x30 mm) with foci of
hemorrhage and calcification in the pineal region (Fig. 1A). Whole spine MRI and cerebrospinal
fluid (CSF) cytology results demonstrated normal extra-neural/CSF
metastasis. The pituitary function survey revealed normal levels of
growth hormone (GH), follicle-stimulating hormone (FSH),
luteinizing hormone (LH), vasopressin AVP) and prolactin (PRL). The
patient suddenly presented with a confused mental status,
bradycardia and decreased respiration, and underwent emergency
third ventriculostomy to relieve some of the symptoms, which were
caused by hydrocephalus blocking the flow of the spinal fluid in
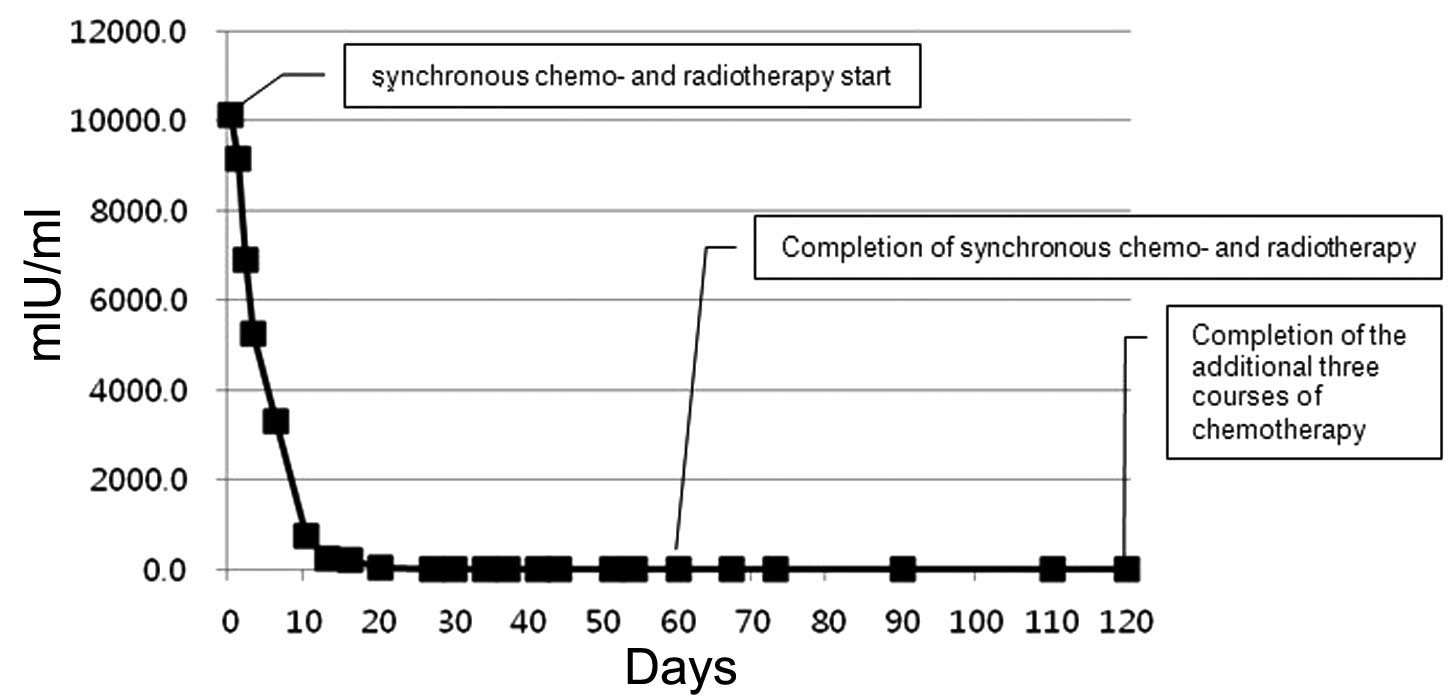
the brain. The baseline levels of serum β human chorionic
gonadotropin (β-HCG) and α-fetoprotein (AFP) were 10147 mIU/ml and
2.6 ng/ml, respectively. The CSF β-HCG and AFP were 634 mIU/ml and
0.6 ng/ml, respectively. Positron emission tomography-CT (PET-CT)
enhanced abdominopelvic CT and chest CT were conducted, and no
abnormal lesions were observed, with the exception of the pineal
region. The patient underwent synchronous ifosfamide, cisplatin and
etoposide chemotherapy (ICE; I, 900 mg/m2; C, 20
mg/m2; and E, 60 mg/m2) on days 1–5, and
external radiotherapy (whole brain, 30 Gy/15 Fxs; local boost, 30
Gy/15 Fxs) followed by ventriculoperitoneal CSF shunting. Following
completion of the first course of synchronous chemotherapy and
radiotherapy, the serum β-HCG and AFP were normalized at 0.2 mIU/ml
and 2.2 ng/ml, respectively (Fig.
2). Imaging studies (CT and MRI) demonstrated an ∼45% reduction
in the tumor mass (21x16 mm) and disappearance of the hydrocephalus
(Fig. 1B). Consequently, the
patient underwent an additional three courses of chemotherapy with
the same ICE regimen. The tumor mass was further reduced by 63%
(14x12 mm; Fig. 1C), and the
patient’s abnormal neurological symptoms recovered fully. It was
difficult to remove the remaining tumor using a surgical approach
due to the risk of postoperative hemorrhage and limited access. We
aimed to observe the remaining mass without surgery, and since then
the patient has undergone regular CT/MRI follow-up as well as serum
β-HCG and AFP level examinations every three months. The patient is
now alive, the mass size has not changed for 18 months since
treatment, and he is leading a normal life.
Discussion
PICCCs are extremely rare and represent only 0.05%
of all brain tumors in Japan (4). A
statistical analysis report published by the Committee of Brain
Tumors Registry of Japan indicated that the incidence of
choriocarcinoma was 3.2% (36 cases) out of 1127 primary
intracranial GCT cases (5).
Additionally, Matsutani et al analyzed 153 cases of
histologically verified intracranial GCTs and revealed that the
incidence of choriocarcinoma was 3.3% (3). Due to this extremely low incidence,
the majority of publications refer to case reports (6–11), and
few studies have compared the treatment and prognosis (1,3).
Matsutani et al classified intracranial GCT into three
therapeutic groups: those with good, intermediate and poor
prognoses. PICCCs were classified into the poor prognosis group,
and this group required more aggressive chemotherapy and
radiotherapy (3). A recent review
article presented an algorithm for diagnostic evaluation and
treatment of pineal or suprasellar tumors (12). The author suggested that PICCCs
require combinational therapy comprising chemotherapy, radiotherapy
and resection. However, there is currently no clear national
consensus for the optimal treatment of PICCCs.
Shinoda et al reviewed 66 PICCC/GCTs with
high β-HCG levels and revealed that their median survival time and
their one- and two-year survival rates were 22 months, 61.2% and
49.8%, respectively (1). Among
these 66 patients, 34 (52%) succumbed within one year of diagnosis
and 14 (21%) succumbed within one month of diagnosis. Early
mortality is commonly associated with tumor hemorrhage. This
suggests that the prognosis of these patients may be improved if
the initial treatment focuses on the prevention of tumor
hemorrhage.
To minimize early mortality arising from tumor
hemorrhage, we planned the following treatment regimen. First, we
did not conduct a tumor biopsy for pathological confirmation. β-HCG
is regarded to be more characteristic of β-HCG-secreting tumors.
Markedly elevated β-HCG levels are strongly suggestive of
choriocarcinomas, while mild elevations can be observed in other
GCTs of syncytiotrophoblastic giant cells (1). In a study by Matsutani et al,
all patients with pure choriocarcinomas or mixed GCTs with a
choriocarcinoma element had highly elevated serum β-HCG levels of
>2,000 IU/l, while GCT patients without a choriocarcinoma
element had serum β-HCG levels of <770 IU/l (3). The serum β-HCG level in our patient
was >1,0147 mIU/ml. The patient had a tumor arising from the
pineal region with hemorrhage, hydrocephalus and a history of
progressive consciousness deterioration. A biopsy was not conducted
due to the limited access and high hemorrhagic risk. We diagnosed
the tumor as PICCC based only on extremely elevated β-HCG levels,
and could prevent tumor hemorrhage by biopsy. Secondly, we selected
synchronous chemotherapy and radiotherapy as the first-line
treatment. Sakurada et al reported that tumor hemorrhage
occurred when radiotherapy was conducted as an initial treatment
(13). Shinoda et al stated
that initial biopsy and radiotherapy may lead to tumor hemorrhage
in PICCCs (1). Thus, we determined
that it was dangerous to start treatment with radiation alone.
Kageji et al reported a case of successful neoadjuvant
synchronous chemotherapy and radiotherapy for disseminated PICCC
(8). The patient underwent
induction chemotherapy in parallel with radiotherapy as the initial
treatment. Following radiotherapy and the second course of
chemotherapy, the patient underwent radical tumor surgery. There
was no evidence of hemorrhage during neoadjuvant treatment. Based
on this, we immediately started initial treatment comprising
synchronous chemotherapy and radiotherapy. The patient did not
undergo fatal events by hemorrhage during synchronous therapy, and
once the first course of synchronous chemotherapy and radiotherapy
was complete, the previously observed hemorrhage had disappeared.
Thirdly, we did not attempt to remove the remaining mass. The
patient had a tumor arising from the pineal region, and due to the
number of neurovascular structures in this area, it is a surgically
inaccessible area of the brain (14). Despite the fact that the tumor
hemorrhage had disappeared following the first course of treatment,
the hemorrhagic risk of PICCC remained. Chan et al reported
a case of successful treatment with chemotherapy and radiotherapy
without surgery (15). We planned
three consecutive courses of chemotherapy without surgery. The
tumor mass was reduced by 63% (14x12 mm), and the patient’s
abnormal neurological symptoms were fully recovered.
To date, the majority of the literature suggests
that intensive chemotherapy, radiation and tumor resection offer
the best chance of treating PICCCs. We agree with this opinion;
however, we suggest that a personal approach to prevent early tumor
hemorrhage is the most important factor.
Although PICCCs are rare, their propensity for fatal
hemorrhage and extraneural/CSF metastasis results in a poor
prognosis. Our patient exhibited severe consciousness disturbances
and a high level of serum β-HCG. Since the initial imaging study
demonstrated a tumor mass with hemorrhage in the pineal region, we
immediately began synchronous chemotherapy and radiotherapy.
Subsequently, our patient underwent three courses of chemotherapy,
each comprising the same ICE regimen. The residual tumor mass was
not resected due to limited access and hemorrhagic risk. Nearly two
years following the initial diagnosis, the patient is alive without
tumor progression and with normal neurological functions.
In conclusion, we reported a rare case of PICCC. We
diagnosed our patient with the aid of serum β-HCG level without
biopsy, and immediately started induction therapy comprising
synchronous chemotherapy and radiotherapy. Without surgery, we
delivered ICE chemotherapy as consolidation treatment. These
treatments led to tumor regression and marked improvements in the
patient’s signs and symptoms. Nearly two years post-diagnosis,
follow-up imaging has demonstrated no tumor progression. This is
the first report of successful synchronous chemotherapy and
radiotherapy, followed by three courses of consecutive
chemotherapy, to treat a patient diagnosed with PICCC by focusing
the initial treatment on the prevention of tumor hemorrhage.
References
|
1.
|
J ShinodaN SakaiH YanoT HattoriA OhkumaH
SakaguchiPrognostic factors and therapeutic problems of primary
intracranial choriocarcinoma/germ-cell tumors with high levels of
HCGJ
Neurooncol66225240200410.1023/B:NEON.0000013499.74404.8115015791
|
|
2.
|
MT JenningsR GelmanF HochbergIntracranial
germ-cell tumors: natural history and pathogenesisJ
Neurosurg63155167198510.3171/jns.1985.63.2.01552991485
|
|
3.
|
M MatsutaniK SanoK TakakuraPrimary
intracranial germ cell tumors: a clinical analysis of 153
histologically verified casesJ
Neurosurg86446455199710.3171/jns.1997.86.3.04469046301
|
|
4.
|
M MatsutaniClinical management of primary
central nervous system germ cell tumorsSemin
Oncol31676683200410.1053/j.seminoncol.2004.07.01015497121
|
|
5.
|
The Committee of the Brain Tumor Registry
of Japan: Report of Brain Tumor Registry of Japan (1969–1993). 10th
editionNeurol Med Chir40Suppl1106200014705327
|
|
6.
|
Y KawakamiO YamadaK TabuchiT OhmotoA
NishimotoPrimary intracranial choriocarcinomaJ
Neurosurg53369374198010.3171/jns.1980.53.3.0369
|
|
7.
|
T FujiiT ItakuraS HayashiN KomaiH
NakamineK SaitoPrimary pineal choriocarcinoma with hemorrhage
monitored by computerized tomography. Case reportJ
Neurosurg55484487198110.3171/jns.1981.55.3.04847196441
|
|
8.
|
T KagejiS NagahiroK MatsuzakiSuccessful
neoadjuvant synchronous chemo- and radiotherapy for disseminated
primary intracranial choriocarcinoma: case reportJ
Neurooncol83199204200710.1007/s11060-006-9311-117205387
|
|
9.
|
H NittaJ YamashitaM NomuraN
IgarashiCervical spinal cord infarction after surgery for a pineal
region choriocarcinoma in the sitting position: case
reportNeurosurgery4010821085discussion10851086199710.1097/00006123-199705000-000399149270
|
|
10.
|
K TaomotoN TamakiY OboraK NakaiH
SatoIntracranial human chorionic gonadotropin producing tumors
(author’s transl)Neurol Med Chir (Tokyo)164114181976(In
Japanese).
|
|
11.
|
M MarxJD BeckGG GrabenbauerR FahlbuschHG
DörrGonadotrophin-independent puberty in a boy with a
beta-HCG-secreting brain tumourHorm Res544448200011182635
|
|
12.
|
AP KyritsisManagement of primary
intracranial germ cell tumorsJ
Neurooncol96143149201010.1007/s11060-009-9951-z19588227
|
|
13.
|
K SakuradaT KayamaK KawakamiM SainoS SatoA
successfully operated case of choriocarcinoma with recurrent
intratumoral hemorrhageNo Shinkei Geka2867722000(In Japanese).
|
|
14.
|
I YamamotoPineal region tumor: surgical
anatomy and approachJ
Neurooncol54263275200110.1023/A:101279021381811767292
|
|
15.
|
HS ChanRP HumphreysEB HendrickSH ChuangCR
FitzLE BeckerPrimary intracranial choriocarcinoma: a report of two
cases and a review of the
literatureNeurosurgery15540545198410.1227/00006123-198410000-000126541765
|