Introduction
Although the liver is a common target for
metastasis, acute or fulminant liver failure due to metastasis is a
rare occurrence (1–7). Diffuse parenchymal metastasis is a
rare pattern of liver metastasis that is correlated with hepatic
failure and an extremely poor prognosis (1–8).
Unlike the usual patterns of liver metastasis, radiological studies
are typically not able to detect this type of pattern (1,3–5,7).
Therefore, metastasis is frequently diagnosed by autopsy (3). In the present study, the authors
describe a case of acute liver failure correlated with diffuse
liver infiltration by metastatic carcinoma in a 49-year-old female
with a history of breast cancer.
Case report
Clinical summary
A 49-year-old Thai female was admitted to hospital
due to a high grade fever, jaundice and abdominal pain in the right
upper quadrant. Four weeks prior to admission, the patient suffered
from malaise, anorexia and weight loss. An initial investigation
revealed that the patient had anemia (Hct, 23%) and abnormal liver
function test results (total bilirubin, 75.24 μmol/l; direct
bilirubin, 34.2 μmol/l; AST, 250 U/l; ALT, 63 U/l; ALP, 198
U/l). The patient received treatment for chronic cholecystitis and
hepatitis; however, the symptoms progressed and the patient
developed thrombocytopenia and coagulopathy. The liver function
test results also worsened (peak values: total bilirubin, 890.91
μmol/l; direct bilirubin, 598.5 μmol/l; AST, 1152
U/l; ALT, 114 U/l; ALP, 845 U/l; GGT, 727 U/l), while both
ultrasonography and computed tomography (CT) scans of the abdomen
were not able to detect any specific hepatic lesions. No evidence
of viral hepatitis or any identifiable source of infection was
observed. The patient’s condition deteriorated further; hepatic
encephalopathy developed and the patient died within the third week
following the onset of acute hepatic failure. The patient had a
history of breast carcinoma stage I and had been treated by
modified radical mastectomy (MRM), and had remained disease-free
for 10 years following treatment.
Pathological findings
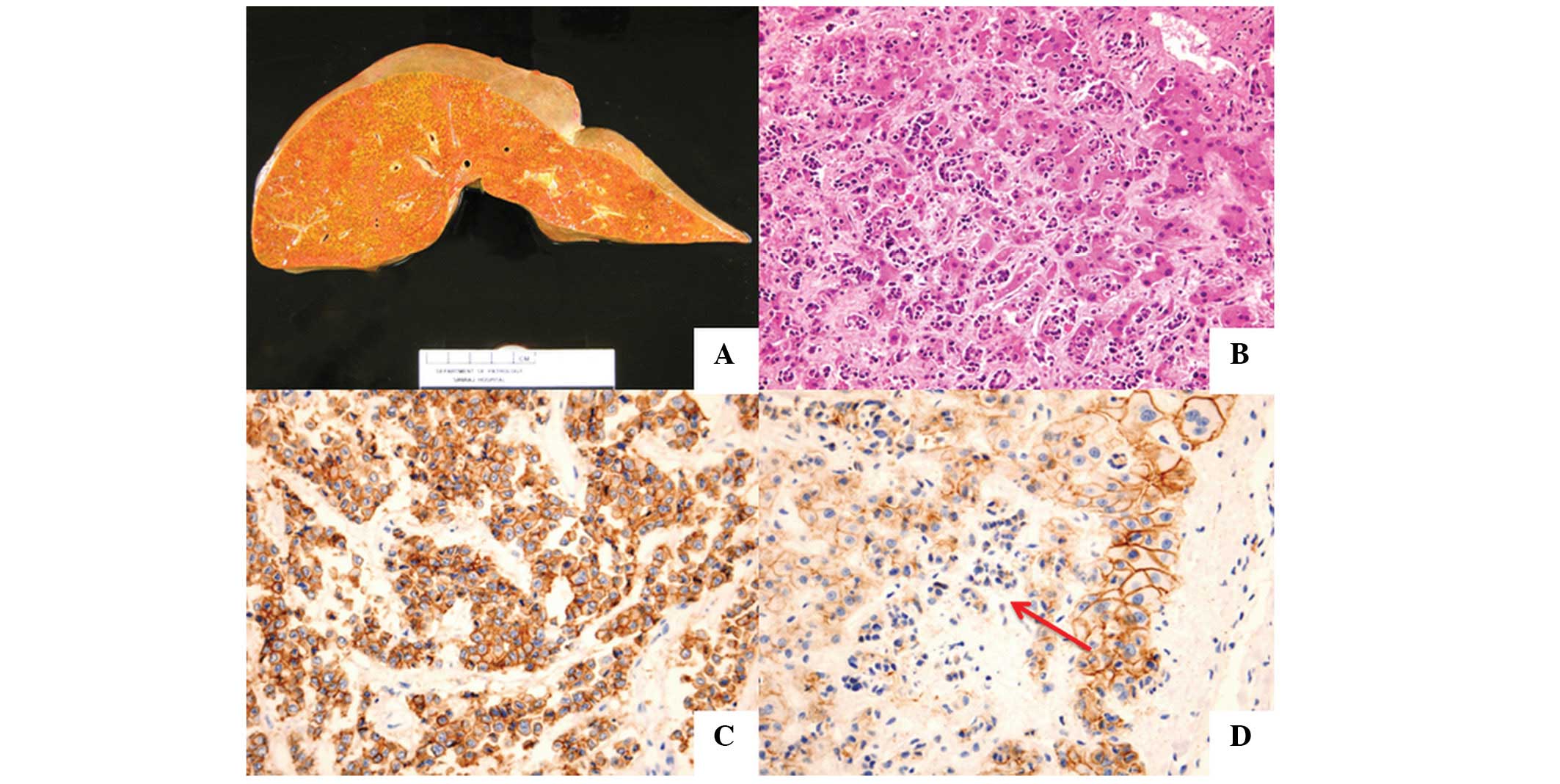
The gross appearance of the liver revealed that the
patient had hepatomegaly (2,150 gm). The liver capsule was smooth,
the cut surfaces of which showed non-homogeneous dark brown and
yellow tissue and no mass-forming lesions (Fig. 1A). An ill-defined yellow-brown
nodule (4 cm in diameter) was observed at the pancreas, and
multiple small yellow-brown nodules were found at the pleural
surface and parenchyma of both lungs. Other abnormal gross findings
included splenomegaly and pulmonary congestion. A previous surgical
scar from the MRM was detected without any abnormality in both
breasts or axillary regions.
Microscopic examination revealed diffuse
infiltration of the liver parenchyma by pleomorphic cells with some
glandular formation (Fig. 1B).
Extensive necrosis of hepatocytes was noted. The tumor cells were
positive for CK7, ER and PR, while negative for CK 20 and TTF-1.
These results support the diagnosis of primary breast
carcinoma.
Metastatic tumor infiltration was also detected in
the spleen and both adrenal glands. Sections from nodules in the
pancreas and the lungs demonstrated metastatic carcinoma. In
addition, microscopic foci of metastasis were observed in the
uterine cervix, appendix, bone marrow, thyroid and intrathoracic
lymph nodes. No evidence of carcinoma was identified in the breast
tissue samples. Additional abnormal histological findings included
pulmonary congestion with edema and focal hemorrhage, myocardial
hypertrophy, acute tubular necrosis of both kidneys and
hypoxic-ischemic changes in the brain tissue.
Immunohistochemical staining for E-cadherin was also
performed. Notably, tumor cells in the lung nodule strongly
expressed E-cadherin (Fig. 1C),
while tumor cells in the liver did not (Fig. 1D).
Discussion
With the exception of the lymph nodes, the liver is
considered to be the most frequent site of metastasis (9–11). In
breast cancer, the liver is also one of the major metastatic
targets along with the lungs and bone (1,9,12). The
most common pattern of liver metastasis is the formation of
discrete multiple nodules followed by a single nodule, while
diffuse tumor invasion into the liver parenchyma or diffuse
parenchymal metastasis is less common (3,4,12).
Hematological malignancies are recognized to be the most common
cause of diffuse parenchymal metastasis (1,3,4). This
metastatic pattern has also been identified in many primary
neoplasms, including breast, lung, stomach, colon, pancreatic,
nasopharynx, urothelial, uterine and malignant melanoma (3,4,7,8).
Acute liver failure rarely occurs in typical liver
metastasis, although abnormal liver enzymes may be detected
(3,4,7),
whilst this condition is more common in diffuse parenchymal
metastasis (1,7). This complication is speculated to be
caused by extensive hepatocellular necrosis resulting from pressure
atrophy and interference of the vascular supply (4,6–8,13).
Radiological studies including ultrasonography, CT and MRI scans
are usually not able to identify diffuse parenchymal metastasis
(1,3–5,7), thus
increasing the difficulty in the diagnosis. Radiological findings
resembling cirrhosis have also been reported (1,7,14). To
confirm the diagnosis, histological examination is necessary and a
liver biopsy may be useful (3,5,7).
The prognosis of acute liver failure secondary to
malignant infiltration is extremely poor; the majority of patients
do not survive shortly after the onset of liver failure (1–4,7,8).
According to a review by Allison et al, concerning 21
reported cases of acute liver failure due to metastatic breast
carcinoma, 18 cases died within three days to two months (7). Non-specific prodromal symptoms, such
as malaise, weight loss, right upper quadrant abdominal pain and
fever, are always observed to be present at least two to four weeks
prior to the onset of liver failure (3,4).
The underlying mechanism of diffuse parenchymal
metastasis remains unknown. Allison et al proposed a loss of
cell surface adhesional molecule expression; the three cases in
their study described as diffuse intrasinusoidal hepatic metastasis
did not express both E-cadherin and CD44, which are glycoproteins
involved in cell-cell and cell-extracellular matrix adhesion
(7). In the present case, a
difference in E-cadherin expression in the two different areas of
metastasis was observed; the tumor cells in the metastatic nodule
in the lung stained positive for E-cadherin, while the infiltrating
tumor cells in the liver stained negative. These findings support
the hypothesis that a loss of cell surface adhesional molecule
expression is involved in facilitating diffuse parenchymal
metastais.
In conclusion, although malignant infiltration of
the liver is rare, it ought to be considered as a differential
diagnosis in patients with acute hepatic failure. Liver biopsy may
be the most effective technique to confirm the diagnosis during the
patient’s life.
Acknowledgements
The authors would like to thank Dr
Chayawee Muangchan from the Department of Medicine, Siriraj
Hospital, Mahidol University, for providing the clinical
information.
References
|
1
|
Nazario HE, Lepe R and Trotter JF:
Metastatic breast cancer presenting as acute liver failure.
Gastroenterol Hepatol. 7:65–66. 2011.PubMed/NCBI
|
|
2
|
Begin LR, Boucher D and Lamoureux E:
Diffuse hepatic intravascular carcinomatous embolization resulting
in fatal liver failure: a clinicopathologic study of 4 cases.
Pathol Res Pract. 197:433–440. 2001. View Article : Google Scholar
|
|
3
|
Rowbotham D, Wendon J and Williams R:
Acute liver failure secondary to hepatic infiltration: a single
centre experience of 18 cases. Gut. 42:576–580. 1998. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Athanasakis E, Mouloudi E, Prinianakis G,
Kostaki M, Tzardi M and Georgopoulos D: Metastatic liver disease
and fulminant hepatic failure: presentation of a case and review of
the literature. Eur J Gastroenterol Hepatol. 15:1235–1240. 2003.
View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Alexopoulou A, Koskinas J, Deutsch M,
Delladetsima J, Kountouras D and Dourakis SP: Acute liver failure
as the initial manifestation of hepatic infiltration by a solid
tumor: report of 5 cases and review of the literature. Tumori.
92:354–357. 2006.
|
|
6
|
Schneider R and Cohen A: Fulminant hepatic
failure complicating metastatic breast carcinoma. South Med J.
77:84–86. 1984. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Allison KH, Fligner CL and Parks WT:
Radiographically occult, diffuse intrasinusoidal hepatic metastases
from primary breast carcinomas: a clinicopathologic study of 3
autopsy cases. Arch Pathol Lab Med. 128:1418–1423. 2004.
|
|
8
|
Barreales M, Casis B, Sáenz López S and
Solis Herruzo JA: Fulminant hepatic failure caused by metastatic
liver disease. Rev Esp Enferm Dig. 99:245–247. 2007.(In
Spanish).
|
|
9
|
Disibio G and French SW: Metastatic
patterns of cancers: results from a large autopsy study. Arch
Pathol Lab Med. 132:931–939. 2008.PubMed/NCBI
|
|
10
|
Centeno BA: Pathology of liver metastases.
Cancer Control. 13:13–26. 2006.PubMed/NCBI
|
|
11
|
Mitchell ML, Filippone MD and Wozniak TF:
Metastatic carcinomatous cirrhosis and hepatic hemosiderosis in a
patient heterozygous for the H63D genotype. Arch Pathol Lab Med.
125:1084–1087. 2001.
|
|
12
|
Wyld L, Gutteridge E, Pinder SE, et al:
Prognostic factors for patients with hepatic metastases from breast
cancer. Br J Cancer. 89:284–290. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Burnett RA: Cor pulmonale due to tumour
embolism derived from intrasinusoidal metastatic liver carcinoma. J
Clin Pathol. 28:457–464. 1975. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Nascimento AB, Mitchell DG, Rubin R and
Weaver E: Diffuse desmoplastic breast carcinoma metastases to the
liver simulating cirrhosis at MR imaging: report of two cases.
Radiology. 221:117–121. 2001. View Article : Google Scholar
|