Introduction
Gastric gastrointestinal stromal tumor (GIST) may be
cured by sleeve resection without lymph node dissection.
Laparoscopic surgery for GIST has been established as a less
invasive option, provided that it is performed by experienced
laparoscopic surgeons (1–4). However, laparoscopic resection for
large gastric GISTs remains under debate due to the high risk of
intraoperative tumor rupture. Liver metastases are common in
advanced or unresectable GISTs. Patients with multiple liver
metastases carry the risk of severe postoperative functional
deficit if massive hepatectomy is performed. In the present study
we present a case of large gastric GIST and synchronous liver
metastases in a patient receiving one-stage laparoscopic resection
following preoperative imatinib treatment. The study was approved
by the Ethics Committee of Xuanwu Hospital, Capital Medical
University, Beijing, China. Written informed consent was obtained
from the patient.
Case report
A 63-year-old female was admitted to the Department
of General Surgery, Xuanwu Hospital, Beijing, China, complaining of
melena for 5 days. Following resuscitation, gastric endoscopy was
performed and a submucosal lesion in the body of the stomach was
reported. A biopsy confirmed the diagnosis of gastric GIST with
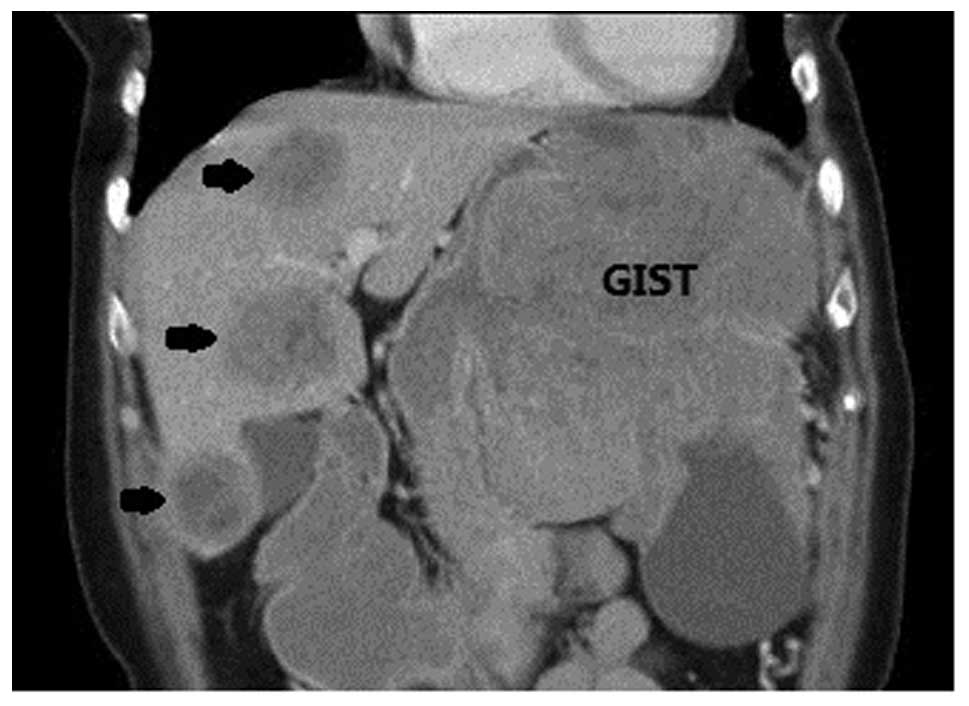
c-kit exon 11 mutation. Computed tomography (CT) of the abdomen
showed an intramural GIST ∼15×10 cm in size with multiple liver
metastases (Fig. 1). The CT value
was 22 and 46 HU prior to and following contrast introduction,
respectively. Tumor markers were within the normal range.
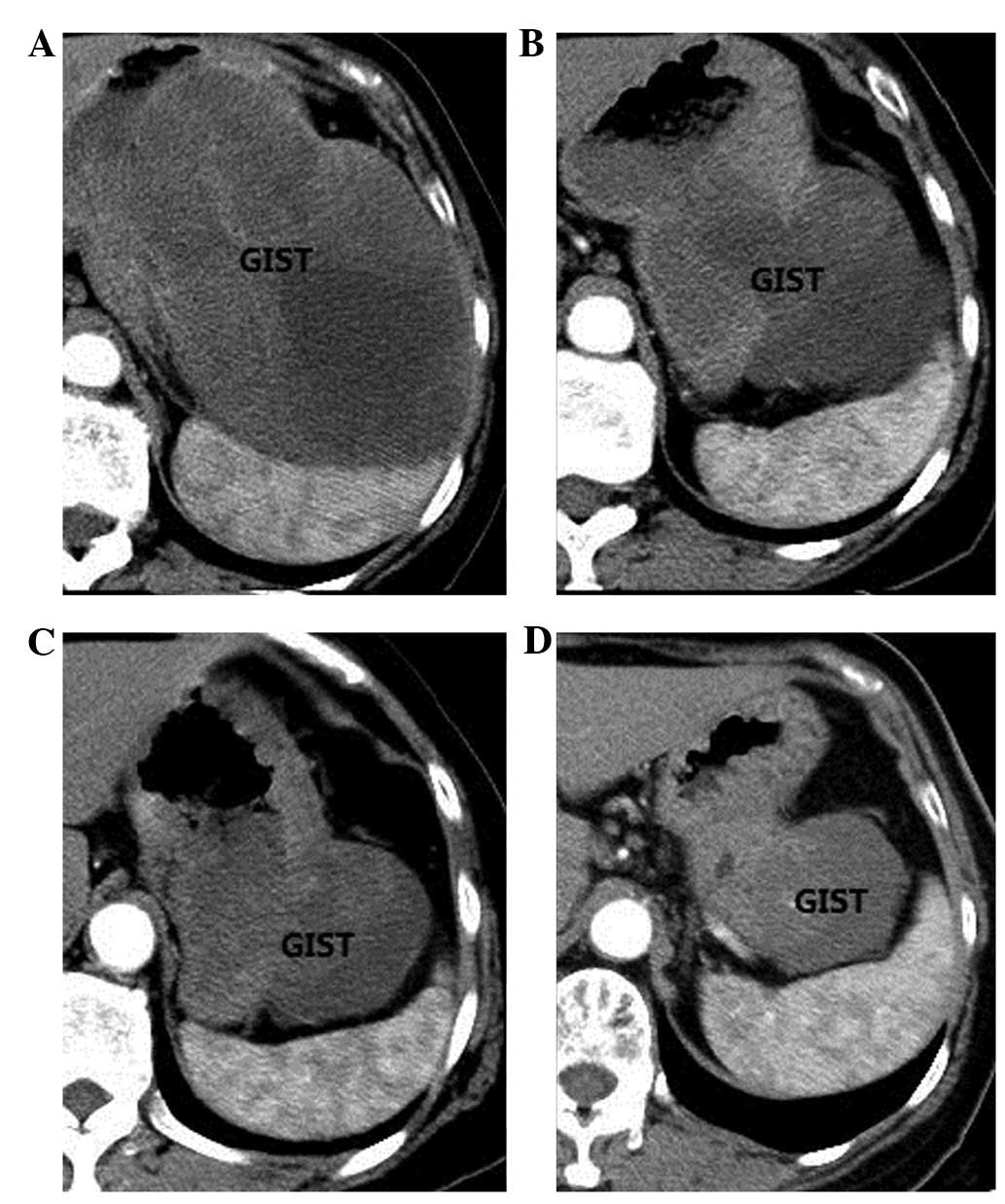
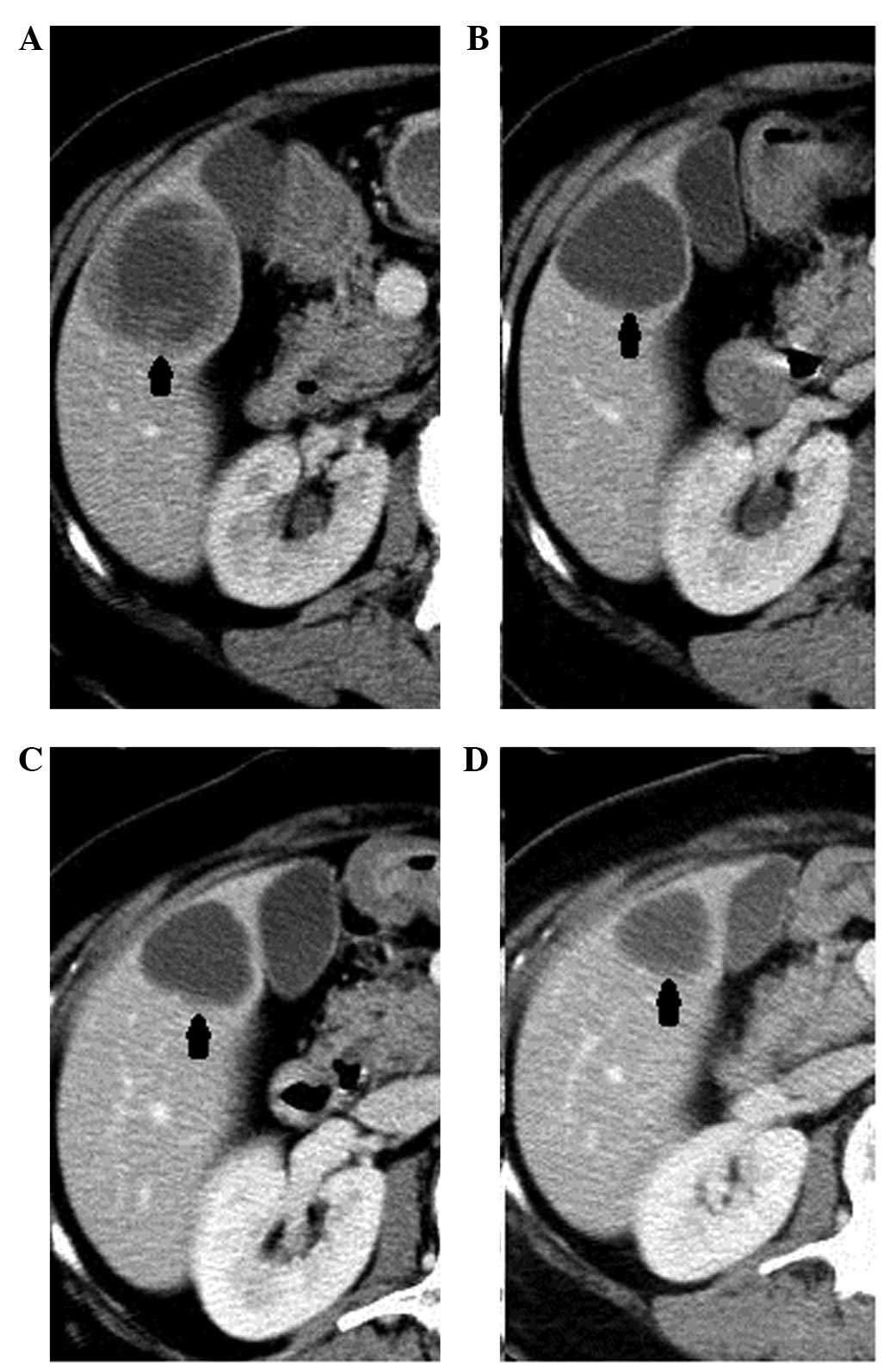
Preoperative imatinib (400 mg/day) therapy was
administered to this patient. The clinical and morphologic response
was monitored by physical examination and CT scan every two months
(Figs. 2 and 3). The size of the tumor decreased
markedly and the CT value declined. No symptoms of upper
gastrointestinal bleeding recurred during the treatment.
After 6 months’ preoperative treatment, a partial
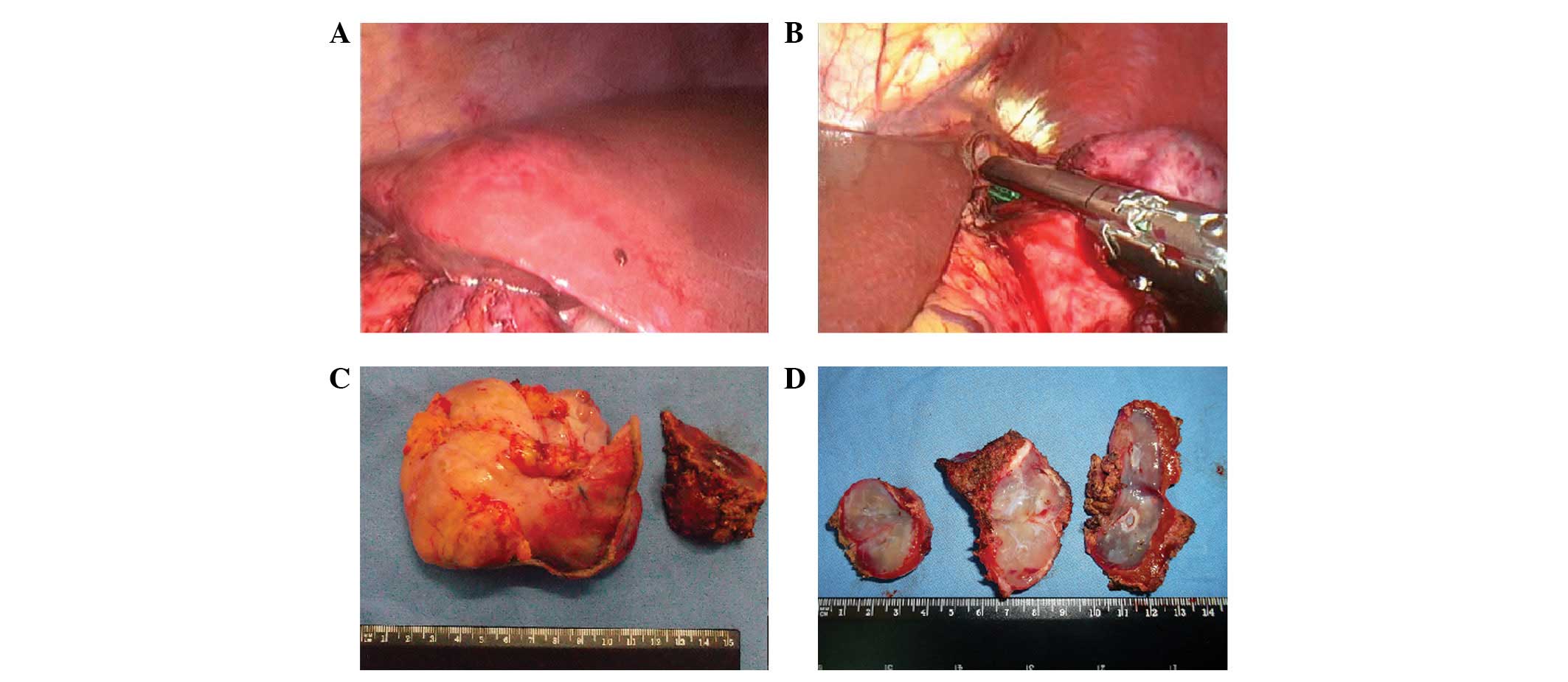
response was achieved according to Choi criteria (5). Laparoscopic surgery was subsequently
performed to remove the gastric GIST and liver metastases
synchronously (Fig. 4).
Laparoscopic sleeve resection was performed to resect the gastric
tumor using two Endo GIA staplers (Ethicon, Johnson and Johnson,
Cincinnati, OH, USA). In order to not disrupt the serosal surface
and cause tumor spillage, the mass was grasped and gently elevated
with an atraumatic bowel grasper during the operation. Liver
metastases enucleation was then performed using the LigaSure system
(Valleylab, Boulder, CO, USA). All the specimens were retrieved in
an endobag without spillage through a muscle-splitting incision in
the left flank. The surgery time was 185 min and the estimated
blood loss was ∼150 ml. The recovery of the patient was
uneventful.
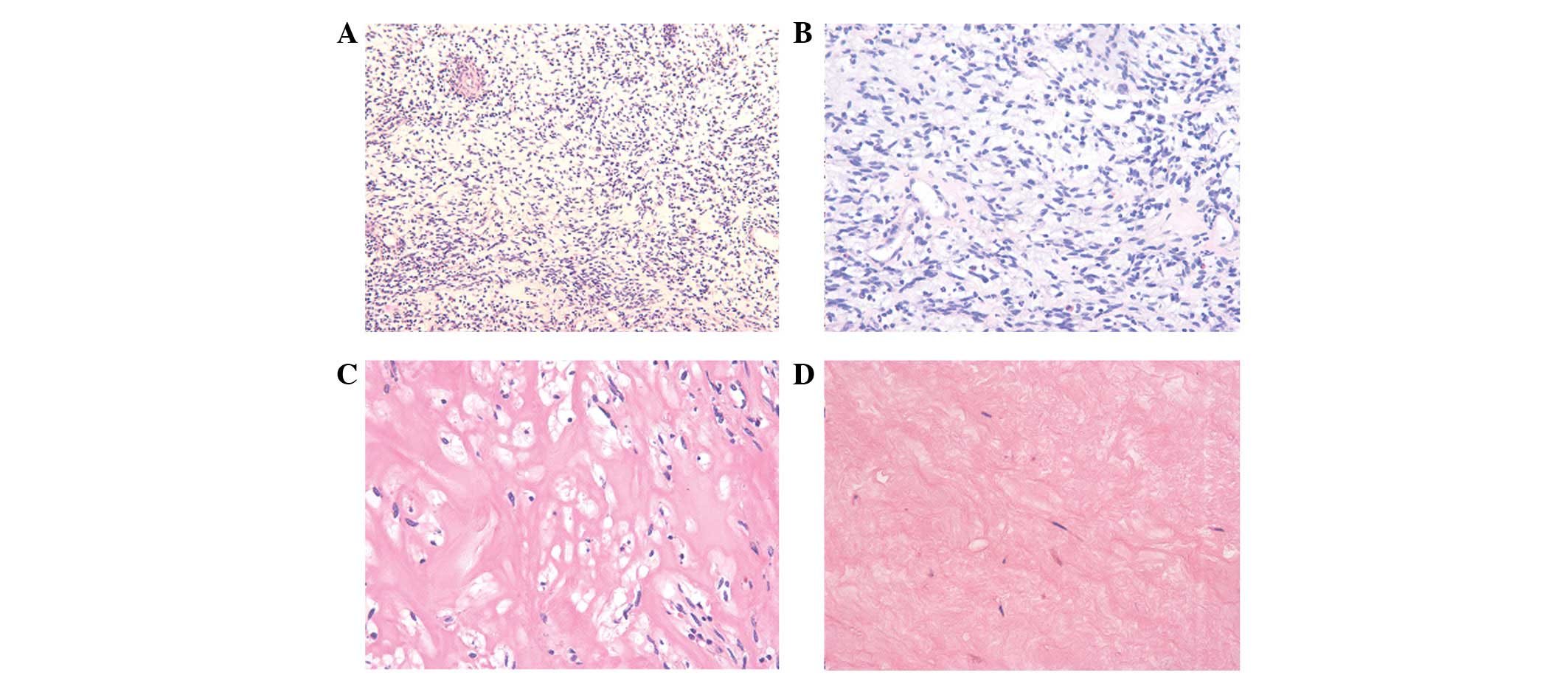
Pathological evaluation of the stomach specimen
revealed that the structure of the mucosa was normal, and that the
tumor mass was present in the muscular layer. Microscopically,
although tumor cells with sharp spindles were detected in certain
areas, the number had declined significantly compared with that in
the biopsy specimens. Many large areas of hyaline degeneration were
found with mitotic figures <5 per 50 high-power fields (Fig. 5). The tumor margins were negative in
both the stomach and liver specimens. The immunohistochemistry
study showed that cells were positive for CD117 and CD34, and
negative for SMA, desmin and s-100.
Four weeks following the surgery, imatimib treatment
was resumed at 400 mg/day. Eleven months following the surgical
resection, the imatinib treatment was ongoing, the patient was
asymptomatic and there was no radiological or clinical evidence of
disease recurrence.
Discussion
Gastric GIST is a relatively rare entity of
nonepithelial, mesenchymal neoplasm with increasing rates of
diagnosis due to the widespread use of upper endoscopy and
endoscopic ultrasound. Gastric GIST may grow quite large without
any symptoms. In the series of De Vogelaere et al, GISTs
with a tumor size larger than 2 cm accounted for >80% of cases
(6). Partial gastrectomy with a
gross free surgical margin is accepted worldwide as a treatment
method since GIST rarely involves the lymph nodes. The role of
laparoscopic, even single-incision laparoscopic surgery, has been
established in the past decade in the treatment of gastric GIST
(1–4,7,8).
However, the feasibility of laparoscopic resection for large
gastric GISTs remains largely unknown. The GIST Consensus
Conference 2004 (9) recommended
limiting laparoscopic resection to tumors smaller than 2 cm due to
the increased risk of tumor rupture and spillage. The consensus of
Chinese experts is the recommendation of laparoscopic surgery for
GIST patients with a tumor size less than 5 cm. Liver metastases
are common in advanced or unresectable GIST; however, these
metastases may be curable when the primary disease has been
eradicated and negative surgical resection margins are attained.
Although evidence is lacking, literature reports of colorectal
liver metastases have demonstrated that one-stage resection for
primary tumor and liver metastases is safe and effective (10).
In our case, surgical resection was not selected as
the initial therapy for the following reasons. First, the
anatomical location and the association between the giant primary
tumor and the contiguous organs was not clear, with some doubt
regarding the invasion to the diaphragm and splenic hilum. Extended
surgery would be required without any appreciable gain in clinical
benefit. Second, as multiple liver metastases were present in the
different liver segments, surgery may have led to a marked loss of
organ function. Third, genetic testing of biopsy specimens revealed
the c-kit exon 11 mutation which indicated a notable response to
imatinib therapy (11,12). Guidelines from the National
Comprehensive Cancer Network (NCCN) also recommend preoperative
imatinib treatment as the primary treatment for metastatic GIST.
After 6 months’ therapy, a curative surgery synchronously resecting
primary tumor and liver metastases was enabled.
Owing to the cooperation of oncologists and
surgeons, our patient received curative treatment with visceral and
functional preservation, maintaining a high quality of life.
One-stage laparoscopic resection may be an option
for large gastric GISTs with synchronous liver metastases. For
advanced or unresectable GIST, preoperative imatinib treatment may
be a bridge to curable disease. Minimally invasive approaches may
be as safe and effective as open surgery. A greater number of cases
and long-term follow-up are necessary to confirm this.
References
|
1
|
Pucci MJ, Berger AC, Lim PW, Chojnacki KA,
Rosato EL and Palazzo F: Laparoscopic approaches to gastric
gastrointestinal stromal tumors: an institutional review of 57
cases. Surg Endosc. 26:3509–3514. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Ma JJ, Hu WG, Zang L, Lu AG, Wang ML, Li
JW, Feng B, Zhong J and Zheng MH: Laparoscopic gastric resection
approaches for gastrointestinal stromal tumors of stomach. Surg
Laparosc Endosc Percutan Tech. 21:101–105. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Karakousis GC, Singer S, Zheng J, Gonen M,
Coit D, DeMatteo RP and Strong VE: Laparoscopic versus open gastric
resections for primary gastrointestinal stromal tumors (GISTs): a
size-matched comparison. Ann Surg Oncol. 18:1599–1605. 2011.
View Article : Google Scholar
|
|
4
|
Thakkar DV, Wani SV, Shetty V and Patankar
RV: Laparoscopic sleeve gastrectomy for a large gastrointestinal
stromal tumor. Surg Laparosc Endosc Percutan Tech. 22:e61–e62.
2012. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Choi H, Charnsangavej C, Faria SC,
Macapinlac HA, Burgess MA, Patel SR, Chen LL, Podoloff DA and
Benjamin RS: Correlation of computed tomography and positron
emission tomography in patients with metastatic gastrointestinal
stromal tumor treated at a single institution with imatinib
mesylate: proposal of new computed tomography response criteria. J
Clin Oncol. 25:1753–1759. 2007. View Article : Google Scholar
|
|
6
|
De Vogelaere K, Van Loo I, Peters O,
Hoorens A, Haentjens P and Delvaux G: Laparoscopic resection of
gastric gastrointestinal stromal tumors (GIST) is safe and
effective, irrespective of tumor size. Surg Endosc. 26:2339–2345.
2012.PubMed/NCBI
|
|
7
|
Takahashi T, Takeuchi H, Kawakubo H,
Saikawa Y, Wada N and Kitagawa Y: Single-incision laparoscopic
surgery for partial gastrectomy in patients with a gastric
submucosal tumor. Am Surg. 78:447–450. 2012.PubMed/NCBI
|
|
8
|
Hirano Y, Watanabe T, Uchida T, Yoshida S,
Kato H and Hosokawa O: Laparoendoscopic single site partial
resection of the stomach for gastrointestinal stromal tumor. Surg
Laparosc Endosc Percutan Tech. 20:262–264. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Blay JY, Bonvalot S, Casali P, Choi H,
Debiec-Richter M, Dei Tos AP, Emile JF, Gronchi A, Hogendoorn PC,
Joensuu H, Le Cesne A, McClure J, Maurel J, Nupponen N, Ray-Coquard
I, Reichardt P, Sciot R, Stroobants S, van Glabbeke M, van Oosterom
A and Demetri GD; GIST consensus meeting panelists: Consensus
meeting for the management of gastrointestinal stromal tumors.
Report of the GIST Consensus Conference of 20–21 March 2004, under
the auspices of ESMO. Ann Oncol. 16:566–578. 2005.PubMed/NCBI
|
|
10
|
Spampinato MG, Mandalá L, Quarta G, Del
Medico P and Baldazzi G: One-stage, totally laparoscopic major
hepatectomy and colectomy for colorectal neoplasm with synchronous
liver metastasis: Safety, feasibility and short-term outcome.
Surgery. July 31–2012.(Epub ahead of print).
|
|
11
|
Heinrich MC, Corless CL, Demetri GD,
Blanke CD, von Mehren M, Joensuu H, McGreevey LS, Chen CJ, Van den
Abbeele AD, Druker BJ, Kiese B, Eisenberg B, Roberts PJ, Singer S,
Fletcher CD, Silberman S, Dimitrijevic S and Fletcher JA: Kinase
mutations and imatinib response in patients with metastatic
gastrointestinal stromal tumor. J Clin Oncol. 21:4342–4349. 2003.
View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Heinrich MC, Owzar K, Corless CL, Hollis
D, Borden EC, Fletcher CD, Ryan CW, von Mehren M, Blanke CD, Rankin
C, Benjamin RS, Bramwell VH, Demetri GD, Bertagnolli MM and
Fletcher JA: Correlation of kinase genotype and clinical outcome in
the North American Intergroup Phase III Trial of imatinib mesylate
for treatment of advanced gastrointestinal stromal tumor: CALGB
150105 study by Cancer and Leukemia Group B and Southwest Oncology
Group. J Clin Oncol. 26:5360–5367. 2008.
|