Introduction
Current management of osteosarcoma comprises pre-
and postoperative chemotherapy and complete surgical removal of all
tumor sites (1–3). With this strategy, 5-year overall
survival rates of 70% have been reported for patients aged <40
years with non-metastatic, extremity-localized osteosarcoma at
diagnosis (4–6). However, anticancer chemotherapies are
responsible for numerous adverse events. Among these, hematological
toxicity is one of the main reasons for treatment discontinuation.
These toxicities decrease production of red blood cells (causing
anemia), white blood cells (neutropenia or granulocytopenia) and
platelets (thrombocytopenia) which may be life-threatening to the
patient. Such complications often result in dose reductions or
treatment delays, which may compromise clinical outcome, or even
mortality (7–12). Preventing discontinuation of
treatment would be valuable for treating patients more effectively.
Much research has shown that the hematological toxicity of
chemotherapy is based on the regimen and drug dose (13), but 40% of the patients who received
high-dose chemotherapy did not experience severe bone suppression
as grade III/IV leucopenia (14).
It may be considered that the regimen and dosage are not the only
risk factors for severe bone marrow suppression. To identify other
risk factors for hematological toxicity of chemotherapy for bone
and soft tissue sarcoma, 113 patients admitted to the Second
Xiangya Hospital of Central South University, China, and treated
with consistent neoadjuvant chemotherapy were studied
retrospectively. The aim of the study was to decrease the
occurrence of hematological toxicity following chemo-therapy and
increase the survival rate. The study was approved by the Ethics
Committee of the Department of Orthopaedics, The Second Xiangya
Hospital, Central South University, Changsha, Hunan, China.
Materials and methods
Patients
The present study included 113 children and adults
who had been treated with neoadjuvant chemotherapy following the
diagnosis of bone and soft tissue sarcoma between June 2007 and
April 2012. .Written informed patient consent was obtained from the
patients. The mean follow-up period was 29.6 months. The patient
characteristics are shown in Table
I. In the current study, severe bone marrow suppression was
mainly indicated by grade III/IV neutropenia or thrombocytopenia,
and the number of patients with grade III/IV anemia was relatively
rare. Notably, all patients who experienced grade III/IV
neutropenia also experienced grade III/IV thrombocytopenia, but
patients with grade III/IV thrombocytopenia did not often
experience grade III/IV neutropenia. The 113 patients were
therefore divided into two groups (A and B) based on clinical
evidence of grade III/IV neutropenia according to World Health
Organization (WHO) criteria for hematological toxicity.
 | Table IPatient characteristics. |
Table I
Patient characteristics.
| Characteristics | No. |
|---|
| Patients | 113 |
| Gender | |
| Male | 40 |
| Female | 73 |
| Median age
(range) | 16 (7–39) |
| Site | |
| Femur | 31 |
| Tibia | 25 |
| Humerus | 14 |
| Pelvis | 15 |
| Knee | 12 |
| Elbow | 4 |
| Shoulder | 9 |
| Other | 3 |
| Histology | |
| Osteosarcoma | 63 |
| Malignant fibrous
histiocytoma | 17 |
| Liposarcoma | 12 |
| Synovial
sarcoma | 10 |
|
Rhabdomyosarcoma | 5 |
| Leiomyosarcoma | 6 |
Chemotherapy
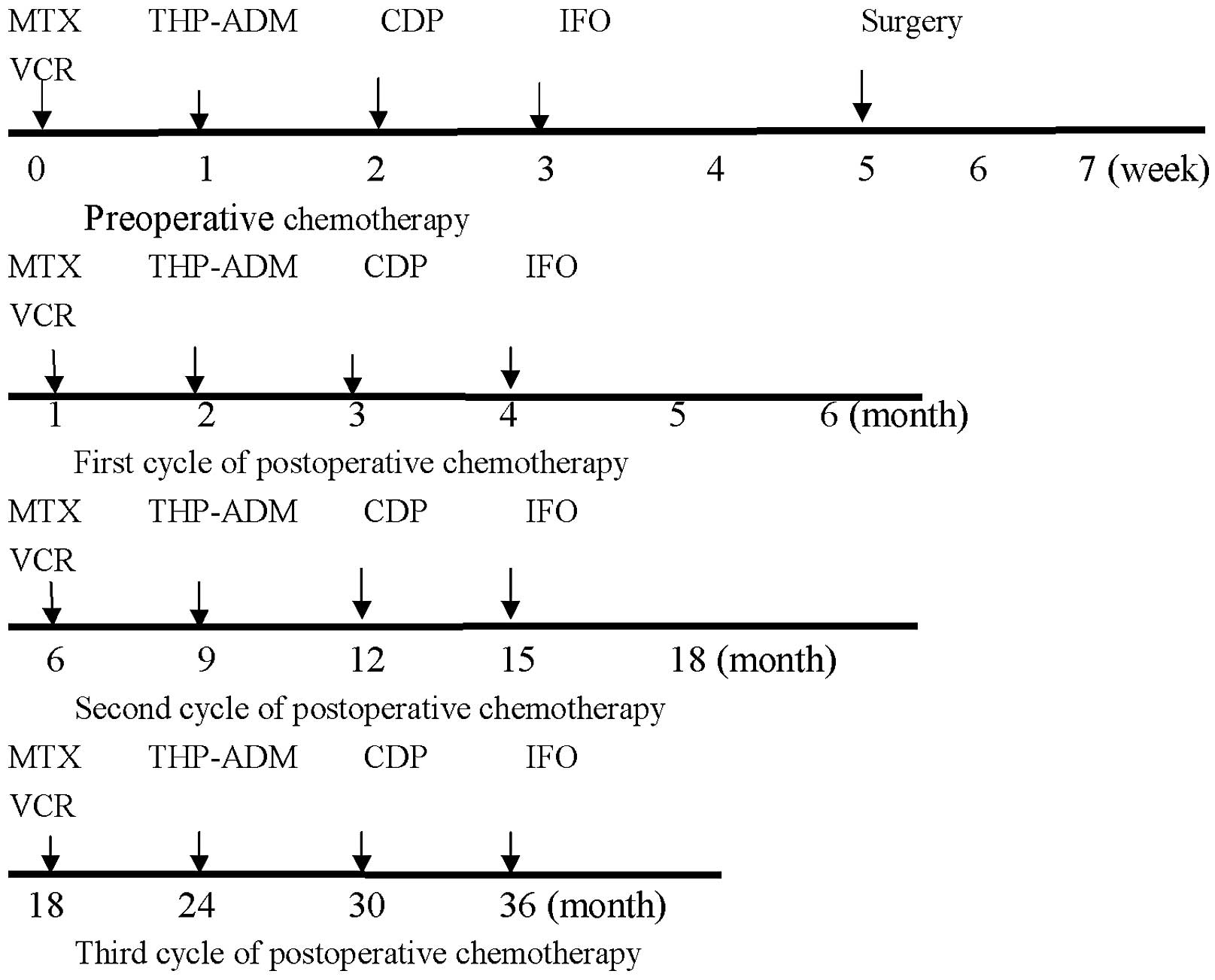
All four drugs active against osteosarcoma,
cisplatin (CDP), pirarubicin (THP-ADM), methotrexate (MTX) and
cyclofosfamide (IFO), were employed. Treatment was performed
according to the protocol used at the time of enrollment with
adjustment for Chinese racial characteristics. Chemotherapy
consisted of 1 cycle of MTX (12 g/m2/day; 1 day),
THP-ADM (40 mg/m2/day; 3 days), CDP 100
mg/m2/day; 1 day) and IFO (3 g/m2/day; 5
days) preoperatively and 3 cycles postoperatively (Fig. 1). MTX was administered as a 4 h
infusion with 11 doses of leucovorin (folinic acid) as rescue (8
mg/m2) every sixth hour, beginning 24 h after starting
the MTX infusion. Vincristine (VCR; 1.4 mg/m2) was
delivered two days after the MTX. IFO was in combination with an
equal amount of mesna. All drugs were given as single agents.
Complete blood counts and renal and liver function
were monitored before each chemotherapy cycle and following
infusion. The blood count was monitored twice a week starting on
day 1-2 from the start of chemotherapy. No dose reductions were
allowed and if the absolute granulocyte count was ≤1,000/μl
(500 for MTX cycles) and/or the platelet count was
≤100,000/μl (60,000 for MTX cycles), chemotherapy was
delayed until recovery. Granulocyte colony-stimulating factor
(G-CSF) and IL-11 support was given according to ASCO guidelines
(1994). Component blood transfusion was used as a favorable measure
in cases of severe marrow suppression.
Statistical analysis
The potential significance of age at the diagnosis
of cancer (<20), gender (female), malnutrition, Karnofsky
Performance Status (KPS) score (<60), leukopenia before
chemotherapy (<4.0×109/l), tumor staging (III), lung
metastasis, the number of previous chemotherapies (>3) and
combination chemotherapy of >3 drugs were evaluated. For
univariate analysis, Pearson’s χ2 test and one-way ANOVA
were used. Factors were kept in the model if the P-value was
<0.05. The analysis was performed with SPSS 18.0 software (SPSS
Inc. Chicago, IL, USA). For multivariate analysis, factors which
were statistically significant were included in the multivariate
logistic regression analysis.
Results
Patients
In 113 patients, 68 patients (group A) experienced
grade III/IV hematological toxicity and the probability of
occurrence was 60.18%. Three of the patients among the remainder
did not experience any episode of bone marrow suppression. The
number of patients with anemia was low. There was no
treatment-related mortality (Table
II).
 | Table IINumber of patients and the probability
of bone marrow suppression. |
Table II
Number of patients and the probability
of bone marrow suppression.
| Bone marrow
suppression | No. of patients | Probability (%) |
|---|
| Neutropenia (grade
I/II) | 45 | 39.82 |
| Neutropenia (grade
III/IV) | 68 | 5.31 |
| Thrombocytopenia
(grade I/II) | 6 | 60.18 |
| Thrombocytopenia
(grade III/IV) | 13 | 11.50 |
| Anemia (grade
I/II) | 11 | 9.73 |
| Anemia (grade
III/IV) | 7 | 6.19 |
Statistical analysis
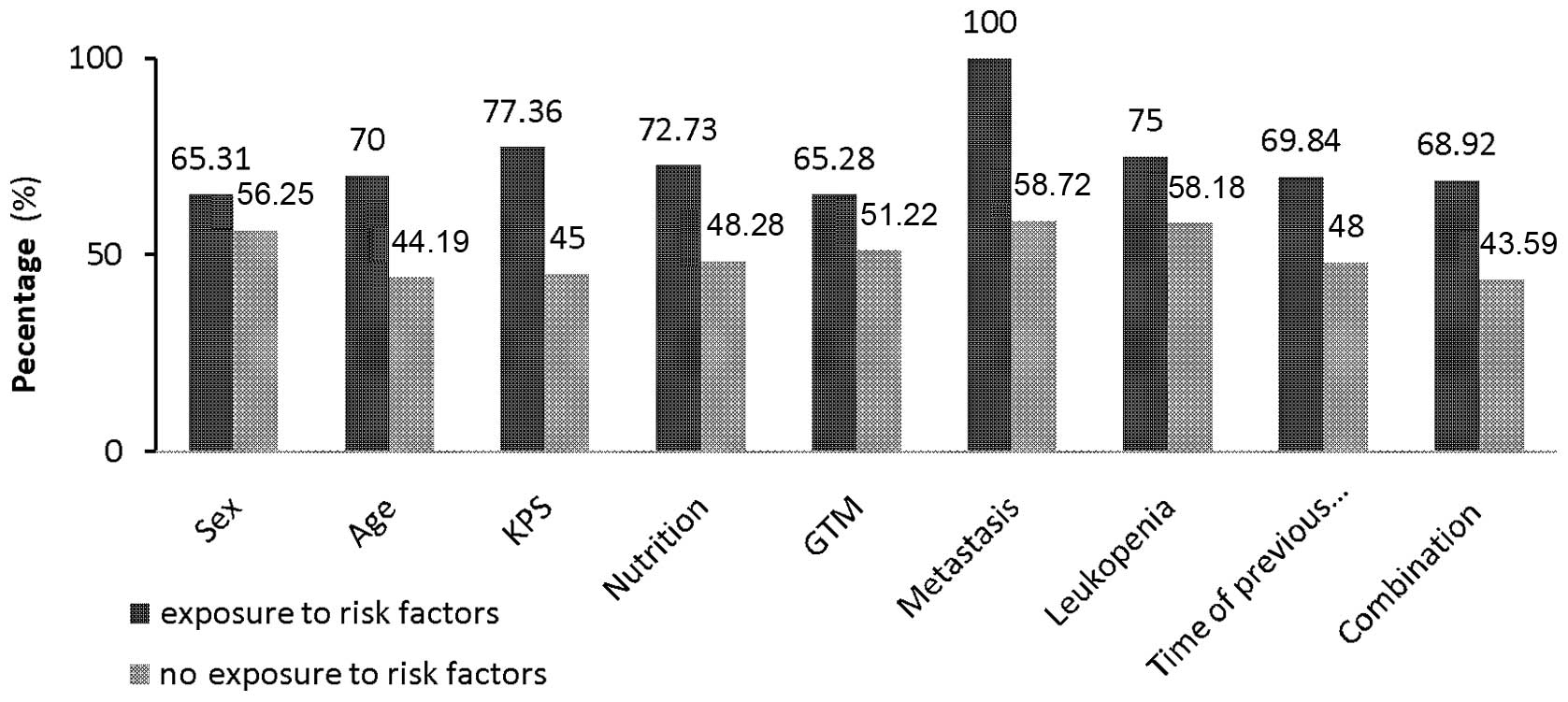
Univariate analysis revealed correlations similar to
those shown using multivariate analysis. Fig. 2 shows the correlation between
potential risk factors and the occurrence of grade III/IV
neutropenia. For univariate analysis (Table III), the results of the Pearson
χ2 test are consistent with those of the one-way ANOVA
analysis (results not shown). Factors such as age (<20), KPS
score (<60), malnutrition, number of previous chemotherapy
regimens >3, leucopenia before chemotherapy
(<4.0×109/l) and combination chemotherapy with >3
drugs were associated with the occurrence of grade III/IV
neutropenia. In the multivariate analysis (Table IV), leucopenia before chemotherapy
(<4.0×109/l) was not statistically significant.
 | Table IIIResults of univariate analysis
(Pearson’s χ2 test). |
Table III
Results of univariate analysis
(Pearson’s χ2 test).
| Potential
factors | Group A (n) | Group B (n) | Probability (%) | χ2 | OR | OR 95% CI | P-value |
|---|
| Gender | | | | | | | |
| Male | 36 | 28 | 56.25 | | | | |
| Female | 32 | 17 | 65.31 | 0.950 | 1.464 | 0.679–3.156 | >0.05 |
| Age | | | | | | | |
| <20 | 49 | 21 | 70.00 | 7.407 | 0.339 | 0.154-0.747 | <0.01 |
| ≥20 | 19 | 25 | 44.19 | | | | |
| KPS score | | | | | | | |
| <60 | 41 | 12 | 77.36 | 12.296 | 0.239 | 0.105–0.544 | <0.05 |
| ≥60 | 27 | 33 | 45.00 | | | | |
| Tumor staging
(Enneking) | | | | | | | |
| G1/2T1/2M1 | 47 | 25 | 65.28 | | | | |
| G1/2T1/2M0 | 21 | 20 | 51.22 | 2.154 | 1.790 | 0.820–3.911 | >0.05 |
| Nutrition | | | | | | | |
| Good | 40 | 15 | 72.73 | 7.043 | 2.857 | 1.302–6.269 | <0.01 |
| Poor | 28 | 30 | 48.28 | | | | |
| Lung
metastasis | | | | | | | |
| Metastatic | 4 | 0 | 100.00 | 2.744 | 0.587 | 0.502–0.687 | >0.05 |
| Local | 64 | 45 | 58.72 | | | | |
| Leucopenia before
chemotherapy | | | | | | | |
| Abnormal | 36 | 12 | 75.00 | 7.651 | 3.094 | 1.370–6.985 | <0.01 |
| Normal | 32 | 33 | 49.23 | | | | |
| No. of previous
chemotherapies | | | | | | | |
| >3 | 44 | 19 | 69.84 | 5.549 | 2.509 | 1.158–5.543 | <0.05 |
| 0–3 | 24 | 26 | 48.00 | | | | |
| Combination
chemotherapy | | | | | | | |
| 1–3 | 17 | 22 | 43.59 | | | | |
| >3 | 51 | 23 | 68.92 | 6.837 | 2.870 | 1.287–6.398 | <0.05 |
 | Table IVResults of multivariate analysis
(multivariate logistic regression analysis). |
Table IV
Results of multivariate analysis
(multivariate logistic regression analysis).
| Factors | B | SE | OR | OR 95% CI | Wald | P-value |
|---|
| Age (<20) | −2.151 | 0.628 | 0.116 | 0.034–0.398 | 11.730 | 0.001 |
| KPS score
(<60) | −2.249 | 0.611 | 0.105 | 0.032–0.349 | 13.540 | 0.000 |
| Malnutrition | 1.332 | 0.593 | 3.787 | 1.184–12.109 | 5.040 | 0.025 |
| Leucopenia before
chemotherapy | 0.018 | 0.565 | 1.019 | 0.337–3.081 | 0.001 | 0.974 |
| No. of previous
chemotherapies (>3) | 1.245 | 0.673 | 3.474 | 1.004–12.019 | 3.868 | 0.049 |
| Combination
chemotherapy (>3) | 1.815 | 0.597 | 6.142 | 1.905–19.803 | 9.234 | 0.004 |
Discussion
In this retrospective study it was found that age
<20 years, KPS score <60, malnutrition, >3 previous
chemotherapies and combination therapy of >3 drugs were
significantly associated with the occurrence of severe bone marrow
suppression, mainly indicated by grade III/IV neotropenia. The
degree of myelosuppression with relative dose instensity in the
same or similar regimens varied greatly, making it difficult to
determine the actual risk of neutropenic complications associated
with common chemotherapy regimens (15). Treatment dose intensity has also
been less consistent, making it difficult to interpret differences
in reported toxicity or treatment efficacy. This, in the present
study, the chemotherapy regimen was consistent but the dosages of
drugs have not been included.
Patients younger than 20 years appear to be more
vulnerable to the adverse effects of chemotherapy treatment for
bone and soft tissue sarcoma. Ten studies found higher age to be a
general risk factor for the development of severe neutropenia
(16–22) and other neutropenic complications
(23–25). Since older patients are often
treated with lower chemotherapy doses to minimize the occurrence of
neutropenic complications, advanced age is a particularly important
independent risk factor. These studies mainly focused on tumors of
non-Hodgkin’s lymphoma (NHL) and breast cancer, however, and the
number of patients with bone and soft tissue sarcoma were rare.
Bone malignancy, especially osteosarcoma, often occurs in young
adolescents. This difference could be due to the inhibition of the
hematopoietic system by drugs, especially high-dose Methotrexate
(HD-MTX) and THP-ADM. This can be accentuated in younger children
whose immature hematopoietic system as well as their great
capability for proliferation and differentiation of hematopoietic
stem cells makes them more susceptible to the toxicity of
chemotherapy. It is possible that higher levels of drugs in tissues
and blood occur in younger patients because of their higher
percentage of body fat.
In developing countries, due to uneven economic
development and imperfect health care systems, malnutrition is
common. In malnourished patients, due to poor physical fitness, the
toxicity of chemotherapy is tolerated in varying degrees which may
be the reason for the higher probability of occurrence of severe
bone marrow suppression.
KPS is widely used to quantify the functional status
of cancer patients. Studies have shown that, in addition to age,
poor performance status is a significant risk factor for
chemotherapy-induced neutropenia (26,27).
Physiological age or frailty may be a more accurate predictor of
risk than chronological age, especially in older patients (28). In the present study, patients with a
lower KPS score (<60) were more likely to experience severe bone
suppression than those above 60.
The findings suggest that chemotherapy is better
tolerated by patients with >3 previous chemotherapies compared
with those who received it once or twice. Peripheral neuropathy
manifests with paresthesia and hearing loss for high frequencies
due to CDP at cumulative doses of 300-600 mg/m2(29). It is possible that hematological
toxicity results from accumulation of the drug.
The intensity of specific chemotherapy regimens is
one of the primary determinants of the risk for severe neutropenia,
with some regimens being more myelosuppressive than others
(30). High IFO dose or the use of
etoposide in treating patients with NHL (16,31)
and high anthracycline doses in treating patients with early-stage
breast cancer (19,32) have all been identified as
significant predictors for severe neutropenia and febrile
neutropenia (FN). The combination of four drugs (HD-MTX, THP-ADM,
CDP, IFO) in the present study showed an increasing risk of severe
bone marrow suppression compared with a three-drug regimen. In
light of this, the development of equally effective but less
intensive regimens for patients whose disease carries a better
prognosis is highly desirable. Ongoing clinical trials are
investigating this strategy.
In 1978, Rosen introduced neoadjuvant (preoperative)
chemotherapy (33). The goals of
neoadjuvant chemotherapy, besides the eradication of
micrometastasis, include the destruction of primary tumor cells
with reduction of tumor burden and the possibility to evaluate the
histologic response to preoperative chemotherapy. At present,
neoadjuvant (preoperative) chemotherapy followed by definitive
resection with subsequent adjuvant (postoperative) chemotherapy is
the well-established approach to the treatment of localized
osteosarcomas. Chemotherapy may eradicate the micrometastatic
disease that is believed to be present in the majority of patients
with clinically resectable cancer. Almost half of young adult
survivors of childhood cancer have at least one major adverse
outcome as a result of their cancer therapy (34). Chemotherapy-induced bone marrow
suppression is the major dose-limiting toxicity of systemic cancer
chemotherapy and it is associated with substantial morbidity,
mortality and costs. The purpose of the present study was to find
the risk factors of severe bone marrow suppression, which may
contribute to improve clinical outcomes. The use of such risk
factors would be to identify the patients with bone and soft tissue
sarcoma who are at greatest risk of neutropenia and target
prophylactic colony-stimulating factors (CSFs) to those patients.
This should help providers focus resources on those who are at most
risk. The present study results, however, are limited by the
retrospective design, small population studied and the various risk
factors and methods used. Also it is reported that pretreatment WBC
counts are predictive of both FN and a relative dose intensity
<85% in patients with early-stage breast cancer (15,20).
Pretreatment hemoglobin levels <12 g/dl are also predictors of
severe neutropenia or FN in cycle 1 (20). In the present study, leukopenia
before chemotherapy was of no significance. To overcome these
limitations, a prospective registry of different tumor types has
been designed, which should make it possible to develop accurate
and valid risk models for severe bone suppression in
chemotherapy.
References
|
1
|
Link MP, Goorin AM, Miser AW, Green AA,
Pratt CB, Belasco JB, et al: The effect of adjuvant chemotherapy on
relapse-free survival in patients with osteosarcoma of the
extremity. N Engl J Med. 314:1600–1606. 1986. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Fuchs N, Bielack SS, Epler D, Bieling P,
Delling G, Korcholz D, et al: Long-term results of the co-operative
German-Austrian-Swiss osteosarcoma study group’s protocol COSS-86
of intensive multidrug chemotherapy and surgery for osteosarcoma of
the limbs. Ann Oncol. 9:893–899. 1998.PubMed/NCBI
|
|
3
|
Bacci G, Ferrari S, Bertoni F, Ruggieri P,
Picci P, Longhi A, et al: Long-term ourcome for patients with
nonmetastatic osteosarcoma of the extremity treated at the istituto
ortopedico Rizzoli according to the institute orotpedico
Rizzoli/osteosarcoma-2 protocol: an update report. J Clin Oncol.
18:4016–4627. 2000.
|
|
4
|
Bielack S, Kempf-Bielack B, Delling G,
Exner GU, Flege S, Helmke K, et al: Prognositic factors in
high-grade osteosarcoma of the extremities or trunk: An analysis of
1,702 patients treated on neoadjuvant cooperative osteosarcoma
study group protocols. J Clin Oncol. 20:776–790. 2002. View Article : Google Scholar
|
|
5
|
Smeland S, Müller C, Alvegaard TA, Wiklund
T, Wiebe T, Bjork O, et al: Scandinavian Sarcoma Group Osteosarcoma
study SSG VIII: prognostic factors for outcome and the role of
replacement salvage chemotherapy for poor histological responders.
Eur J Cancer. 39:488–494. 2003. View Article : Google Scholar
|
|
6
|
Ferrari S, Smeland S, Mercuri M, Bertoni
F, Longhi A, Ruggieri P, et al: Neoadjuvant chemotherapy with
high-dose Ifosfamide, high-dose methotrexate, cisplatin, and
doxorubicin for patients with localized osteosarcoma of the
extremity: a joint study by the Italian and Scandinavian sarcoma
groups. J Clin Oncol. 23:8845–8852. 2005. View Article : Google Scholar
|
|
7
|
Ozer H, Armitage JO, Bennett CL, Crawford
J, Demetri GD, Pizzo PA, et al: 2000 update of recommendations for
the use of hematopoietic colony-stimulating factors:
evidence-based, clinical practice guidelines. American Society of
Clinical Oncology Growth Factors Expert Panel. J Clin Oncol.
18:3558–3385. 2000.
|
|
8
|
Rolston KV: New trends in patient
management: risk-based therapy for febrile patients with
neutropenia. Clin Infect Dis. 29:515–521. 1999. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Bonadonna G, Valagussa P, Molitemi A,
Zambetti M and Brambilla C: Adjuvant cyclophosphamide,
methotrexate, and fluorouracil in node-positive breast cancer: the
results of 20 years of follow-up. N Engl J Med. 332:901–906.
1995.PubMed/NCBI
|
|
10
|
Budman DR, Berry DA, Cirrincione CT,
Henderson IC, Wood WC, Weiss RB, et al: Dose and dose intensity as
determinants of outcome in the adjuvant treatment of breast cancer.
The Cancer and Leukemia Group B. J Natl Cancer Inst. 90:1205–1211.
1998. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Kwak LW, Halpern J, Olshen RA and Horning
SJ: Prognostic significance of actual dose intensity in diffuse
large-cell lymphoma: results of a tree-structured survival
analysis. J Clin Oncol. 8:963–977. 1990.PubMed/NCBI
|
|
12
|
Talcott JA, Siegel RD, Finberg R and
Goldman L: Risk assessment in cancer patients with fever and
neutropenia: A prospective two center validation of a prediction
rule. J Clin Oncol. 10:316–322. 1992.PubMed/NCBI
|
|
13
|
Blay JY, Chauvin F, Le Cesne A, Anglaret
B, Bouhour D, Lasset C, et al: Early lymphopenia after cytotoxic
chemotherapy as a risk factor for febrile neutropenia. J Clin
Oncol. 14:636–643. 1996.PubMed/NCBI
|
|
14
|
Coiffier B, Gisselbrecht C, Herbercht R,
Tilly H, Bosly A and Brousse N: LNH-84 regimen: a multicenter study
of intensive chemotherapy in 737 patients with aggressive malignant
lymphoma. J Clin Oncol. 7:1018–1026. 1989.PubMed/NCBI
|
|
15
|
Dale DC, McCarter GC, Crawford J and Lyman
GH: Myelotoxicity and dose intensity of chemotherapy: reporting
practices from randomized clinical trials. J Natl Compr Canc Netw.
1:440–454. 2003.PubMed/NCBI
|
|
16
|
Kloess M, Wunderlich A and Trumper L:
Predicting hematotoxicity in multicycle chemotherapy. Blood.
94(Suppl 1): 87a1999.
|
|
17
|
Lyman GH, Morrison VA, Dale DC, Crawford
J, Delgado DJ, Fridman M, et al: Risk of febrile neutropenia among
patients with intermediate-grade non-Hodgkin’s lymphoma receiving
CHOP chemotherapy. Leuk Lymphoma. 44:2069–2076. 2003.
|
|
18
|
Morrison VA, Picozzi V, Scott S, Pohlman
B, Dickman E, Lee M, et al: The impact of age on delivered dose
intensity and hospitalizations for febrile neutropenia in patients
with intermediate-grade non-Hodgkin’s lymphoma receiving initial
CHOP chemotherapy: a risk factor analysis. Clin Lymphoma. 2:47–56.
2001.PubMed/NCBI
|
|
19
|
Lyman GH, Dale DC, Friedberg J, Crawford J
and Fisher RI: Incidence and predictors of low chemotherapy
dose-intensity in aggressive non-Hodgkin’s lymphoma: a nationwide
study. J Clin Oncol. 22:4302–4311. 2004.PubMed/NCBI
|
|
20
|
Morrison VA, Caggiano V, Fridman M, Dale
DC, Crawford J, Delagado DJ, et al: A model to predict
chemotherapy-related severe or febrile neutropenia in cycle one
among breast cancer and lymphoma patients. Proc Am Soc Clin Oncol.
23:7422004.
|
|
21
|
Aslani A, Smith RC, Allen BJ, Pavlakis N
and Levi JA: The predictive value of body protein for
chemotherapy-induced toxicity. Cancer. 88:796–803. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Lyman GH, Dale DC and Crawford J:
Incidence and predictors of low dose-intensity in adjuvant breast
cancer chemotherapy: a nationwide study of community practices. J
Clin Oncol. 21:4524–4531. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Klastersky J, Paesmans M, Rubenstein EB,
Boyer M, Elting L, Feld R, et al: The multinational association for
supportive care in cancer risk index: a multinational scoring
system for identifying low-risk febrile neutropenic cancer
patients. J Clin Oncol. 18:3038–3051. 2000.PubMed/NCBI
|
|
24
|
Kuderer NM, Dale DC, Crawford J, Cosler LE
and Lyman GH: Mortality, morbidity, and cost associated with
febrile neutropenia in adult cancer patients. Cancer.
106:2258–2266. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Kim YJ, Rubenstein EB and Rolston KV:
Colony stimulating factors (CSFs) may reduce complications and
death in solid tumor patients (Pts) with fever and neutropenia.
Proc Am Soc Clin Oncol. 19:612a2000.
|
|
26
|
Voog E, Bienvenu J, Warzocha K, Moullet I,
Dumontet C, Thieblemont C, et al: Factors that predict
chemotherapy-induced myelosuppression in lymphoma patients: role of
the tumor necrosis factor ligand-receptor system. J Clin Oncol.
18:325–331. 2000.PubMed/NCBI
|
|
27
|
Silber JH, Fridman M, DiPaola RS, Erder
MH, Pauly MV and Fox KR: First-cycle blood counts and subsequent
neutropenia, dose reduction, or delay in early-stage breast cancer
therapy. J Clin Oncol. 16:2392–2400. 1998.PubMed/NCBI
|
|
28
|
Bladucci L and Extermann M: Cancer and
aging. An evolving panorama. Hematol Oncol Clin North Am. 14:1–16.
2000. View Article : Google Scholar
|
|
29
|
Cvitkovic E: Cumulative toxicity from
cisplatin therapy and current cytoprotective measures. Cancer Treat
Rev. 24:265–281. 1998. View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Blay JY, Chauvin F, Le Cesne A, Anglaret
B, Bouhour D, Lasset C, et al: Early lymphopenia after cytotoxic
chemotherapy as a risk factor for febrile neutropenia. J Clin
Oncol. 14:636–643. 1996.PubMed/NCBI
|
|
31
|
Voog E, Bienvenu J, Warzocha K, Moullet I,
Dumontet C, Thieblemont C, et al: Factors that predict
chemotherapy-induced myelosuppression in lymphoma patients: role of
the tumor necrosis factor ligand-receptor system. J Clin Oncol.
18:325–331. 2000.PubMed/NCBI
|
|
32
|
Szucs TD, Leonard R and Pettengell R:
Dose-limiting effects of neutropenic events in six European audits
of adjuvant breast cancer chemotherapy. Proc Am Soc Clin Oncol.
24:312004.
|
|
33
|
Rosen G, Caparros B, Huvos AG, Kosloff C,
Nirenberg A, Cacavio A, et al: Preoperative chemotherapy for
osteogenic sarcoma: selection of postoperative adjuvant
chemotherapy based on the response of the primary tumor to
preoperative chemotherapy. Cancer. 15:1221–1230. 1982. View Article : Google Scholar
|
|
34
|
Offinger KC and Hudson MM: Long term
complications following childhood and adolescent cancer:
foundations for providing Risk-based health care for survivors. CA
Cancer J Clin. 54:208–236. 2004. View Article : Google Scholar : PubMed/NCBI
|