Introduction
Cancer arises from the uncontrolled dissemination
and spread of clones of transformed cells, which should be
recognized by the immune system before transforming into a tumor.
Although it has been demonstrated that the immune system reacts to
many tumors and at least slows down the progression, it is not yet
known how immune reactions are used to destroy tumors in a specific
manner. Moreover, one must take into account the capacity of tumor
cells to evade or overcome the defense mechanisms of the host
(1). Remodeling of the
extracellular matrix and basal membrane confined to the
pericellular microenvironment may be the first step toward invasion
(2). Escape from the action of the
immune system results in the rapid progression of cancer, requiring
immunotherapy to potentiate the antitumor response of the host and
avoid dissemination (3).
The effector mechanisms of the immune response begin
with the bonding of a signaling agent to a specific receptor on the
cell surface, which sends signals to the nucleus through signal
transduction pathways, where regulating factors known as
transcription factors promote specific alterations in the
regulation of gene expression.
Nuclear factor κ-light chain enhancer of activated
B-cells (NF-κB) is a transcription factor activated in response to
signals from the T-cell receptor (TCR) and is essential in the
synthesis of cytokines. In the resting T-cell, this protein is
found in the cytoplasm associated with inhibitor proteins (IκBs).
Signals from the TCR induce phosphorylation via IκB kinases, which
is followed by the insertion of multiple copies of a small protein
called ubiquitin, which releases NF-κB. This enters the nucleus
where it contributes to the transcriptional activation of several
genes of cytokines and cytokine receptors. NF-κB is involved in the
activation of T-cells, contributing to the transcription of
interleukin 2 (IL-2) and the response of many cell types to
pro-inflammatory cytokines, such as tumor necrosis factor (TNF),
IL-1 and bacterial lipoproteins (4).
The maintenance of activated NF-κB during
inflammation predisposes a tumor to malignant transformation. NF-κB
could be used to inhibit tumor transformation, but for such it
would be necessary to interfere in its physiological role in both
immunity and/or inflammation and homeostasis (5).
Human tumors activate cluster of differentiation 4
(CD4) or CD8 lymphocytes, depending on the processing pathway for
triggering the immune response. Control of the tumor depends both
on the magnitude of the initial immune response and the capacity to
sustain this response for a prolonged period of time (6). The main antitumor defense mechanism is
the death of tumor cells by CD8 T-lymphocytes, also known as
cytotoxic T-lymphocytes. They have the ability to recognize and
kill potentially malignant cells that express peptides derived from
mutant cell proteins or oncogenic viral proteins associated with
major histocompatability complex (MHC) class I.
The Treg cell line is a T-lymphocyte subtype that
has the role of inducing and maintaining immunological tolerance
and the finalization of the immune response. A deficiency or
reduction in this cell type leads to an auto-immune disease
(7,8). However, a group of adaptable Treg
cells (Th3) become mature in peripheral tissues under antigen
stimulation and/or co-stimulation, exercising a suppressive
function through the secretion of IL-10 and transforming growth
factor-β (TGF-β).
Forkhead box P3 (FOXP3) is a protein responsible for
the regulation of the function and development of Treg cells and
has been used in their detection (9–11).
According to Hori et al(7),
FOXP3 is the best marker for Treg cells.
In normal tissue, TGF-β regulates cell growth and
differentiation. The autocrine reduction of TGF-β in keratinocytes
has been found to lead to papillomatous lesions that transform into
carcinomas (12). The cancer cells
develop partial or complete resistance to this inhibition, however
(13). TGF-β often functions as a
tumor suppressor in the early stages of carcinogenesis and later
becomes a promoter in the progression of the tumor and metastasis
(14,15). The negative regulation or damage to
the disposition of the receptors on the surface of cytolytic
T-lymphocytes allows tumor cells to escape the inhibitory effects
of TGF-β (16).
This study assessed the role of inflammation in oral
carcinogenesis through the investigation of cellular markers,
cytokines and nuclear transcription factors that identify the cells
that participate in antitumor defense in cases of oral epithelial
dysplasia (OED) and oral squamous cell carcinoma (OSCC).
Materials and methods
Selection criteria
A total of 20 cases of OED and 40 cases of OSCC were
randomly selected from the archives of the Pathological Anatomy
Service of the Federal University of Sergipe and the Pathological
Anatomy Laboratory of the Oral Pathology Sector of the Federal
University of Rio Grande do Norte in Brazil. The study received
approval from the Research Ethics Committee of the latter
institution (process no. 233/2007).
Histology
The hematoxylin and eosin-stained slides were viewed
under a light microscope and examined in a double-blind manner by
two histopathologists. The criteria of the World Health
Organization (WHO) were used for the histological grading of the
dysplasia (17). Carcinomas were
classified as stage I (low-grade) or stage II (high-grade)
according to the method proposed by Piva et al(18).
Immunohistochemistry
Immunohistochemical analysis was performed for CD8,
FOXP3, TGF-β, TNF-α and NF-κB in cases of dysplasia and carcinoma.
Paraffin-embedded specimens were cut (3 μm) and the slices
were mounted on glass slides prepared with an organosilane-based
adhesive (3-amino-propyltriethoxysilane, Sigma Chemical Co., St.
Louis, MO, USA). Antibodies directed against the proteins studied
were applied to the histological slices, according to the
specifications displayed in Table
I. For negative controls, the primary antibodies were omitted.
For positive controls, previously tested breast cancer and
periapical granuloma specimens were used. Following the
classification of the cases as dysplasia and carcinoma, a
semi-quantitative analysis was performed on the markers, cytokines
and nuclear transcription factor expression, with reactions of a
brown coloration considered positive, regardless of intensity. The
percentage of positive cells was calculated for CD8 and FOXP3 for
stromal cells, NF-κB for epithelial cells and TGF-β and TNF-α for
both epithelial and stromal cells. Labeled cells were classified as
low expression with <5%, as moderate expression with 5–50% and
as high expression with >50%, following the criteria proposed by
Abbas et al(19).
 | Table ISpecifications of primary
antibodies. |
Table I
Specifications of primary
antibodies.
| Antibody | Clone time |
Dilution/Incubation | Antigen recovery | Method |
|---|
| NF-κBa | NF-κB p65 (A) | 1:100/3 h | Citrate | Envision-HRPb |
| TNF-αa | TNF-α (2C8) | 1:100/Overnight | Pepsin | Envision-HRPb |
| TGF-βa | TGF-β1 (V) | 1:500/Overnight | Pepsin | Envision-HRPb |
| FOXP3a | FOXP3 (H190) | 1:100/Overnight | Tris-EDTA, pH
9.0 | Envision-HRPb |
| CD8b | C8/144B | 1:200/60 min | Tris-EDTA, pH
9.0 | SABCb |
Statistical analysis
The statistical analysis was performed using SPSS
13.0 for Windows (SPSS Inc., Chicago, IL, USA). The Mann-Whitney U
test was used to determine the hypothesis of equality in the
expression of the markers, cytokines and nuclear transcription
factors in relation to the type of lesion and histological grade of
carcinoma. The Kruskal-Wallis test was used to compare the
expression of CD8, FOXP3, TGF-β, TNF-α and NF-κB between the grades
of dysplasia. The Spearman’s rank correlation coefficient was used
to investigate the correlation between inflammatory infiltrate
intensity and positivity of CD8, FOXP3, TGF-β, TNF-α and NF-κB.
P<0.05 was considered to indicate a statistically significant
result.
Results
Histology and immunohistochemistry
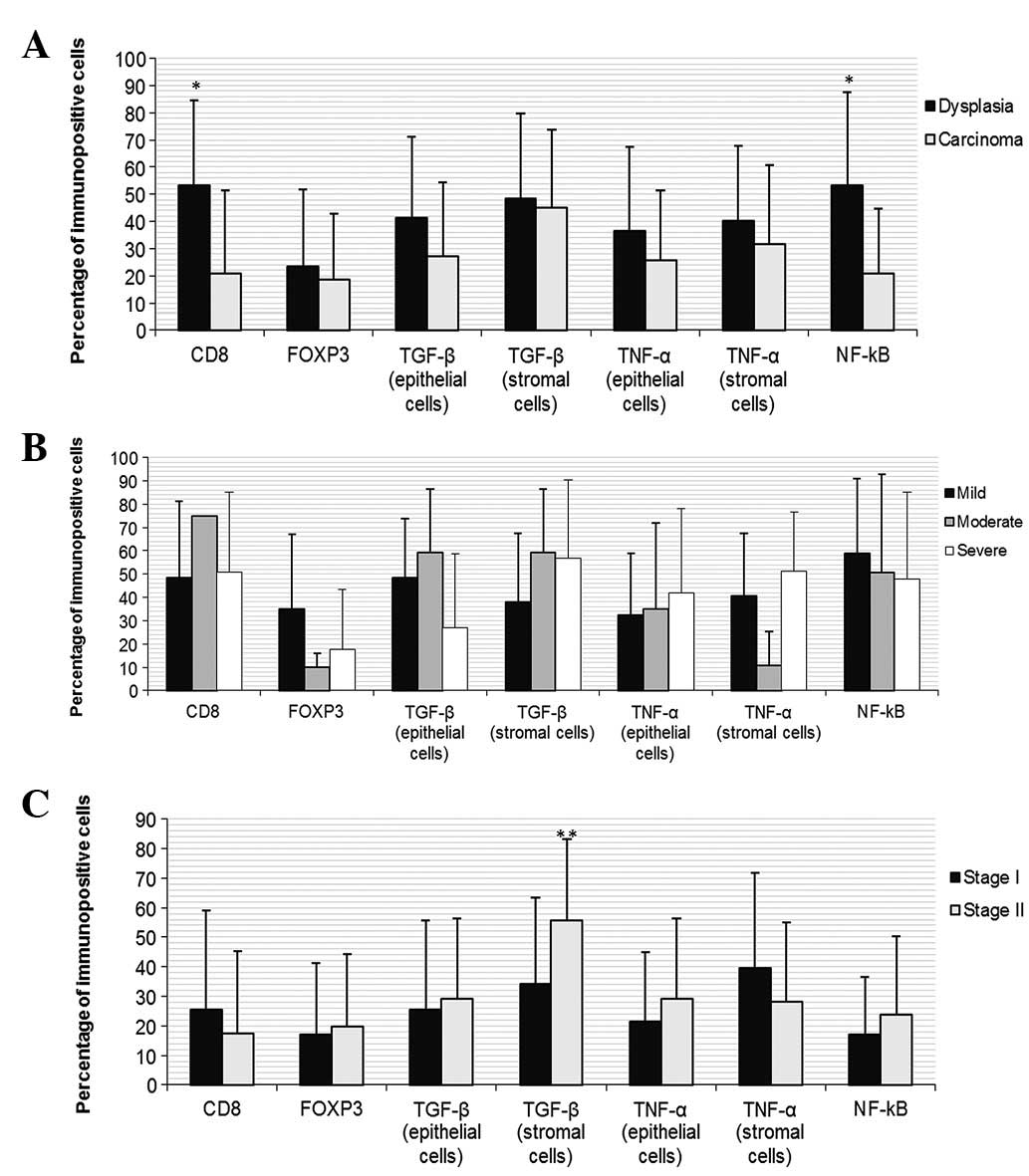
CD8 and NF-κB expression were found to be
significantly higher in the dysplasia group (Fig. 1A). However, no differences were
noted in the expression of CD8, FOXP3, TGF-β, TNF-α and NF-κB
between degrees of dysplasia (Fig.
1B). The immunohistochemical expression of cellular markers,
cytokines and nuclear transcription factor was no different between
stages of carcinoma, with the exception of the stromal TGF-β, which
was higher in stage II lesions (Fig.
1C).
TNF-α in both epithelial and stromal cells and NF-κB
exhibited a direct, statistically significant correlation with the
intensity of the inflammatory infiltrate in the cases of dysplasia.
In the cases of carcinoma, the intensity of the inflammatory
infiltrate was directly and significantly correlated with CD8 and
stromal TNF-α expression. In contrast, an inverse correlation
between the inflammatory infiltrate and the expression of
epithelial TNF-α was observed in carcinomas (Table II).
 | Table IICorrelation between inflammatory
infiltrate intensity and expression of cluster of differentiation 8
(CD8), forkhead box P3 (FOXP3), transforming growth factor-β
(TGF-β), tumor necrosis factor-α (TNF-α) and nuclear factor-κ-light
chain enhancer of activated B-cells (NF-κB). |
Table II
Correlation between inflammatory
infiltrate intensity and expression of cluster of differentiation 8
(CD8), forkhead box P3 (FOXP3), transforming growth factor-β
(TGF-β), tumor necrosis factor-α (TNF-α) and nuclear factor-κ-light
chain enhancer of activated B-cells (NF-κB).
|
Inflammatory
infiltrate intensity |
|---|
|
|---|
| Dysplasia (n=20) | Carcinoma (n=40) |
|---|
|
|
|---|
| Expression (%) | Mild n (%) | Mod. n (%) | Int. n (%) | Total | r | P-value | Mild n (%) | Mod. n (%) | Int. n (%) | Total | r | P-value |
|---|
| CD8 | | | | | | | | | | | | |
| <5 | 2 (40) | 1 (10) | 1 (20) | 4 (20) | | | 11 (100) | 6 (60) | 10 (50) | 27 (67.5) | | |
| 5–50 | 2 (40) | 2 (20) | 0 (0) | 4 (20) | 0.391 | NS | 0 (0) | 1 (10) | 2 (10) | 3 (7.5) | 0.365 | <0.05a |
| >50 | 1 (20) | 7 (70) | 4 (80) | 12 (60) | | | 0 (0) | 2 (20) | 8 (40) | 10 (25) | | |
| FOXP3 | | | | | | | | | | | | |
| <5 | 3 (60) | 6 (60) | 2 (40) | 11 (55) | | | 7 (63.6) | 6 (60) | 11 (57.9) | 24 (60) | | |
| 5–50 | 1 (20) | 2 (20) | 2 (40) | 5 (25) | 0.109 | NS | 2 (18.2) | 3 (30) | 6 (31.6) | 11 (27.5) | 0.018 | NS |
| >50 | 1 (20) | 2 (20) | 1 (20) | 4 (20) | | | 2 (18.2) | 1 (10) | 2 (10.5) | 5 (12.5) | | |
| TGF-β (epithelial
cells) | | | | | | | | | | | | |
| <5 | 1 (20) | 3 (30) | 0 (0) | 4 (20) | | | 4 (36.4) | 3 (30) | 9 (47.4) | 16 (40) | | |
| 5–50 | 1 (20) | 4 (40) | 3 (60) | 8 (40) | 0.026 | NS | 3 (27.2) | 5 (50) | 6 (31.6) | 14 (35) | −0.142 | NS |
| >50 | 3 (60) | 3 (40) | 2 (40) | 8 (40) | | | 4 (36.4) | 2 (20) | 4 (21) | 10 (25) | | |
| TGF-β (stromal
cells) | | | | | | | | | | | | |
| <5 | 0 (0) | 4 (40) | 0 (0) | 4 (20) | | | 3 (27.2) | 2 (20) | 2 (10.5) | 7 (17.5) | | |
| 5–50 | 2 (40) | 1 (10) | 2 (40) | 5 (25) | 0.000 | NS | 4 (36.4) | 3 (30) | 8 (42.1) | 15 (37.5) | 0.189 | NS |
| >50 | 3 (60) | 5 (50) | 3 (60) | 11 (55) | | | 4 (36.4) | 5 (50) | 9 (47.4) | 18 (45) | | |
| TNF-α (epithelial
cells) | | | | | | | | | | | | |
| <5 | 3 (60) | 2 (20) | 1 (20) | 6 (30) | | | 3 (27.3) | 1 (10) | 10 (52.6) | 14 (35) | | |
| 5–50 | 2 (40) | 4 (40) | 1 (20) | 7 (35) | 0.442 | <0.05a | 6 (54.5) | 6 (60) | 6 (31.6) | 18 (45) | −0.337 | <0.05a |
| >50 | 0 (0) | 4 (40) | 3 (60) | 7 (35) | | | 2 (18.2) | 3 (30) | 3 (15.8) | 8 (20) | | |
| TNF-α (stromal
cells) | | | | | | | | | | | | |
| <5 | 2 (40) | 1 (10) | 0 (0) | 3 (15) | | | 9 (81.8) | 3 (30) | 9 (47.4) | 21 (52.5) | | |
| 5–50 | 3 (60) | 6 (60) | 1 (20) | 10 (50) | 0.632 | <0.05a | 1 (9.1) | 5 (50) | 6 (31.6) | 12 (30) | 0.383 | <0.05a |
| >50 | 0 (0) | 3 (30) | 4 (80) | 7 (35) | | | 1 (9.1) | 2 (20) | 4 (21) | 7 (17.5) | | |
| NF-κB | | | | | | | | | | | | |
| <5 | 4 (80) | 2 (20) | 0 (0) | 6 (30) | | | 6 (54.5) | 6 (60) | 8 (42.1) | 20 (50) | | |
| 5–50 | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0.617 | <0.05a | 3 (27.3) | 2 (20) | 10 (52.6) | 15 (37.5) | 0.046 | NS |
| >50 | 1 (20) | 8 (80) | 5 (100) | 14 (70) | | | 2 (18.2) | 2 (20) | 1 (5.3) | 5 (12.5) | | |
Discussion
Comparative studies have demonstrated that
significant molecular alterations occur in the progression of OED
to invasive carcinoma, but not between histological grades of OSCC
(19). The present study
corroborates these findings, since the expression of cytokines was
higher in cases of dysplasia, although only CD8 and NF-κB showed
statistically significant differences. This result suggests that
the higher expression of CD8 in the inflammatory infiltrate in
dysplasia exercises a protective function, although the maintenance
of the stimulus and the differences in expression of other
cytokines, such as TNF-α and NF-κB, may favor transformation
followed by invasion. While the cases of dysplasia exhibited a
lesser quantity of this infiltrate, such cases demonstrated a
significant correlation between the intensity of the infiltration
and expression of TNF-α in both stromal and epithelial cells and
NF-κB.
According to Pacifico and Leonardi (5), the maintenance of activated NF-κB
during inflammation predisposes the lesion to malignant
transformation. This cytokine is involved in the activation of
T-cells, thereby contributing to the transcription of IL-2 and the
response of many cell types to pro-inflammatory cytokines, such as
TNF (4). In the present study, the
overexpression of NF-κB and epithelial TNF-α was positively
correlated to the intensity of the inflammatory infiltrate in
dysplasia. However, these results are in disagreement with those
described by Lind et al(20), who noted that the signaling mediated
by the TNF-α receptor (TNFR1) in keratinocytes is necessary for the
development of skin cancer induced by the inhibition of NF-κB. It
was postulated, therefore, that the increased expression of NF-κB
in dysplasia and subsequent decrease in carcinoma could be a
consequence, rather than the cause, of transformation.
According to Sabel et al(6), tumor control depends as much on the
magnitude of the initial immune response as the capacity to sustain
this response for a prolonged period. In reference to the cases of
dysplasia, the present study corroborates this. This strengthens
the notion of flexibility regarding the role of inflammation in
oral carcinogenesis. This is contrary to the protective role of
inflammation used in systems for the histological grading of
malignancy proposed by Jakobsson et al(21) and Bryne et al(22), since the >5% expression of CD8 in
16 (80%) of the 20 cases of OED occurred in only 12 (30%) of the 40
cases of OSCC, with a significant correlation with the intensity of
the inflammatory infiltrate.
The inverse correlation between the intensity of the
inflammatory infiltrate and epithelial TNF-α in the cases of
carcinoma may be responsible for the reduction in NF-κB in
epithelial cells following transformation, thereby suggesting a
role in this process. On the other hand, the positive correlation
between stromal TNF-α and inflammatory infiltrate, which was more
intense in the cases of OSCC, suggests a participation in tumor
progression. These findings are in disagreement with the
possibility of an activated form of NF-κB being induced by various
inflammatory stimuli and regulating the gene products (5,23), as
this occurred in the cases of dysplasia and was therefore involved
in cell transformation. However, these findings are in agreement
with the fact that this occurrence is an important link between
cancer and inflammation, which may be initiated by the
overregulation of TNF-α (24).
In addition, the correlation of TNF-α to the
intensity of the inflammatory infiltrate in dysplasia and
carcinoma, even while exercising different roles, is in agreement
with the findings described by Aggarwal et al(25), who suggested that, as one of the
major chemical mediators of inflammation, TNF-α is involved in
diverse steps of tumorigenesis, including the transformation
process.
In normal tissue, TGF-β regulates cell growth and
differentiation and functions as a tumor suppressor during the
onset of carcinogenesis. In the present study, TGF-β was expressed
in a moderate to intense degree in 80% of the cases of OED and in
only 60% of the cases of OSCC. However, between the degrees of OED,
there was a 50% reduction among the intense cases compared with the
mild and moderate cases, all of which had >5% labeling. These
findings are in agreement with those described by Glick et
al(12), who demonstrated the
occurrence of carcinomatous transformation in keratinocytes
following the autocrine reduction in TGF-β.
According to Donalisio et al(13), transformed cells are either
partially or totally resistant to the inhibitory effect of TGF-β,
which may be related to the degree of cell differentiation.
According to Gorelik and Flavell (26), however, in order to favor the
antitumor CD8 response, TGF-β must be blocked before the tumor
cells partially or totally inhibit this response. It may therefore
be considered that, depending on the risk factor, the amount of
TGF-β produced after transformation may partially or totally
inhibit this antitumor response, leading to the development of a
less or more aggressive OSCC, respectively.
In the inflammatory infiltrate, stromal TGF-β was
expressed in a moderate to intense degree in 80% of the cases of
OED and 82.5% of the cases of OSCC and appears to participate in
this process by inhibiting the protective function of CD8, which is
in agreement with the findings described by Gorelik and Flavell
(26). Thus, TGF-β becomes
oncogenic, promoting tumor progression and invasion (14,15).
Sato et al(10) report having found a favorable
prognosis in cases of ovarian cancer in which the CD8/Treg cell
ratio was high. Based on the fact that Treg cells maintained a
regular pattern in the cases of dysplasia and carcinoma, with CD8
being more expressed in cases of dysplasia, the results agree with
the findings of this previous study and also suggest that a
reduction in this ratio favors malignant transformation.
The general context of the present study is in
agreement with Weitzman and Gordon (27), who associated a number of chronic
inflammatory processes with the development of cancer, as well as
Balkwill and Mantovani (28), who
suggested the participation of cytokines and inflammatory cells in
tumor development and progression. Moreover, the findings are in
agreement with Abbas et al(19), who report that transformed cells
have the ability to evade or overcome the defense mechanisms of the
host.
For prognostic evaluation it is necessary to
associate a system for the histological grading of malignancy with
immunohistochemical analysis to assess both the risk of malignant
transformation of dysplasia and tumor aggressiveness. The results
of the present study suggest that CD8, TGF-β and TNF-α should be
included in this analysis. Further studies with a larger sample
size should be carried out in order to confirm the participation of
these and other inflammatory cytokines in carcinogenesis and the
possibility of their use in antitumor therapy.
In summary, it was concluded that the antitumor
reaction exerted by CD8 T-lymphocytes occurs with greater frequency
in cases of OED, suggesting a slow down of the transformation and
invasion process when associated with a high rate of CD8. The
presence of inflammatory infiltrate in cases of OED favors the
transformation and invasion process when stromal TNF-α and NF-κB
are overexpressed, as NF-κB activated by TNF-α during inflammation
predisposes the lesion to transformation, functioning as a link
between inflammation and cancer. Although intense inflammatory
infiltrate has a positive relation with CD8 in cases of OSCC, the
antitumor defense function is minimal, as only ∼30% of cases of
carcinoma exhibit >5% labeling. TNF-α, which has a positive
correlation in the stroma and a negative correlation in the
epithelium when associated to the intensity of the inflammatory
infiltrate in cases of OSCC, appears to favor tumor progression
following transformation. Transformed keratinocytes either
partially or totally lose control of the growth exercised by TGF-β,
which becomes oncogenic.
References
|
1
|
Coussens LM and Werb Z: Inflammatory cells
and cancer: think different! J Exp Med. 193:23–26. 2001.
|
|
2
|
Yan L, Zucker S and Toole BP: Roles of the
multifunctional glycoprotein, emmprin (basigin; CD 147), in tumour
progression. Thromb Haemost. 93:199–204. 2005.PubMed/NCBI
|
|
3
|
Sheu BC, Hsu SM, Ho HN, Lin RH, Torng PL
and Huang SC: Reversed CD4/CD8 ratios of tumor-infiltrating
lymphocytes are correlated with the progression of human cervical
carcinoma. Cancer. 86:1537–1543. 1999. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Hayden MS and Ghosh S: Signaling to
NF-kappa B. Genes Dev. 18:2195–2224. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Pacifico F and Leonardi A: NF-kB in solid
tumors. Biochem Pharmacol. 72:1142–1152. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Sabel MS, Hess SD, Egilmez NK, Conway TF
Jr, Chen FA and Bankert RB: CTLA-4 blockade augments human T
lymphocyte-mediated suppression of lung tumor xenografts in SCID
mice. Cancer Immunol Immunother. 54:944–952. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Hori S, Namura T and Sakaguchi S: Control
of regulatory T cell development by the transcription factor Foxp3.
Science. 299:1057–1061. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Maggi E, Cosmi L, Liotta F, Romagnani P,
Romagnani S and Annunziato F: Thymic regulatory T cells. Autoimmun
Rev. 4:579–586. 2005. View Article : Google Scholar
|
|
9
|
Sakaguchi S: Naturally arising CD4+
regulatory cells for immunologic self-tolerance and negative
control of immune responses. Annu Rev Immunol. 22:531–562.
2004.
|
|
10
|
Sato E, Olson SH, Ahn J, Bundy B,
Nishikawa H, Qian F, et al: Intraepithelial CD8+ tumor-infiltrating
lymphocytes and a high CD8+/regulatory T cell ratio are associated
with favorable prognosis in ovarian cancer. Proc Natl Acad Sci USA.
102:18538–18543. 2005.
|
|
11
|
de Boer OJ, van der Loos CM, Teeling P,
van der Wal AC and Teunissen MB: Immunohistochemical analysis of
regulatory T cell markers FOXP3 and GITR on CD4+CD25+ T cells in
normal skin and inflammatory dermatoses. J Histochem Cytochem.
55:891–898. 2007.PubMed/NCBI
|
|
12
|
Glick AB, Lee MM, Darwiche N, Kulkarni AB,
Karlsson S and Yuspa SH: Targeted deletion of the TGF-beta 1 gene
causes rapid progression to squamous cell carcinoma. Genes Dev.
8:2429–2440. 1994. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Donalisio M, Cornaglia M, Landolfo S and
Lembo D: TGF-β1 and IL-4 downregulate human papillomavirus-16
oncogene expression but have differential effects on the malignant
phenotype of cervical carcinoma cells. Virus Res. 132:253–256.
2008.
|
|
14
|
Massagué J, Blain SW and Lo RS: TGF-beta
signaling in growth control, cancer, and heritable disorders. Cell.
103:295–309. 2000.PubMed/NCBI
|
|
15
|
Moustakas A, Pardali K, Gaal A and Heldin
CH: Mechanisms of TGF-β signaling in regulation of cell growth and
differentiation. Immunol Lett. 82:85–91. 2002.
|
|
16
|
Derynck R, Akhurst RJ and Balmain A:
TGF-beta signaling in tumor suppression. Nat Genet. 29:117–129.
2001. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Warnakulasuriya S, Reibel J, Bouquot J and
Dabelsteen E: Oral epithelial dysplasia classification systems:
predictive value, utility, weaknesses and scope for improvement. J
Oral Pathol Med. 37:127–133. 2008. View Article : Google Scholar
|
|
18
|
Piva MR, De Souza LB, Martins-Filho PR,
Soares RC, De Santana Santos T and De Souza Andrade ES: Role of
inflammation in oral carcinogenesis (Part I): Histological grading
of malignancy using a binary system. Oncol Lett. 2:1225–1231.
2011.PubMed/NCBI
|
|
19
|
Abbas NF, Labib El-Sharkawy S, Abbas EA
and Abdel Monem El-Shaer M: Immunohistochemical study of p53 and
angiogenesis in benign and preneoplastic oral lesions and oral
squamous cell carcinoma. Oral Surg Oral Med Oral Pathol Oral Radiol
Oral Endod. 103:385–390. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Lind MH, Rozell B, Wallin RP, van
Hogerlinden M, Ljunggren HG, Toftgård R and Sur I: Tumor necrosis
factor receptor 1-mediated signaling is required for skin cancer
development induced by NF-kappaB inhibition. Proc Natl Acad Sci
USA. 101:4972–4977. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Jakobsson PA, Eneroth GM, Killander D,
Moberger G and Mårtensson B: Histologic classification and grading
of malignancy in carcinoma of the larynx (a pilot study). Acta
Radiol Ther Phys Biol. 12:1–8. 1973. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Bryne M, Koppang HS, Lilleng R, Stene T,
Bang G and Dabelsteen E: New malignancy grading is a better
prognostic indicator than Broders’ grading in oral squamous cell
carcinomas. J Oral Pathol Med. 18:432–437. 1989.PubMed/NCBI
|
|
23
|
Aggarwal BB: Nuclear factor-kappaB: the
enemy within. Cancer Cell. 6:203–208. 2004.PubMed/NCBI
|
|
24
|
Pikarsky E, Porat RM, Stein I, Abramovitch
R, Amit S, Kasem S, et al: NF-kappaB functions as a tumour promoter
in inflammation-associated cancer. Nature. 341:461–466. 2004.
View Article : Google Scholar
|
|
25
|
Aggarwal BB, Shishodia S, Sandur SK,
Pandey MK and Sethi G: Inflammation and cancer: How hot is the
link? Biochem Pharmacol. 72:1605–1621. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Gorelik L and Flavell RA: Immune-mediated
eradication of tumors througth the blockade of transforming growth
factor-β signaling in T cells. Nature Med. 7:1118–1122.
2011.PubMed/NCBI
|
|
27
|
Weitzman SA and Gordon LI: Inflammation
and cancer: Role of phagocyte-generated oxidants in carcinogenesis.
Blood. 76:655–663. 1990.PubMed/NCBI
|
|
28
|
Balkwill F and Mantovani A: Inflammation
and cancer: back to Virchow? Lancet. 85:473–483. 2001.
|