Introduction
Non-keratinizing, undifferentiated nasopharyngeal
carcinoma (NPC; WHO type III) is the most common subtype of NPC and
is particularly common in Asia (1).
The Epstein-Barr virus has been implicated in the pathogenesis of
this subtype and while its presence does not currently guide
standard therapy, it may assist in establishing a correct diagnosis
(2,3). The majority of cases present with
localized disease and although local therapy may be curative, the
potential for developing distant metastases is high. The most
commonly described sites of metastasis are the lymph nodes, bones,
lungs and liver (4). The breast is
an uncommon site of metastasis in NPC and represents a diagnostic
challenge due to the radiographical similarities to primary breast
cancer, a considerably more common cancer. There have been four
previously reported cases of NPC with metastasis to the breast
(5–7). The present case study reports a fifth
case and describes the Epstein-Barr virus testing procedure used to
confirm the diagnosis. Informed consent was obatined from the
patient.
Case report
Clinical presentation
A 49-year-old Vietnamese female was diagnosed with a
stage III, WHO type III, NPC upon presentation with diffuse
headaches. The patient was treated with curative intent, receiving
6 weeks of definitive radiation and concurrent bolus cisplatin at a
dose of 100 mg/m2 for 3 doses followed by 3 cycles of
adjuvant cisplatin 100 mg/m2 and 5-fluorouracil 1000
mg/m2/day for 4 days. The patient exhibited a complete
response and was disease-free for 18 months, at which point lower
back pain developed. Radiographical assessment identified diffuse
blastic bone lesions and a biopsy confirmed relapsed metastatic
NPC.
Treatment and clinical course
Following the administration of palliative radiation
to a painful sacral lesion, the patient began systemic therapy with
weekly paclitaxel 80 mg/m2 and cetuximab 250
mg/m2, but experienced progression after 6 months.
Following this, second line gemcitabine was administered at a dose
of 1000 mg/m2 on days 1, 8 and 15 in a 4-week cycle and
disease control was maintained for 8 months. The patient initially
received zoledronic acid with chemotherapy, however, this was later
changed to denosumab. Subsequent radiographical procedures then
identified progression of the disease with the development of new
axillary and iliac adenopathy. A third line therapy using weekly
methotrexate (1 mg/kg) was administered; however, progression
occurred at 3 months. The patient was then treated in a phase I
clinical trial at our institution with the MEK inhibitor GDC-0623
designed to determine the maximal tolerated dose; the disease was
controlled for 4 months. Following this, the patient developed a
new, palpable, painless mass in the left breast.
Diagnosis of cancer
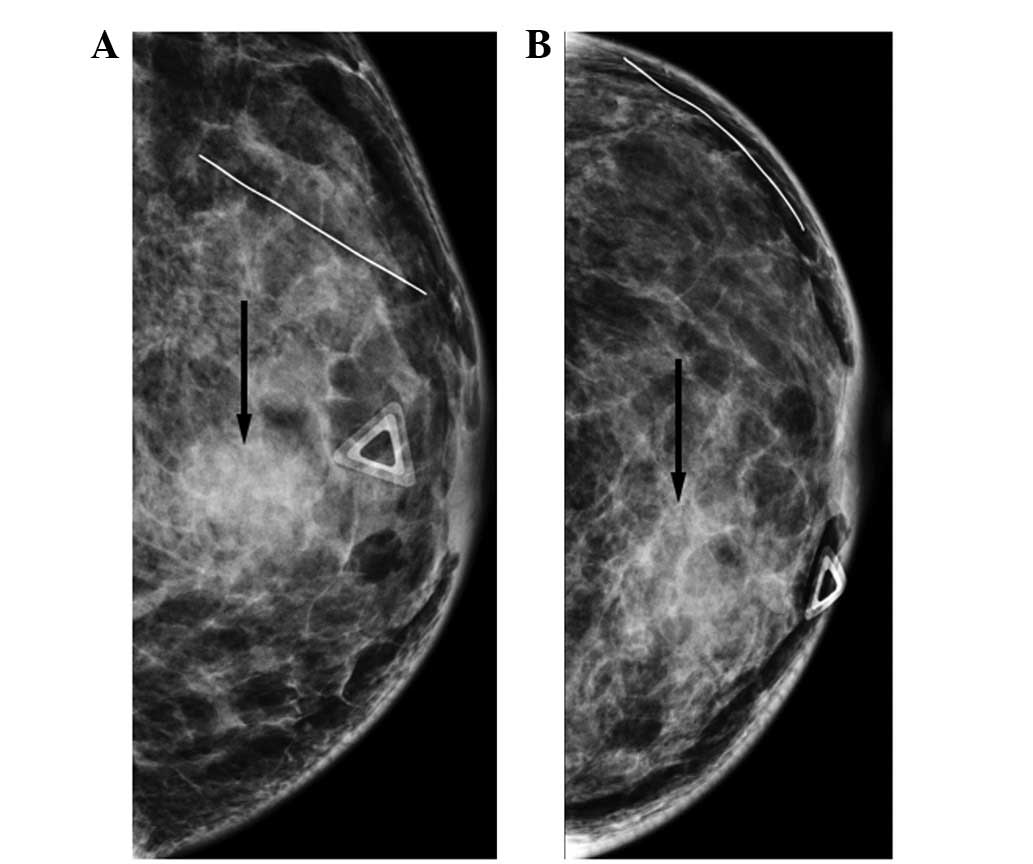
Mammography identified a 5×4.4×1.9-cm irregular mass
at the 10 o’clock position of the left breast, BI-RADS category 5
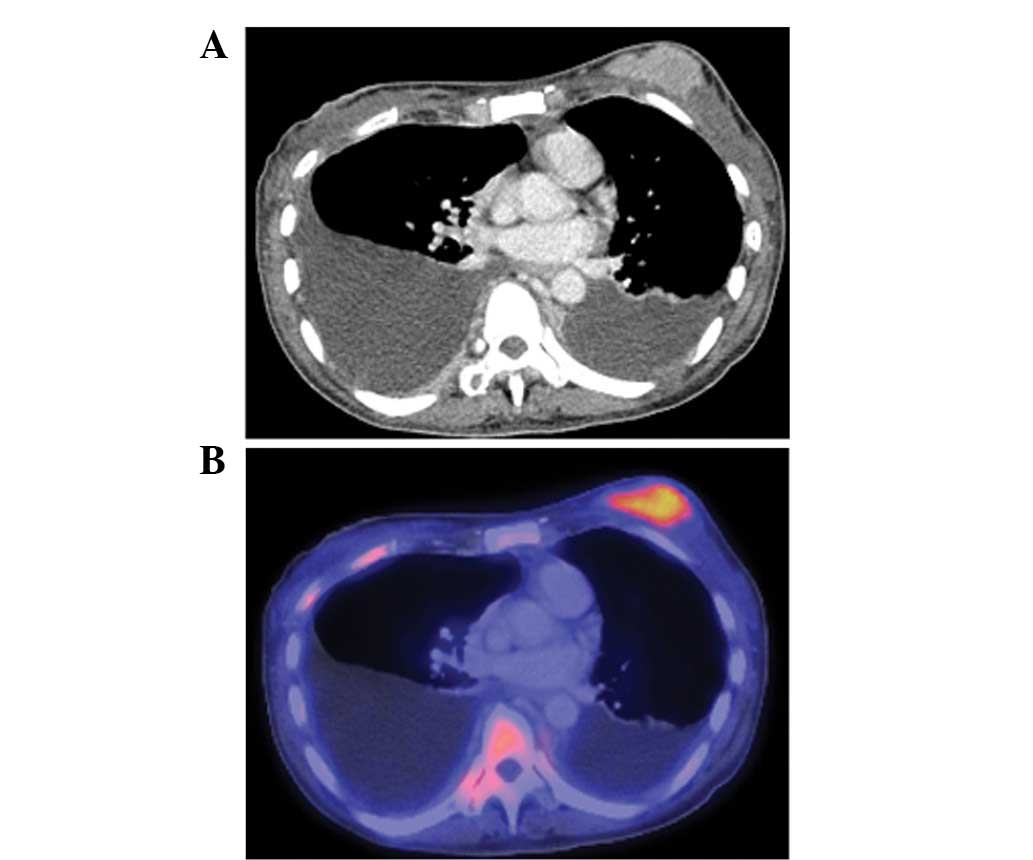
(Fig. 1). Positron emission
tomography-computed tomography (PET-CT) imaging also identified the
new left breast mass (Fig. 2),
which was radiographically suggestive of a primary breast
carcinoma. The other sites of NPC were unchanged from the prior
examinations. An ultrasound-guided biopsy was performed and the
analysis revealed malignant cells consistent with a primary breast
cancer. Immunohistochemistry revealed no estrogen or progesterone
receptor expression and there was no amplification of HER2
expression. The patient received a presumptive diagnosis of a
concurrent and separate primary breast carcinoma.
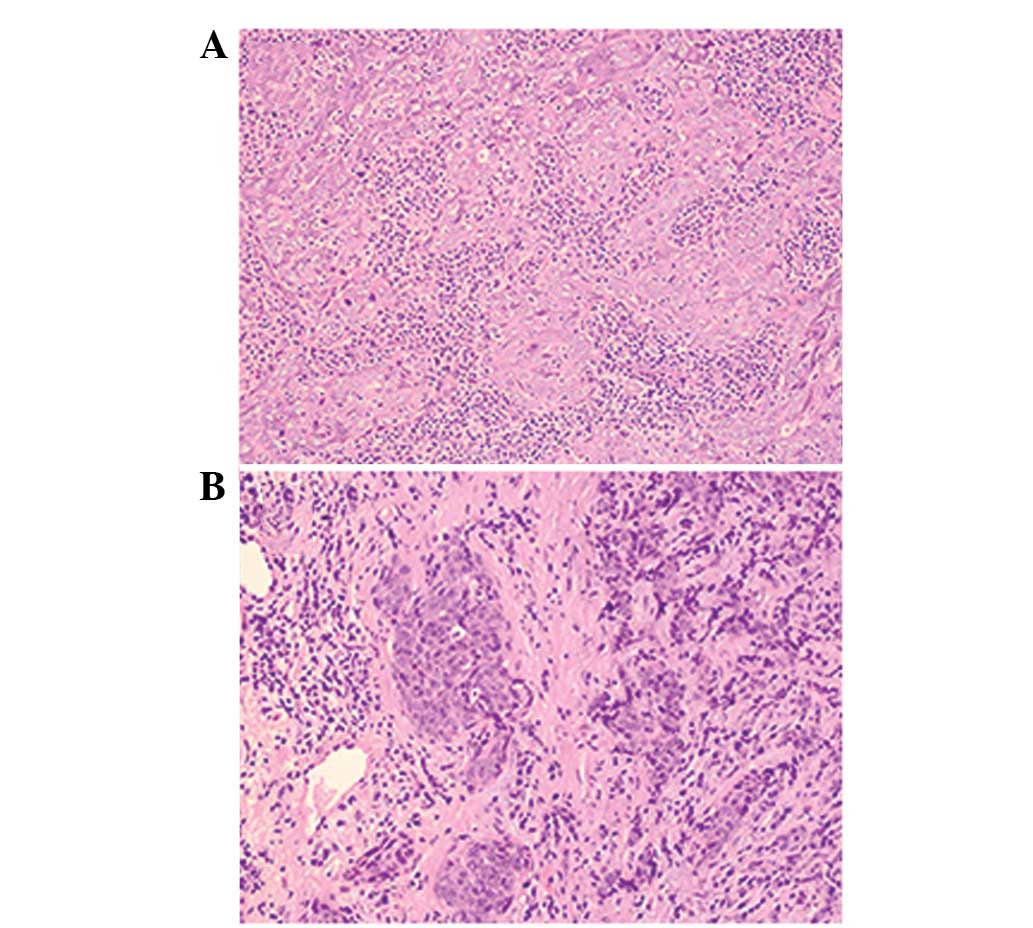
Histological analysis
All biopsy specimens were obtained for direct
comparison. Following close review, all samples exhibited a similar
histological appearance (Fig. 3).
Epstein-Barr virus testing was performed by in situ
hybridization. Slides were incubated, deparaffinized, blocked with
3% hydrogen peroxide, digested, dehydrated and incubated in a
prehybridization solution. Slides were then incubated with
ribo-probes for EBER1 (8). The
primary tumor and the breast mass were Epstein-Barr virus-positive.
The diagnosis was changed to progressive NPC metastatic to the
breast and the treatment was terminated. At the time of this
report, the patient was doing well and beginning fifth line
chemotherapy.
Discussion
Metastasis to the breast from an extra-mammary
primary tumor is uncommon, accounting for <2% of tumors
identified in the breast (7,9). This
holds true for NPC. While distant metastases from NPC are common,
only 4 cases of metastasis to the breast have been described
(Table I). The potential for
misdiagnosis and confusion is high, as primary breast cancer is far
more common than NPC and the radiographical appearance of these
lesions is often extremely similar (10). Although a biopsy is used to
establish the diagnosis, nasopharyngeal biopsies often provide
scant tissue for comparison and these two epithelial tumors share a
number of histological characteristics. As the treatment for these
two types of cancer is vastly different, it is critically important
to establish the correct diagnosis.
 | Table ISummary of cases of NPC metastasis to
the breast. |
Table I
Summary of cases of NPC metastasis to
the breast.
| First author
(Ref.) | Year | Age (years) | Initial therapy | Time to relapse
(months) | Time to breast
metastasis (months) | Survival following
diagnosis (months) |
|---|
| Sham et
al(5) | 1986 | 39 | Radiation | 17 | 30 | 33 |
| Sham et
al(5) | 1987 | 51 | Radiation | 27 | 30 | N/R |
| Driss et
al(6) | 1999 | 25 | Chemotherapy | 42 | 42 | N/R |
| Yeh et
al(7) | 2004 | 46 | Chemotherapy +
radiation | N/R | N/R | N/R |
| Leach et
ala | 2009 | 49 | Chemotherapy +
radiation | 18 | 39 | N/R |
Epstein-Barr virus is markedly associated with the
development of WHO type III NPC and a number of diagnostic
modalities have been developed to facilitate the detection of the
virus. These include in situ hybridization and polymerase
chain reaction (11,12). The presence of the Epstein-Barr
virus is not necessary to establish a diagnosis of NPC, however, it
may be extremely useful for cases where the diagnosis is unclear.
In the present case, the detection of the Epstein-Barr virus in the
breast mass confirmed the diagnosis of metastatic NPC and
facilitated the correct treatment decisions.
Only four cases of breast metastasis from NPC have
been previously reported. All four cases described a solitary
breast mass that developed following a diagnosis of metastatic NPC.
The first patient received an initial radiation treatment to the
primary NPC, then developed bone and lung metastases (5). The patient received cyclophosphamide
as a salvage therapy, but developed a breast mass with axillary
lymphadenopathy. The biopsy was consistent with NPC, and in light
of progression, the treatment was changed to cisplatin plus
5-fluorouracil. The patient succumbed to cancer several months
later. The second patient also received initial radiation treatment
to the nasopharynx and then developed lung metastases (5). Salvage therapy with mitoxantrone was
initiated when the patient developed a breast mass with axillary
adenopathy. Again, the histological examination was indicative of
NPC and the treatment was changed to cisplatin plus 5-fluorouracil.
The third patient was treated with systemic chemotherapy for the
initial diagnosis of NPC. The individual then presented with
bilateral breast masses and pathological lymphadenopathy in the
supraclavicular and axillary stations three and a half years later.
A diagnosis of metastatic disease was confirmed via biopsy and
negative staining for the estrogen and progesterone receptors. In
addition, in situ hybridization using an Epstein-Barr virus
encoded RNA probe was markedly and diffusely positive (6). The fourth patient developed a breast
metastasis following the initial diagnosis of NPC, but no details
of the treatment were reported (7).
These cases stress the importance of the clinical
correlation with biopsy specimens. In the case presented, the
breast mass that emerged during therapy was the only sign of
disease progression and the confirmatory Epstein-Barr virus testing
helped to confirm treatment failure. The radiographical and
histological characteristics of breast metastasis from NPC are
extremely similar to those of primary breast carcinoma. The
clinical context of concurrent or remote NPC may guide the
pathologist to consider the diagnosis of this rare diagnosis. In
cases of WHO type III NPC, positive Epstein-Barr virus testing
provides confirmatory evidence for the diagnosis and direct
treatment strategies. As with localized NPC, a multidisciplinary
approach is always beneficial to the patient.
References
|
1
|
Dickens P, Srivastava G, Loke SL, Chan CW
and Liu YT: Epstein-Barr virus DNA in nasopharyngeal carcinomas
from Chinese patients in Hong Kong. J Clin Pathol. 45:396–397.
1992. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Wei WI and Sham JS: Nasopharyngeal
carcinoma. Lancet. 365:2041–2054. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Raab-Traub N: Epstein-Barr virus in the
pathogenesis of NPC. Semin Cancer Biol. 12:431–441. 2002.
View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Ahmad A and Stefani S: Distant metastases
of nasopharyngeal carcinoma: a study of 256 male patients. J Surg
Oncol. 33:194–197. 1986. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Sham JS and Choy D: Breast metastasis from
nasopharyngeal carcinoma. Eur J Surg Oncol. 17:91–93. 1991.
|
|
6
|
Driss M, Abid L, Mrad K, Dhouib R, Charfi
L, Bouzaein A and Ben Romdhane K: Breast metastases from
undifferentiated nasopharyngeal carcinoma. Pathologica. 99:428–430.
2007.PubMed/NCBI
|
|
7
|
Yeh CN, Lin CH and Chen MF: Clinical and
ultrasonographic characteristics of breast metastases from
extramammary malignancies. Am Surg. 70:287–290. 2004.PubMed/NCBI
|
|
8
|
Elgui de Oliveira D, Furtado Monteiro TA,
Alencar de Melo W, Amaral Rebouças Moreira M, Alvarenga M and
Bacchi CE: Lack of Epstein-Barr virus infection in cervical
carcinomas. Arch Pathol Lab Med. 123:1098–1100. 1999.PubMed/NCBI
|
|
9
|
Amichetti M, Perani B and Boi S:
Metastases to the breast from extramammary malignancies. Oncology.
47:257–260. 1990. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Shahrokni A, Rajebi MR and Saif MW: Breast
metastasis of small bowel carcinoid tumor misdiagnosed as primary
breast cancer. Ann Saudi Med. 29:320–321. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Lee WY, Hsiao JR, Jin YT and Tsai ST:
Epstein-Barr virus detection in neck metastases by in-situ
hybridization in fine-needle aspiration cytologic studies: an aid
for differentiating the primary site. Head Neck. 22:336–340. 2000.
View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Tsai ST, Jin YT and Su IJ: Expression of
EBER1 in primary and metastatic nasopharyngeal carcinoma tissues
using in situ hybridization. A correlation with WHO histologic
subtypes. Cancer. 77:231–236. 1996. View Article : Google Scholar : PubMed/NCBI
|