Introduction
Osteosarcoma is the most common primary malignant
bone tumor. Although the clinical outcome has significantly
improved with the application of neoadjuvant chemotherapy, the
recurrence of osteosarcoma remains a common post-operative
complication, often resulting in treatment failure. It is generally
recognized that the post-operative recurrence of osteosarcoma may
occur within two years post-surgery, with the possibility of
recurrence decreasing gradually with the prolongation of the
follow-up time. However, although it is extremely rare, a
recurrence may also occur five years subsequent to the treatment
(1), which is defined as a late
recurrence of osteosarcoma. The present study retrospectively
analyzed three patients with late recurrent osteosarcomas who were
treated at the General Hospital of Jinan Military Command, General
Hospital of Nanjing Military Command and Xinan Hospital of The
Third Military Medical University (Chongqing, China). Furthermore,
10 similar cases from the literature were comprehensively reviewed
in order to determine the correct diagnosis and treatment for this
disease. This study was approved by the ethics committee of the
General Hospital of Jinan Military Command. Written informed
consent was obtained from all patients.
Case reports
Case 1
A six-year-old female was admitted to the General
Hospital of Jinan Military Command on June 9, 2005 due to right
knee pain that had lasted for one and a half months, with no
significant pain at night. A physical examination revealed a 6×4-cm
mass in the medial-posterior side of the right distal femur, with
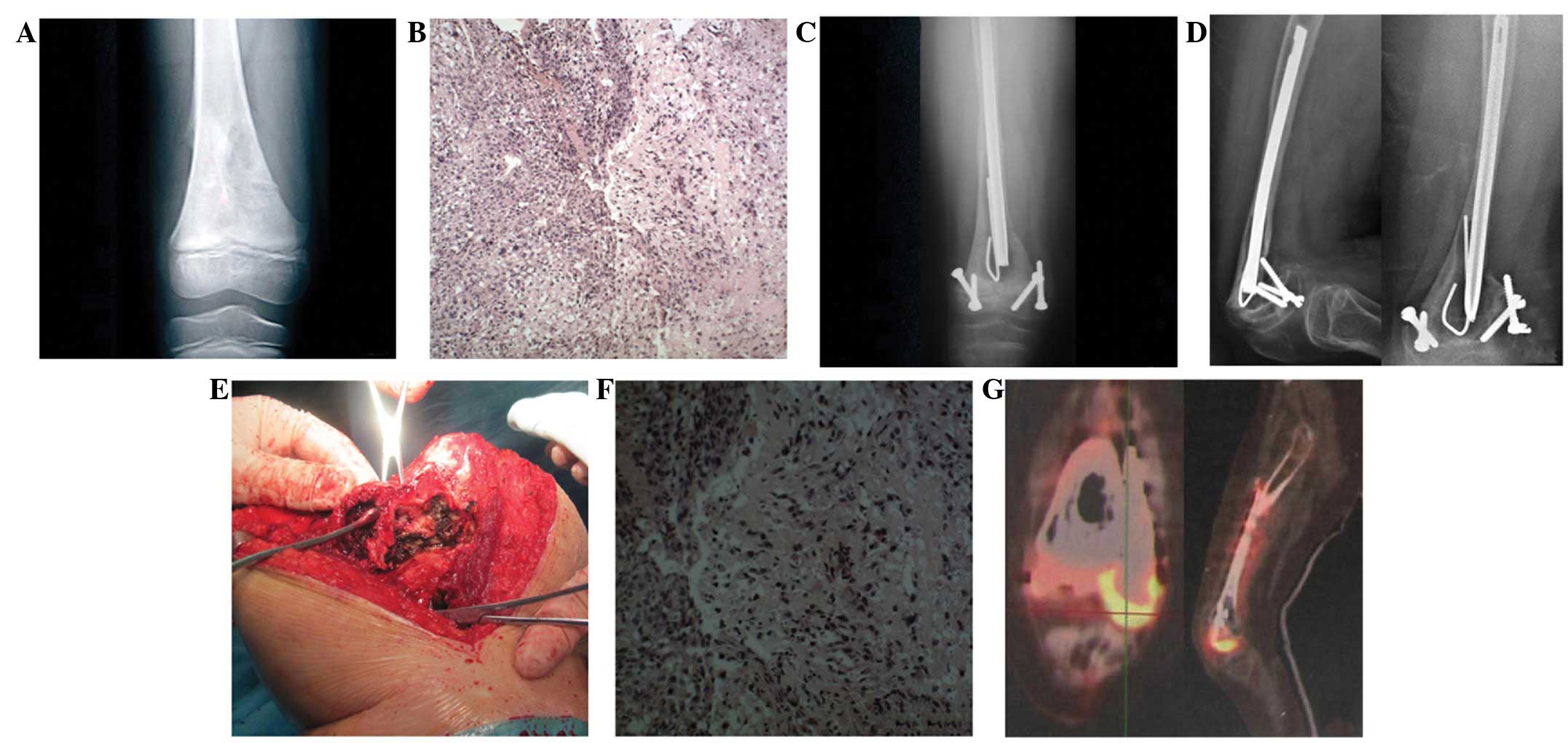
obvious tenderness to the area and a poorly-defined border. X-ray
imaging (Fig. 1A) revealed a mixed
osteolytic-osteoblastic lesion with a periosteal reaction of the
right distal femur and a shadow of a soft tissue mass. MRI showed a
mixed high and low signal intensity lesion in the right distal
femur, with evidence of a soft tissue mass, but no tumor invasion
of the epiphysis. A needle aspiration biopsy was performed and a
histological examination of the specimen confirmed the diagnosis of
osteosarcoma (Fig. 1B). The patient
then received two courses of pre-operative DIA chemotherapy
[doxorubicin (ADR), 30 mg/m2 × 3; ifosfamide (IFO), 2
g/m2 × 5; and cisplatin (DDP), 120 mg/m2].
The patient’s pain symptoms disappeared following chemotherapy. The
X-ray examination showed osteolytic damage to the right distal
femur with a clear boundary. A tumor bone calcification shadow was
visible in the medullary cavity, but the surrounding soft tissue
mass had disappeared. MRI showed a significantly reduced lesion in
the right distal femur and an evident disappearance of the soft
tissue swelling, without tumor invasion of the epiphysis. On
September 1, 2005, under epidural anesthesia, the patient underwent
an en bloc resection of the tumor and an inactivated bone
replantation with preservation of the epiphysis. The incision
healed and no complications occurred. A post-operative histological
examination of the specimen confirmed the evident degeneration and
necrosis of the osteosarcoma cells. Post-operative chemotherapy was
begun at two weeks post-surgery, with the same regimen as the
pre-operative chemotherapy, and lasted for six courses with
three-week intervals. A post-operative X-ray following six months
of treatment showed good healing between the inactivated and host
bones (Fig. 1C), and the knee was
able to achieve 90 degrees of flexion. However, at two years
post-surgery, the affected limb began to shorten, which gradually
limited the knees function. On February 22, 2012, 6.5 years after
the initial surgery, the patient was readmitted into hospital due
to one week of pain in the affected knee. The patient was unable to
walk due to a goose-shaped deformity of the right knee. While there
was no obvious tenderness to the area, the patient was unable to
straighten the affected knee. The affected limb was 7 cm shorter
than the contralateral one. An X-ray examination confirmed good
healing between the inactivated bone and the femoral shaft
(Fig. 1D). However, the diameter of
the affected femur was thinner than that of the contralateral one
and bone fragmentation was observed at the healing site, connecting
the inactivated bone and the preserved epiphysis, which formed a
forward protrusion. Emission computed tomography (ECT) and lung CT
scans showed no abnormalities. The patient was then diagnosed with
a nonunion following inactivated bone replantation with
preservation of the epiphysis for osteosarcoma of the right distal
femur. On March 4, 2012, an en bloc resection of the inactivated
tumor bone and an allograft bone transplantation were performed
under general anesthesia. Granulation-like tissue was observed
intraoperatively in the medial femoral condyle. This was considered
to be a reaction of the surrounding bones to the screw and was
subsequently removed completely (Fig.
1E). However, a post-operative pathological examination of the
specimen indicated that the curetted tissue was that of
osteosarcoma (Fig. 1F), with the
same histology as the specimen from the initial diagnosis. On March
15, 2012, a positron emission tomography (PET)/CT examination
showed abnormal bone metabolism at the right distal femoral condyle
(Fig. 1G), which was diagnosed as a
recurrence of the osteosarcoma of the right distal femur. On March
23, 2012, under general anesthesia, the entire right knee joint was
removed due to osteosarcoma at the femoral condyle and an
inactivated allograft bone replantation and arthrodesis were
performed. The incision stitches were removed at 14 days
post-surgery and the wound healed well. Chemotherapy was initiated
two weeks after the surgery, using the original regimen, and
stopped following two courses of treatment due to the occurrence of
cardiac hypertrophy. There was no recurrence or metastasis within a
follow-up period of 8 months.
Case 2
A 25-year-old male was admitted to the General
Hospital of Nanjing Military Command on June 15, 2000, due to a
gradually increasing, severe pain in the left knee that had lasted
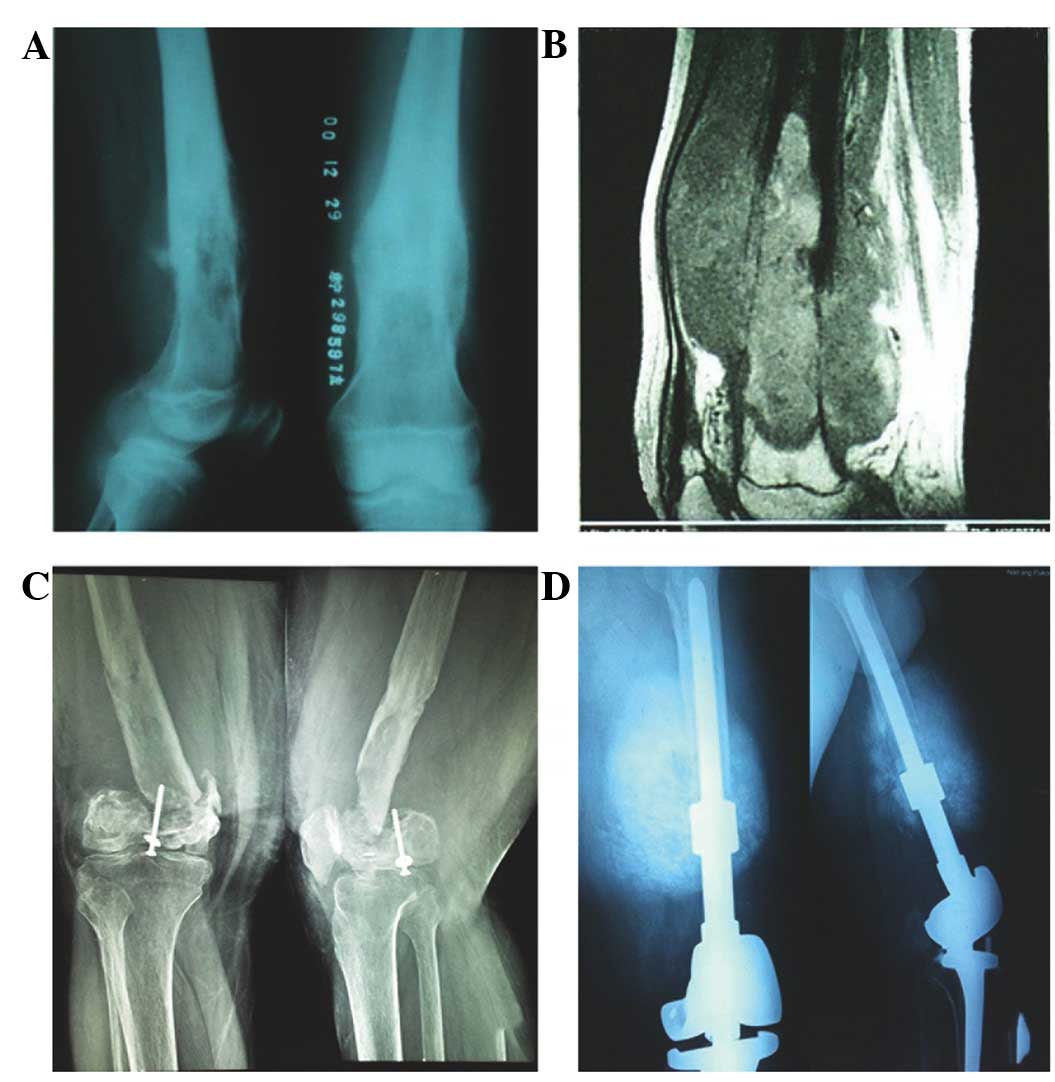
for one month. X-ray imaging (Fig.
2A) showed osteoblastic destruction of the left distal femur,
partial osteolytic changes, a visible periosteal reaction and a
soft tissue mass. MRI (Fig. 2B)
showed a mixed high and low signal intensity in the left distal
femur, which formed a large soft tissue mass. The patient was
finally diagnosed with osteosarcoma of the left distal femur by
biopsy and was administered two courses of high-dose methotrexate
(HDMTX) and one course of ADR and DDP at the same dosage as
previously reported (HDMTX, 10 g/m2; ADR, 60
mg/m2; and DDP, 120 mg/m2) (2). On August 16, 2000, the patient
received an en bloc resection of the left distal femoral
osteosarcoma and an allograft bone transplantation. The incision
healed well. The same regimen as used in the pre-operative
chemotherapy was applied post-operatively. One year after the
surgery, the patient’s left knee was able to achieve 90 degrees of
flexion. However, at six years post-surgery, the patient felt pain
in the affected limb, which was now shortened and causing a limp.
At eight years post-surgery, the patient had difficulty walking,
felt exacerbated pain and the affected limb was shortened by 12 cm.
A diagnosis of bone resorption following allograft bone
transplantation was determined (Fig.
2C). In December 2009, the patient underwent a resection of the
allograft bone and a reconstruction using a tumor prosthesis. Three
months after the second surgery, the affected knee was able to
achieve 45 degrees of flexion. In August 2010, X-ray imaging
revealed a tumor shadow between the prosthesis and the host bone in
the middle of the right femur, which was gradually increasing in
size (Fig. 2D). In August 2011, the
affected leg was amputated and the osteosarcoma was confirmed by a
post-operative pathological examination. The patient was then
provided with four courses of chemotherapy consisting of ADR, DDP
and IFO (identical doses to previously). There were no recurrences
or distant metastases within 10 months following the third surgery.
The patient is currently being monitored using follow-up
appointments.
Case 3
A 12-year-old female was admitted to Xinan Hospital
of The Third Military Medical University on January 24, 2007 due to
two months of intermittent lower left leg pain, which became
aggravated in the second month and was accompanied by the growth of
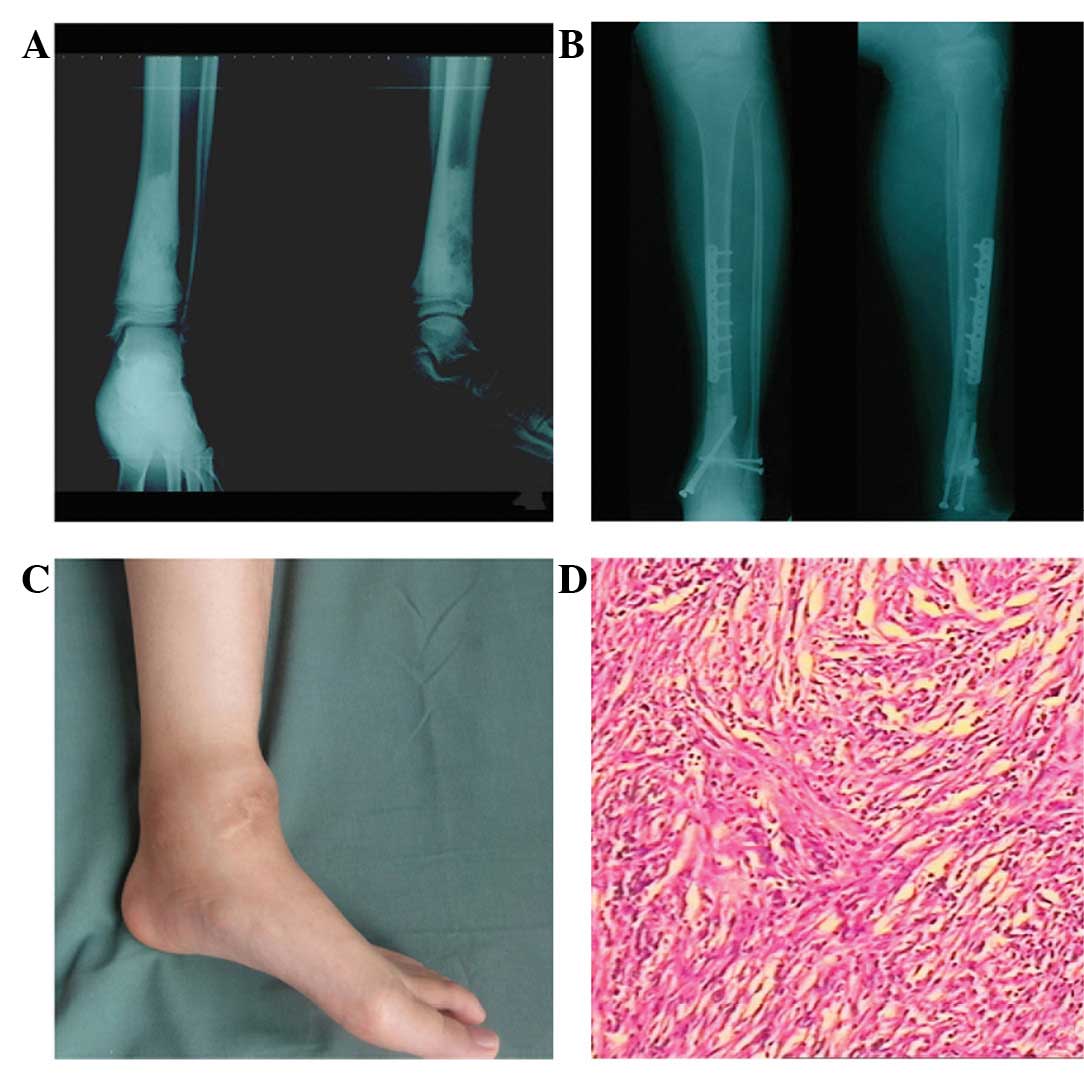
a mass. X-ray imaging showed osteoblastic bone destruction of the
left distal tibia (Fig. 3A). MRI
showed a mixed high and low signal intensity, with a visible
periosteal reaction and an anterior soft tissue swelling. The
patient was diagnosed with osteosarcoma of the distal left tibia by
biopsy. The symptoms disappeared following one course of AP (ADR,
60 mg/m2; and DDP, 120 mg/m2) regimen
chemotherapy. On March 2, 2007, the patient underwent a sectional
removal of the osteosarcoma of the left distal tibia, a
reconstruction using inactivated bone and an internal fixation,
under general anesthesia. The post-operative pathological
examination confirmed the initial diagnosis of osteosarcoma.
Chemotherapy with the AP regimen (four courses with three week
intervals) was initiated subsequent to the healing of the incision
(two weeks post-surgery). An X-ray captured at 29 months
post-surgery showed a nonunion between the host bone and the distal
side of the inactivated bone, accompanied by a posterior protrusion
and varus deformity (Fig. 3B). On
July 31, 2009, the stainless steel plate-screw fixation was
surgically removed from the left tibia. On April 4, 2012, 62 months
after the initial surgery, the patient was hospitalized due to one
month of ankle pain, which was associated with a mass (Fig. 3C). An X-ray examination demonstrated
healing between the host bone and the proximal end of the
inactivated bone, but a hypertrophic nonunion existed between the
host bone and the distal end of the inactivated bone, which was
accompanied by a posterior protrusion and varus deformity. Screw
residues were left in the inferior tibia and fibula. MRI showed an
anterior soft tissue mass in the lower left leg and osteolytic
destruction of the left distal tibia, surrounded by edema. ECT
showed an abnormal concentration of radionuclides in the left
distal tibia, but no obvious abnormalities in the rest of the
skeletal system. The patient was diagnosed with a recurrence of
osteosarcoma of the left tibia. On May 4, 2012, an amputation of
the middle section of the lower left leg was performed under
epidural anesthesia. A post-operative pathological examination
confirmed the pre-operative diagnosis of fibroblastic osteosarcoma
(Fig. 3D). The incision stitches
were removed at 14 days post-surgery, and the wound healed first
time. There was no recurrence or metastasis at 6 months
post-surgery. The patient is currently being monitored by follow-up
appointments.
Discussion
With the clinical application of neoadjuvant
chemotherapy and the technical improvements in limb salvage
surgery, the tumor-free survival rate of osteosarcoma has
significantly improved. However, recurrence and metastasis occur in
1/3 of the affected patients and the treatment of these patients
remains a challenge. According to a study by Spiegelberg et
al (1), the rate of local
recurrence following osteosarcoma surgery is generally 4–10%.
However, the same rate in China is higher, at 10–20% (3). The recurrence of osteosarcoma
generally occurs within less than two years post-surgery. Grimer
et al (4) studied 96
patients with recurrent osteosarcoma and identified an average time
of post-operative recurrence as 11 months (range, 1–66 months),
during which, 60% of patients relapsed in less than one year
post-surgery and 82% of patients relapsed in less than two years
(5). Data from the Rizzoli
Orthopaedic Institute (Bologna, Italy) indicated that the
recurrence of osteosarcoma was significantly associated with the
surgical margins and the effectiveness of pre-operative
chemotherapy; if the surgical margin met the requirements, 97% of
patients showed no local recurrence in 7 years, otherwise, the rate
dropped to 71%. Following chemotherapy, the rate of local
recurrence was 4% in patients with tumor cell necrosis >90%,
otherwise, the rate increased to 10% (5).
Studies have indicated that a post-operative local
recurrence of osteosarcoma may develop at 5 years, or even up to 20
years, post-surgery. The data from the Cooperative Osteosarcoma
Study Group (COSS) (6) showed that
between 1980 and 1998, only 23 (1.4%) of 1,702 cases suffered from
a post-operative recurrence of osteosarcoma after five years (up to
14 years), which was defined as a late local recurrence of
osteosarcoma. To the best of our knowledge, the present study has
described 3 cases of recurrent osteosarcoma at 6.5, 10 and 5.2
years post-surgery, respectively, and is the first study of late
local recurrence in Chinese patients.
The literature was searched using keywords including
osteosarcoma, late local recurrence, limb and pelvic, and it was
found that only 10 cases in the literature met the requirements for
late local recurrent osteosarcoma (7–9).
Therefore, to date, only a total of 13 patient cases, including
those in the present study, have been reported (Table I).
 | Table I.Clinical characteristics of 13
patients with late recurrent osteosarcoma. |
Table I.
Clinical characteristics of 13
patients with late recurrent osteosarcoma.
| Patient No. | Ref. | Age at reccurrance
(years) | Gender | Site | Histology | Pre-operative
chemotherapy result | Recurrence time
(years) | Retreatment | Follow-up
(years) | Outcome |
|---|
| 1 | 6 | 38.0 | M | FD | Fib | Poor | 7.5 | NR | 4.50 | Survived |
| 2 | 6 | 15.0 | F | FD | Tel | Poor | 5.5 | NR | 3.00 | Succumbed |
| 3 | 6 | 13.0 | M | TD | CO | Good | 5.3 | NR | 0.60 | Survived |
| 4 | 6 | 34.0 | M | FD | Chb | Poor | 8.5 | NR | 4.70 | Succumbed |
| 5 | 6 | 18.0 | M | TP | Fib | Good | 5.5 | NR | 3.90 | Succumbed |
| 6 | 7 | 24.7 | M | NR | NR | NR | 9.7 | OP/CH | 1.40 | Succumbed |
| 7 | 7 | 27.3 | M | NR | NR | NR | 11.3 | OP/CH | 3.60 | Survived |
| 8 | 7 | 32.3 | M | NR | NR | NR | 19.3 | OP/CH | 1.30 | Succumbed |
| 9 | 8 | 41.0 | F | P | Chb/Ob | NR | 17.0 | OP/RA | NR | NR |
| 10 | 1 | 42.0 | F | P | Fib/Tel | NR | 19.0 | OP | NR | Succumbed |
| 11 | Study | 13.0 | F | FD | CO | Good | 6.5 | OP/CH | 0.75 | Survived |
| 12 | Study | 35.0 | M | FD | Ob | Good | 10.0 | OP/CH | 0.80 | Survived |
| 13 | Study | 17.0 | F | TD | Hb | NR | 5.2 | OP | 0.50 | Survived |
These 13 patients consisted of eight males and five
females. The average age of recurrence was 25.56 years (range,
13–42 years). A total of five cases involved the distal femur, the
distal tibia and acetabulum were involved in two cases each and one
case involved the proximal tibia (the locations of the recurrent
lesions in the remaining cases were not described). The
histological types of the recurrent tumors were as follows: three
patients with fibroblastic-type, two with traditional-type, two
with mixed-type, one with chondroblastic-type and one with
telangiectasia-type osteosarcoma (the remaining cases were not
described). The average time of post-operative recurrence was 10.02
years (range, 5.2–19.3 years). The treatment modalities were
surgery with chemotherapy in five cases, surgery with radiotherapy
in one case, surgery alone in two cases and one case did not
complete the treatment (the remaining cases were not described).
The average time of follow-up was 2.28 years (range, 0.5–4.7
years), excluding two cases that were not recorded. In total, six
patients survived up to 4.5 years and 6 patients succumbed within
the timespan of 0.6–4.7 years. The survival outcome was not
recorded in one case.
The present data demonstrate that patients with late
recurrent osteosarcomas are extremely rare, accounting for only 1%
of the total osteosarcoma cases. The clinical manifestations do not
exhibit evident specificity and are not significantly correlated
with parameters that include the tumor location, histological type,
efficacy of pre-operative chemotherapy and surgical approach
(7). There is no consensus on the
treatment plan for these patients, as this should be determined
based on the general condition of the patients and the experience
of the surgeon. Although a general post-operative chemotherapy
regimen is applied, the drug toxicity during the treatment should
also be monitored. In the present study, the cumulative dose of
doxorubicin given to the patient in case 1 had reached the maximal
tolerance, and the chemotherapy following the second surgery had to
be terminated due to cardiac toxicity. The clinical outcomes of
these patients were not ideal. In the present series of studies,
out of the 12 patients who had a follow-up record, six cases
survived and six succumbed to their condition. Evaluating the
long-term prognoses of the these late recurrence osteosarcoma
patients remains difficult due to the short follow-up times applied
in the present study and literature cases. Whether neoadjuvant
chemotherapy and surgical treatment may be applied to these late
recurrence patients requires further study and observation.
The present series of data suggest that although the
survival rate was continuously improved with the increased
application of neoadjuvant chemotherapy and limb salvage surgery,
attention should be focused on the long-term regular follow-up of
these osteosarcoma patients. Certain researchers suggest that the
follow-up time should be extended to 10 years (8), and that the patients should be
followed up every 6 months from 5 years post-surgery. While it is
of great importance to exclude the presence of lung metastases,
more attention should be paid to the abnormal changes at the
surgical site. Although routine ECT examinations are a viable way
to exclude the presence of bone metastases, it is recommended that
the patients in whom recurrence is suspected should be examined by
PET/CT. One patient in the present study did not show an
abnormality in the pre- or post-operative ECT, but the PET/CT
examination confirmed the diagnosis of the post-operative
pathology.
References
|
1.
|
Spiegelberg BGI, Gokaraju K, Parratt MT,
Flanagan AM, Cannon SR and Briggs TWR: Late recurrence of pelvic
osteosarcoma: a case report and review of the literature. Grand
Rounds. 10:8–12. 2010.
|
|
2.
|
Yu XC, Xu M, Song RX and Xu SF: Marginal
resection for osteosarcoma with effective preoperative
chemotherapy. Orthop Surg. 1:196–202. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
3.
|
Zhang Q, Niu XH, Cai YB, Hao L and Ding Y:
Prognostic factors for the local recurrence of osteosarcoma in
extremities treated with combined therapy. Zhonghua Wai Ke Za Zhi.
45:1114–1117. 2007.(In Chinese).
|
|
4.
|
Grimer RJ, Sommerville S, Warnock D,
Carter S, Tillman R, Abudu A and Spooner D: Management and outcome
after local recurrence of osteosarcoma. Eur J Cancer. 41:578–583.
2005. View Article : Google Scholar : PubMed/NCBI
|
|
5.
|
Bacci G, Ferrari S, Mercuri M, Bertoni F,
Picci P, Manfrini M, Gasbarrini A, Forni C, Cesari M and Campanacci
M: Predictive factors for local recurrence in osteosarcoma: 540
patients with extremity tumors followed for minimum 2.5 years after
neoadjuvant chemotherapy. Acta Orthop Scand. 69:230–236.
1998.PubMed/NCBI
|
|
6.
|
Bielack SS, Kempf-Bielack B, Delling G,
Exner GU, Flege S, Helmke K, Kotz R, Salzer-Kuntschik M, Werner M,
Winkelmann W, Zoubek A, Jürgens H and Winkler K: Prognostic factors
in high-grade osteosarcoma of the extremities or trunk: an analysis
of 1,702 patients treated on neoadjuvant cooperative osteosarcoma
study group protocols. J Clin Oncol. 20:776–790. 2002. View Article : Google Scholar
|
|
7.
|
Hauben EI, Bielack S, Grimer R, Jundt G,
Reichardt P, Sydes M, Taminiau AH and Hogendoorn PC:
Clinico-histologic parameters of osteosarcoma patients with late
relapse. Eur J Cancer. 42:460–466. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
8.
|
Ferrari S, Briccoli A, Mercuri M, Bertoni
F, Cesari M, Longhi A and Bacci G: Late relapse in osteosarcoma. J
Pediatr Hematol Oncol. 28:418–422. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
9.
|
Welck MJ, Gikas PD, Pearce P, Bhumbra R,
Briggs TW and Cannon S: Local recurrence of osteosarcoma after 17
years. Ann R Coll Surg Engl. 91:W17–W19. 2009.PubMed/NCBI
|