Introduction
Cancer of unknown primary site (CUP) is a category
of malignancy with undetectable primary site upon diagnosis. It is
characterized by diverse clinical manifestations and poor prognosis
(1). The histological types include
adenocarcinoma, squamous cell carcinoma, neuroendocrine tumors and
carcinoma not otherwise specified. Adenocarcinoma of unknown
primary site accounts for 60–70% of all cases of CUP and is
commonly identified in the liver, lung, bone and lymph nodes
(1,2). Metastatic adenocarcinoma of unknown
primary site, first presenting with malignant renal subcapsular
effusions, is extremely rare and has not been analyzed in previous
studies. The current case report presents a patient with
adenocarcinoma of unknown primary site that initially presented
with renal subcapsular and pleural effusion followed by
carcinomatous meningitis. The treatment of this specific type of
carcinoma is subsequently discussed. Written informed consent was
obtained from the patient.
Case report
Patient presentation and diagnosis
A 45-year-old female was admitted to The
Comprehensive Cancer Center, Drum Tower Hospital (Nanjing, China)
on April 9, 2006 with flank pain, cough and dyspnea. One month
prior to admission, the patient had suffered from left flank pain.
Abdominal ultrasonography at the patient’s local hospital revealed
a subcapsular effusion, a small cyst in the left kidney and a
calculus of 0.8 cm in diameter in the upper right ureter. The
patient was treated for lithiasis for ~1 month with no amelioration
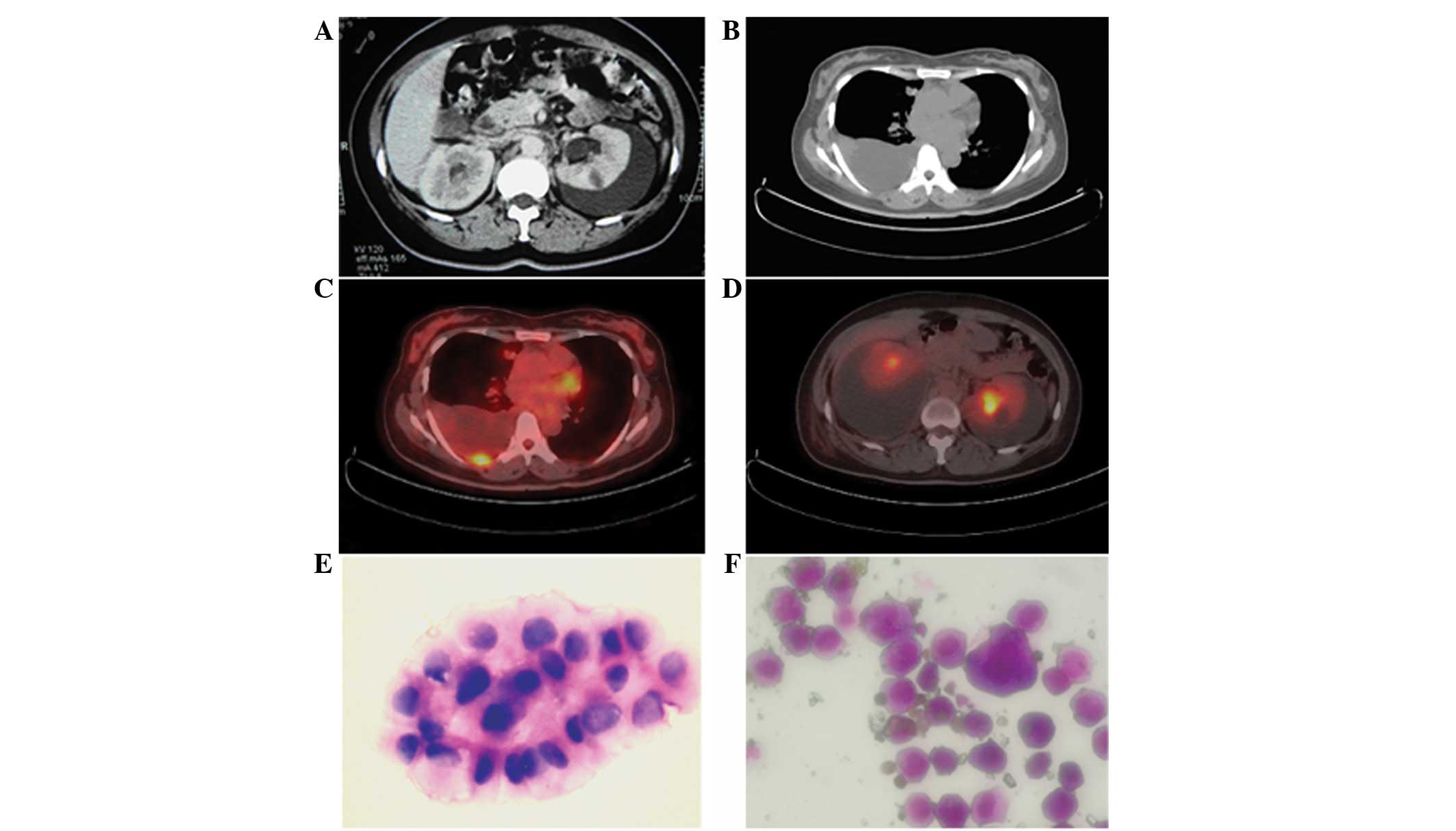
and subsequently developed a cough and dyspnea. A computed
tomography (CT) scan revealed right pleural and subcapsular
effusions in the left kidney (Fig.
1A). A thorough examination of the individual was performed,
including an intravenous urogram, mammography, gynecological
ultrasonography, whole gastrointestinal barium contrast imaging and
colonoscopy, however, no abnormalities were identified.
Upon admission, a physical examination revealed high
blood pressure (160/100 mmHg), lowered respiratory sounds in the
right lung and a mass in the left loin. Blood tests showed an
elevated level of serum creatinine (196 μmol/l) and serum tumor
markers, cancer antigen (CA)125 (168 U/ml; reference range, <35
U/ml), carcinoembryonic antigen (CEA; 15.3 ng/ml; reference range,
<5.0 ng/ml) and CA153 (68 U/ml; reference range, <25 U/ml)
and a urine test was negative. The cytopathological examination of
the pleural effusion was positive for poorly-differentiated
adenocarcinoma cells. To identify the primary tumor site, the
patient received a systemic positron emission tomography (PET)/CT
scan, which identified a small nodule measuring 7×12×9 mm in the
upper lobule of the right lung and right pleural (Fig. 1B and C) and subcapsular effusions of
the kidneys (Fig. 1D), with normal
18F-fluorodeoxyglucose (FDG) uptake. Due to its size and
site, a fine-needle biopsy of the lung nodule was not performed and
therefore, the patient was diagnosed with a carcinoma of unknown
primary site.
Treatment and clinical course
Chemotherapy was initiated and agents with high
renal toxicity were excluded to avoid the deterioration of the
patient’s kidney function. Intravenous docetaxel (40
mg/m2 on days 1 and 8, every 3 weeks) plus oxaliplatin
(75 mg/m2 on days 1 and 8, every 3 weeks) and
intrapleural interleukin-2 (1×109 U on days 3 and 10,
every 3 weeks) was administered. The pleural effusion subsided
after being drained three times and intrapleural interleukin-2
administration. Following the initial course of chemotherapy, the
cough and dyspnea ameliorated and serum levels of creatinine and
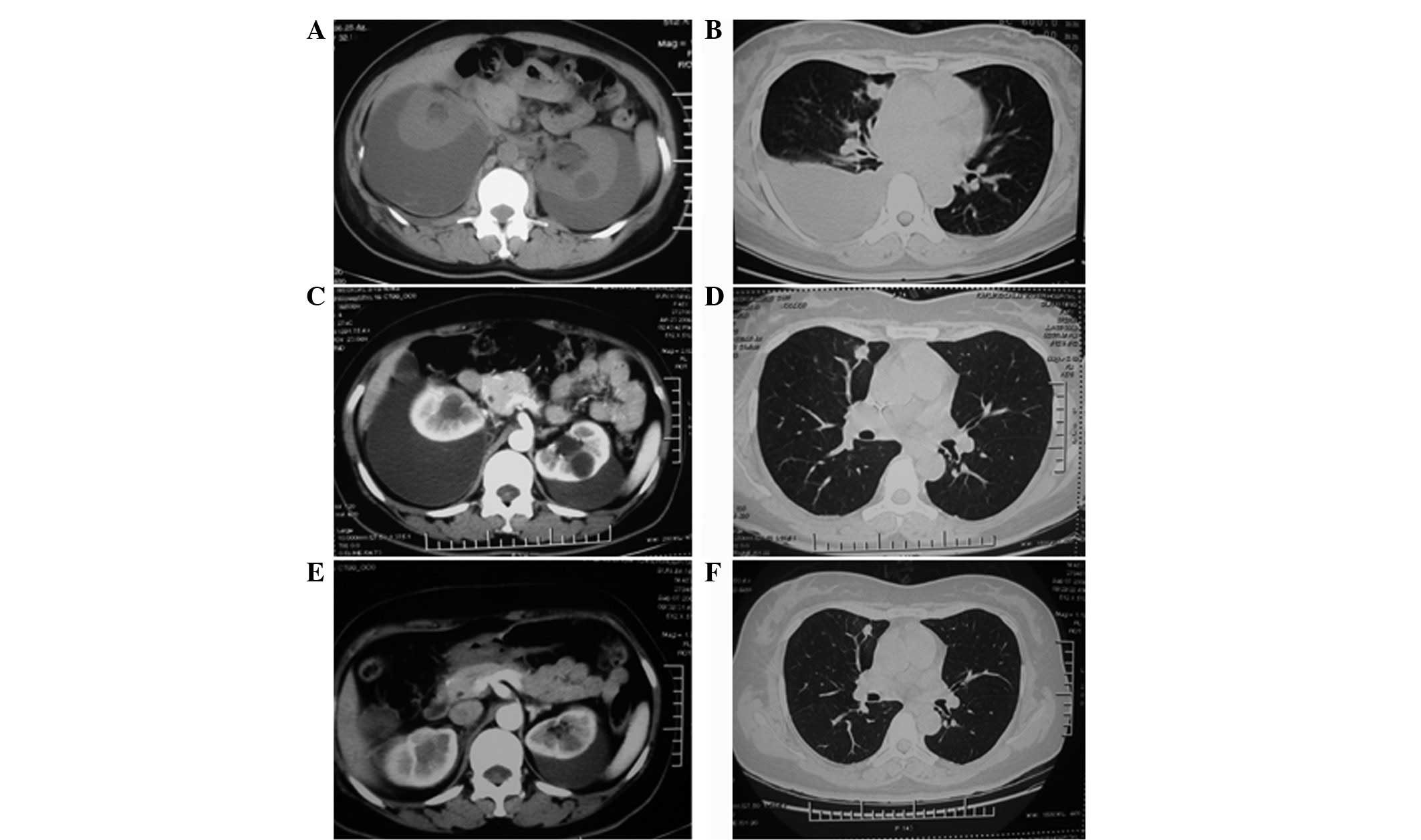
tumor markers decreased. Following three cycles of chemotherapy,
the CT scan showed no change in the pulmonary nodule (Fig. 2B and D) or subcapsular effusion
(Fig. 2A and C). Next, renal
subcapsular drainage was performed and ~330 and 960 ml stale
hematoid fluid was aspirated from the left and right sides,
respectively. The levels of CA125, CA199 and CA153 tumor markers
were significantly elevated in the drained fluid and adenocarcinoma
cells were evident upon analysis of the drainage cytology (Fig. 1E). Following sequential treatments
of interleukin-2 and bleomycin administered intrasubcapsularly, the
amount of drained fluid decreased (Fig.
2C and E) and turned yellow and clear. The abdominal symptoms
were ameliorated and the patient’s blood pressure and serum
creatinine level returned to normal; however, no clear changes to
the lung nodule were observed (Fig.
2F). Subsequently, the patient received an additional three
cycles of systemic chemotherapy with gemcitabine (1,000
mg/m2 on days 1 and 8, every 3 weeks) plus cisplatin (25
mg/m2 daily for 3 days ).
The patient’s condition was stable prior to an
intense headache that developed three weeks after the final
administration of gemcitabine plus cisplatin. The individual
exhibited no vomiting or blurred vision, the blood pressure
remained normal and the brain and spinal MRI scans were negative. A
lumber puncture was performed and the cerebrospinal fluid was
positive for a large number of adenocarcinoma cells (Fig. 1F). Immunostaining was positive for
epithelial membrane antigen and pan-cytokeratin, but negative for
vimentin, glial fibrillary acidic protein, cluster of
differentiation (CD)3, CD20, CD30 and CD68. Meningeal metastasis
and carcinomatous meningitis were diagnosed and the patient
received 10 mg intrathecal methotrexate weekly, but refused cranial
and spinal cord radiation therapy. Following a total of 40 mg
intrathecal methotrexate chemotherapy, the patient’s headache was
ameliorated and the cerebrospinal fluid was negative for tumor
cells. The individual was administered with 250 mg gefitinib daily
for the following nine months, during which the disease status was
stable. However, following this, the patient developed paroxysmal
syncope and epileptic seizures. No abnormalities were identified in
the cranial MRI. Following an additional four months of treatment,
the patient succumbed to carcinoma of unknown primary site on March
20, 2008, ~23.5 months after the initial diagnosis. An autopsy was
not performed according to the wishes of the patient’s family.
Discussion
CUP comprises 2–5% of all diagnosed tumors (1,2). It
represents a heterogeneous group of metastatic tumors that share
unique clinical features, including early dissemination, a clinical
absence of a primary tumor, unpredictable metastatic patterns and
aggressiveness, and patients tend to have an unfavorable prognosis.
Adenocarcinoma of unknown primary site commonly presents in the
liver, lungs, lymph nodes and bones and is rarely identified with
malignant pleural or peritoneal effusions (3). A malignant renal subcapsular effusion
of unknown primary site is extremely rare and has not been analyzed
in previous studies. The current case report presents an unusual
manifestation of CUP with massive malignant renal subcapsular and
pleural effusions and subsequent carcinomatous meningitis. No solid
metastasis was identified during a thorough examination.
Renal subcapsular effusions may be hydroceles or
hematoceles, and various mechanisms, including venous, lymphatic
and urine regurgitation, may contribute to a subcapsular hydrocele
of the kidney. However, a hematocele is likely to be caused by
trauma, a renal tumor, vascular disease, infection, nephritis,
blood dyscrasias, calculus or hydronephrosis (4). With an incidence rate of 57.7%,
spontaneous subcapsular or perirenal hematomas are commonly
associated with primary renal neoplasms, of which 33.4% are
malignant with renal cell carcinoma predominance and 24.3% are
benign with angiomyolipoma predominance (5). In addition, tumors occasionally arise
from metastasis of extrarenal primary tumors to the kidney
(6). In the present case report,
the subcapsular effusion was hematoid and positive for
adenocarcinoma cells. The renal parenchyma was negative for any
discernible lesions with the exception of a cyst in the left
kidney, which did not resemble a common entity of a metastasis of
adenocarcinoma cells and did not change throughout the duration of
the treatment process. In addition, the urine test was negative for
tumor cells or hematuria. As the effusion was bilateral,
subcapsular metastasis from the extrarenal site was
hypothesized.
No consensus has been made with regard to the
standard therapy for CUP and particularly for multiple malignant
cavity effusions. Empiric chemotherapy with 5-fluorouracil,
doxorubicin or cisplatin-based regimens have previously produced
relatively low response rates and few complete responses (7). Broad spectrum antineoplastic agents,
including taxanes, topoisomerase I inhibitors, gemcitabine and
vinorelbine, have been investigated in epithelial CUP, and platinum
and taxane combination therapy is now widely used in clinical
practice. However, a previous meta-analysis showed that no types of
chemotherapy have been confirmed to prolong survival in patients
with CUP (8).
Paclitaxel/docetaxel-containing combination regimens have been used
in specific phase II trials and the preliminary results have shown
response rates between 23 and 38.7% (9–11).
Briasoulis et al reported encouraging results from phase II
data on carboplatin and paclitaxel combination therapy for patients
with CUP (12). The overall
response rate by an intention-to-treat analysis was 38.7% and the
median overall survival time was 13 months with a median follow-up
of 28 months. A recent randomized study compared empiric therapy
with paclitaxel/carboplatin/etoposide against
gemcitabine/irinotecan, each followed by single-agent gefitinib,
and subsequently identified a comparable efficacy. However,
gemcitabine/irinotecan therapy revealed a more favorable toxicity
profile (13). In the current case
report, the docitaxel/oxiplatin and gemcitabine/cisplatin regimens
were administered to the patient successively, but the efficacy was
limited since the tumor rapidly metastasized to the meninges and
caused carcinomatous meningitis.
As a maintenance therapy, gefitinib was effective
and the patient’s condition was stabilized for nine months despite
metastasis of the tumor to the meninges and subsequent
carcinomatous meningitis, for which the median survival time is 2–3
months. Patients untreated or unresponsive to treatment exhibit a
median survival of 4–6 weeks (14,15).
Overexpression of epidermal growth factor receptor (EGFR) has been
observed frequently in a large subset of CUP and gefitinib is
effective in a broad spectrum of tumor types (16–19).
Although no previous randomized studies have analyzed the effect of
gefitinib in CUP, a previous prospective study reported that the
combination of vascular endothelial growth factor receptor
inhibitor (bevacizumab) and EGFR inhibitor (erlotinib) in CUP has a
better median survival than previously reported with second-line
chemotherapy and is similar to the results of a number of
first-line therapies (20).
Gefitinib maintenance therapy was also included in a recent
prospective randomized trial (13).
The role of gefitinib in adenocarcinoma with CUP is promising and
must be analyzed in future studies.
In conclusion, the current case report presents the
case of a patient with a malignant effusion in multiple cavities
and demonstrates the intracavity administration of chemotherapeutic
agents. Interleukin-2 appeared to be effective for controlling the
effusion, however, systemic chemotherapy with docetaxel plus
oxaliplatin, followed with gemcitabine plus cisplatin, appeared
non-effective and the patient exhibited disease progression with
involvement of the central nervous system, indicating the
refractory entity and poor prognosis of this type of carcinoma. The
overall survival time of the patient was ~24 months, which was
considerably higher than the normal median survival of individuals
with CUP. Gefitinib was identified to be promising for maintenance
therapy and was shown to prolong the patient’s survival.
Acknowledgements
The authors would like to thank Tom Morse (Office of
the President, Drum Tower Hospital, Medical School of Nanjing
University, Nanjing, Jiangsu, China) for his assistance in
correcting the original manuscript.
References
|
1
|
Pavlidis N, Briasoulis E, Hainsworth J and
Greco FA: Diagnostic and therapeutic management of cancer of an
unknown primary. Eur J Cancer. 39:1990–2005. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Hainsworth JD and Greco FA: Treatment of
patients with cancer of an unknown primary site. N Engl J Med.
329:257–263. 1993. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Morris GJ, Greco FA, Hainsworth JD, et al:
Cancer of unknown primary site. Semin Oncol. 37:71–79. 2010.
View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Kendall AR, Senay BA and Coll ME:
Spontaneous subcapsular renal hematoma: diagnosis and management. J
Urol. 139:246–250. 1988.PubMed/NCBI
|
|
5
|
McDougal WS, Kursh ED and Persky L:
Spontaneous rupture of the kidney with perirenal hematoma. J Urol.
114:181–184. 1975.PubMed/NCBI
|
|
6
|
Demos TC, Schiffer MS and Reynes CJ:
Metastatic leiomyosarcoma of the kidney with spontaneous perirenal
hemorrhage. Diagn Imaging Clin Med. 53:87–90. 1984.PubMed/NCBI
|
|
7
|
Hainsworth JD and Greco A: Neoplasms of
unknown primary site. Holland-Frei Cancer Medicine. Bast RC Jr,
Kufe DW, Pollock RE, et al: 5th edition. BC Decker; Hamilton, ON,
Canada: pp. 2114–2124. 2000
|
|
8
|
Golfinopoulos V, Pentheroudakis G, Salanti
G, et al: Comparative survival with diverse chemotherapy regimens
for cancer of unknown primary site: multiple-treatments
meta-analysis. Cancer Treat Rev. 35:570–573. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Greco FA, Erland JB, Morrissey LH, et al:
Carcinoma of unknown primary site: phase II trials with docetaxel
plus cisplatin or carboplatin. Ann Oncol. 11:211–215. 2000.
View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Greco FA, Burris HA III, Litchy S, et al:
Gemcitabine, carboplatin and paclitaxel for patients with carcinoma
of unknown primary site: a Minnie Pearl Cancer Research Network
study. J Clin Oncol. 15:1651–1656. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
El-Rayes BF, Shields AF, Zalupski M, et
al: A phase II study of carboplatin and paclitaxel in
adenocarcinoma of unknown primary. Am J Clin Oncol. 28:152–156.
2005. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Briasoulis E, Kalofonos H, Bafaloukos D,
et al: Carboplatin plus paclitaxel in unknown primary carcinoma: a
phase II Hellenic Cooperative Oncology Group Study. J Clin Oncol.
18:3101–3107. 2000.PubMed/NCBI
|
|
13
|
Hainsworth JD, Spigel DR, Clark BL, et al:
Paclitaxel/carboplatin/etoposide versus gemcitabine/irinotecan in
the first-line treatment of patients with carcinoma of unknown
primary site: a randomized, phase III Sarah Cannon Oncology
Research Consortium Trial. Cancer J. 16:70–75. 2010. View Article : Google Scholar
|
|
14
|
Grant R, Naylor B, Greenberg HS and Junck
L: Clinical outcome in aggressively treated meningeal
carcinomatosis. Arch Neurol. 51:457–461. 1994. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Jayson GC and Howell A: Carcinomatous
meningitis in solid tumours. Ann Oncol. 7:773–786. 1996. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Pavlidis N, Briassoulis E, Bai M, et al:
Overexpression of C-myc, Ras and C-erbB-2 oncoproteins in carcinoma
of unknown primary origin. Anticancer Res. 15:2563–2567.
1995.PubMed/NCBI
|
|
17
|
Fukuoka M, Yano S, Giaccone G, et al:
Multi-institutional randomized phase II trial of gefitinib for
previously treated patients with advanced non-small-cell lung
cancer (The IDEAL 1 Trial) [corrected]. J Clin Oncol. 21:2237–2246.
2003.
|
|
18
|
Massard C, Voigt JJ, Laplanche A, et al:
Carcinoma of an unknown primary: are EGF receptor, Her-2/neu and
c-Kit tyrosine kinases potential targets for therapy? Br J Cancer.
97:857–861. 2007.PubMed/NCBI
|
|
19
|
Kris MG, Natale RB, Herbst RS, et al:
Efficacy of gefitinib, an inhibitor of the epidermal growth factor
receptor tyrosine kinase, in symptomatic patients with non-small
cell lung cancer: a randomized trial. JAMA. 290:2149–2158. 2003.
View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Hainsworth JD, Spigel DR, Farley C, et al;
Minnie Pearl Cancer Research Network. Phase II trial of bevacizumab
and erlotinib in carcinomas of unknown primary site: the Minnie
Pearl Cancer Research Network. J Clin Oncol. 25:1747–1752. 2007.
View Article : Google Scholar : PubMed/NCBI
|