Introduction
Postoperative ileus (POI) is described as a
transient impairment of bowel motility that may occur following
major surgery (1). The process of
postoperative bowel recovery following abdominal surgery, including
colectomy, typically lasts for 3–5 days (2). Prolonged postoperative ileus (PPOI)
usually manifests with nausea, vomiting, abdominal pain and
distension and/or delay in the passage of flatus and stool. PPOI is
associated with prolonged hospitalization and readmission and high
morbidity and mortality (3).
Although PPOI is a severe condition that requires immediate
diagnosis and appropriate treatment (4), the accurate and early diagnosis of
PPOI remains difficult due to a lack of appropriate laboratory
parameters (5). Early detection of
PPOI is critical for early intervention and minimizing
mortality.
Cytokines are pleiotropic substances with a
diversity of functions (6) and the
cytokines IL-1β, IL-6 and TNF-α are significant mediators of the
acute-phase response in humans (6,7). It
has been previously reported that peritoneal cytokines are
sensitive indicators of the postoperative inflammatory reaction and
may be predictors of serious surgical complications (8). In addition, monitoring peritoneal
cytokine levels following elective gastrointestinal surgery may
indicate severe intra-abdominal complications (9) and the present study investigated
whether the measurement of peritoneal cytokines was an early
predictor of PPOI following colorectal surgery.
Patients and methods
Patients
In the present study, 100 consecutive patients (60
male and 40 female) with carcinoma of the sigmoid or rectum and
scheduled to undergo elective open anterior resection under general
anesthesia between January and December 2011 were included. Of
note, ileostomy was not perfomed on patients during surgery.
Postoperative care for all patients included an analgesia protocol
using a patient-controlled analgesia (PCA) pump of morphine
chlorhydrate for 48 h and the dose of morphine chlorhydrate used
was recorded. Exclusion criteria included patients who had received
preoperative radiotherapy or chemotherapy, undergone emergency
surgery and received anti-inflammatory drugs including
corticosteroids and immunosuppressants preoperatively for
infectious or inflammatory diseases. The mean age of the 100
eligible patients was 59 years (range, 24–87 years) at the time of
surgery. The site of the carcinoma was the sigmoid colon in 26
patients and the rectum in 74 patients. All the patients underwent
bowel resection with end-to-end anastomosis with the aid of
circular staplers. Prior to the closure of the peritoneum, a
silastic drainage tube was placed in the pelvic base of all the
patients and removed 5–12 days following surgery. This study was
approved by the ethics committee of Xinhua Hospital Affiliated to
Shanghai Jiaotong University School of Medicine. Written informed
consent was obtained from the patients.
Definition of PPOI
POI is commonly observed ~3–5 days following major
abdominal surgery and presents a number of clinical symptoms,
including abdominal pain or distension, nausea or vomiting, the
inhibited passage of feces and/or flatus and abnormal bowel sounds.
POI develops in the majority of patients undergoing abdominal
surgery and it is considered to be a normal phenomenon during the
postoperative course. However, a previous study (1) reported that among patients who
underwent abdominal surgery, 7% developed PPOI with the observation
of clinical manifestations and radiological imaging for ileus,
which usually required clinical intervention. In addition, findings
of another study demonstrated that the recovery of small bowel
motility and absorption occurs within hours of surgery, whereas
gastric and colonic functions may require 2–5 days (10). An improved clinical definition of
PPOI is an ileus that persists for >6 days following surgery
with evident clinical symptoms and radiological imaging which must
be diagnosed at an early stage for immediate treatment (11). This definition was utilized in the
present study and therefore, patients were divided into two groups:
PPOI (with evident clinical symptoms and radiological imaging of
PPOI) and No-PPOI (with no clinical symptoms and radiological
imaging of PPOI).
Sampling
Samples of abdominal exudate were collected via
abdominal drains on postoperative days 1, 3 and 5 for detection.
Samples were obtained as fresh material within 2 h of the morning
emptying of the drainage bag. Measurements of 5 ml abdominal
exudate were collected into a vacutainer tube and immediately
centrifuged at 1,400 × g for 15 min. Samples were stored at −80°C
until analysis. The levels of IL-1β, IL-6 and TNF-α were measured
by enzyme-linked immunosorbent assays (R&D Systems,
Minneapolis, MN, USA). Each assay was performed in duplicate and a
standard curve was constructed using recombinant cytokines. The
minimum sensitivity of each cytokine assay was 2.0 pg/ml.
Statistical analysis
Comparison of frequencies between the groups was
analysed using the χ2 test with Yates' correction.
Continuous data were presented as the mean ± SD. Mean values
between the two groups were compared using the unpaired t-test. For
comparisons involving more than two groups, a one-way analysis of
variance was applied and changes with time were analysed using the
paired t-test. P<0.05 was considered to indicate a statistically
significant difference.
Results
Clinical characteristics
PPOI occurrence was clinically proven in 8/100
patients (8%; 6 male and 2 female) who underwent elective open
resection for carcinoma of the sigmoid or rectum. The median number
of days to PPOI diagnosis was 12 days (range, 10–15 days) following
surgery. Conservative treatment was administered to 6/8 PPOI
patients to promote bowel movement and the remaining 2 patients
were urgently reoperated on for adhesiolysis. All 8 PPOI patients
recovered well following treatment and there were no mortalities
for the duration of the present study. No significant differences
were observed among the majority of clinical variables, including
age, gender, BMI, location of carcinoma, intraoperative blood loss,
operative time, dose of morphine during PCA and duration of
postoperative hospitalization in the No-PPOI group when compared
with that of the PPOI group. However, the number of days to the
first passage of flatus was significantly higher in the PPOI group
when compared with that of the No-PPOI group (Table I).
 | Table IData of patients receiving anterior
resection of the sigmoid or rectum. |
Table I
Data of patients receiving anterior
resection of the sigmoid or rectum.
| Variables | No-PPOI | PPOI | P-value |
|---|
| Age, years | 61.6±17.6 | 53.37±8.41 | 0.192 |
| Gender | | | 0.471 |
| Male | 54 | 6 | |
| Female | 38 | 2 | |
| BMI | 23.62±4.62 | 25.87±4.48 | 0.213 |
| Site of
carcinoma | | | 0.160 |
| Sigmoid colon | 24 | 2 | |
| Rectum | 68 | 6 | |
| Blood loss, ml | 186.32±12.17 | 272.86±78.40 | 0.315 |
| Operative time,
min | 164.68±30.62 | 184.43±32.60 | 0.447 |
| Dose of morphine
during PCA, mg | 188.22±117.61 | 194.84±127.30 | 0.852 |
| Time to first passage
of flatus, days | 3.09±1.09 | 10.00±1.41 | 0.001 |
| Postoperative
hospital stay, days | 15.62±4.46 | 35.43±12.21 | 0.043 |
Peritoneal cytokines
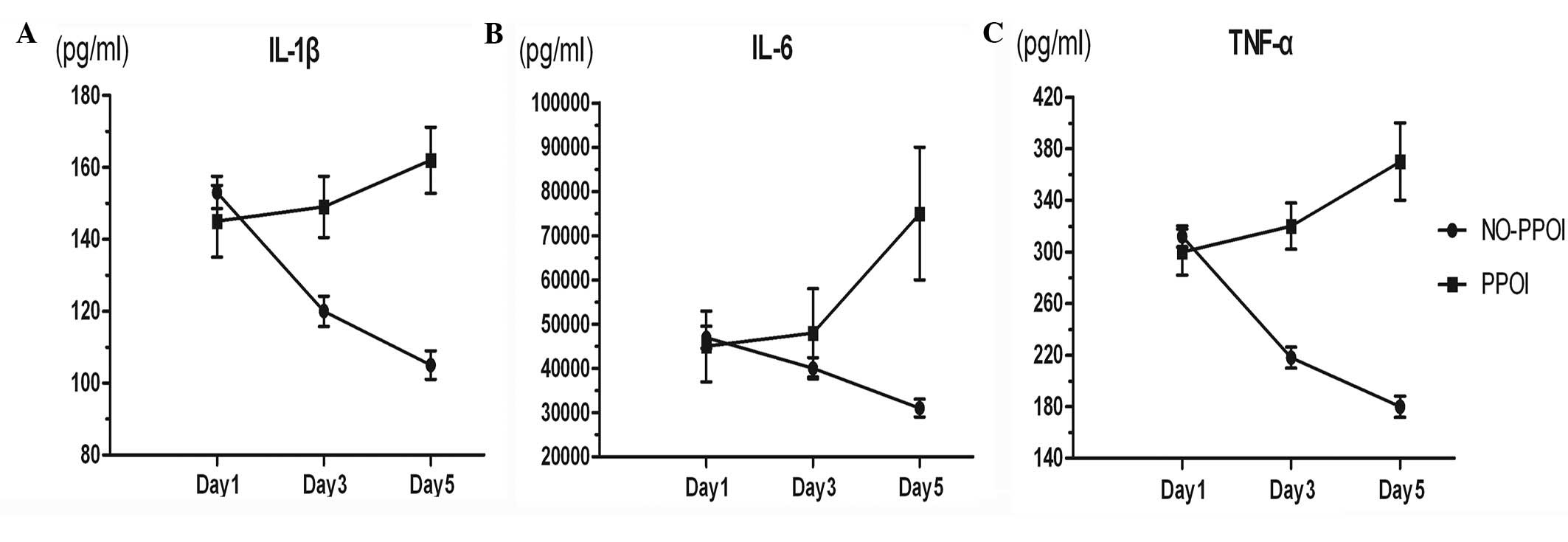
The values of IL-1β, IL-6 and TNF-α levels on
postoperative days 1, 3 and 5 are shown in Table II. The impact between patient
demographic factors on day 1 and peritoneal cytokine production was
also examined (Table III). Age
(<60/≥60 years), gender, normal or poor (>10% loss of body
weight) preoperative nutritional status, site of carcinoma (sigmoid
colon/rectum) and the Dukes' stage (A/B/C) did not affect the
peritoneal cytokine levels. The changes in peritoneal cytokine
level for a 5-day duration following surgery are shown in Fig. 1. No significant differences were
noted on postoperative days 1 and 3 among the levels of IL-1β, IL-6
and TNF-α and the 8 patients who developed PPOI when compared with
those of the 92 patients that did not develop PPOI. However, on
postoperative day 5 the levels of IL-1β, IL-6 and TNF-α were
significantly higher in patients who developed PPOI when compared
with those of patients who did not develop PPOI. The levels of
IL-1β, IL-6 and TNF-α decreased in the 92 patients without PPOI and
significantly increased in the 8 patients with PPOI. During the
first 5 days following surgery the IL-1β levels increased in 7/8
patients (88%) with PPOI vs. 16/92 patients (17%) without PPOI
(P=0.0001), the IL-6 levels increased in 8/8 patients (100%) with
PPOI vs. 15/92 patients (16%) without PPOI (P<0.0001) and the
TNF-α levels increased in 8/8 patients (100%) with PPOI vs. 13/92
patients (14%) without PPOI (P<0.0001).
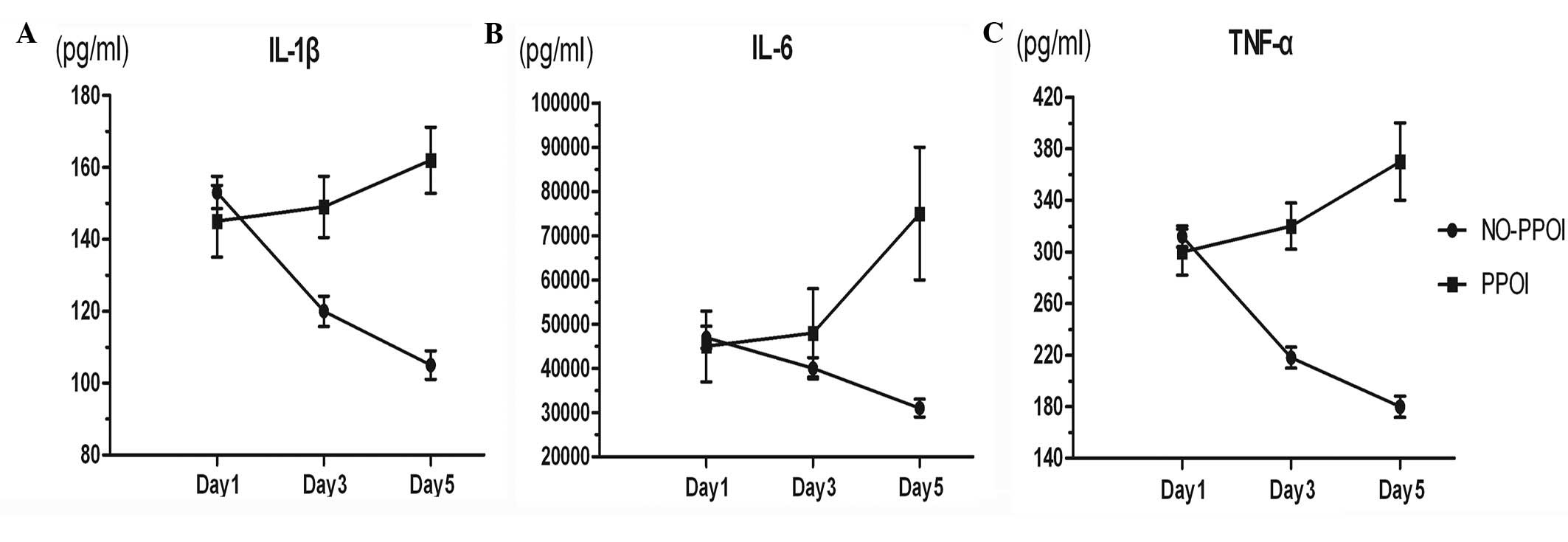 | Figure 1No significant differences were
observed between the peritoneal cytokine levels on postoperative
days 1 and 3 and patients who developed PPOI when compared with
those that did not develop PPOI (day 1: IL-1β, P=0.23; IL-6, P=0.35
and TNF-α, P=0.62 and day 3: IL-1β, P=0.34; IL-6, P=0.65 and TNF-α,
P=0.29). By contrast, cytokine levels on postoperative day 5 were
significantly higher in patients who developed PPOI when compared
with patients that did not develop PPOI (IL-1β, P=0.012; IL-6,
P<0.0001 and TNF-α, P<0.0001). Cytokine levels significantly
increased in the first 5 days following surgery in patients who
developed PPOI (IL-1β, P=0.045; IL-6, P=0.03; TNF-α, P=0.02) and
significantly decreased in patients who did not develop PPOI
(IL-1β, P<0.0001; IL-6, P<0.0001; TNF-α, P<0.0001). IL,
interleukin; TNF, tumour necrosis factor; PPOI, prolonged
postoperative ileus. Data are presented as the mean ± SD. |
 | Table IIPeritoneal cytokine levels on
postoperative days 1, 3 and 5. |
Table II
Peritoneal cytokine levels on
postoperative days 1, 3 and 5.
| Day | IL-1β (pg/ml) | IL-6 (pg/ml) | TNF-α (pg/ml) |
|---|
| 1 | 152±5.4 | 52,000±2600 | 312±10.7 |
| 3 | 126±4.8 | 40,000±2500 | 218±8.9 |
| 5 | 86±5.1 | 36,700±2100 | 197±9.2 |
 | Table IIIPeritoneal cytokine production level
on postoperative day 1 vs. patient demographic factors. |
Table III
Peritoneal cytokine production level
on postoperative day 1 vs. patient demographic factors.
| Variables | n | IL-1β (pg/ml) | IL-6 (pg/ml) | TNF-α (pg/ml) |
|---|
| Age, years |
| <60 | 54 | 149±6.4 | 44000±2,800 | 306±12 |
| ≥60 | 46 | 157±5.6 | 53,200±2,900 | 316±11 |
| P-value | | 0.78 | 0.66 | 0.51 |
| Gender |
| Male | 60 | 157±7.7 | 54,200±2,600 | 298±12 |
| Female | 40 | 149±6.8 | 52,000±2,800 | 325±10 |
| P-value | | 0.82 | 0.53 | 0.23 |
| Preoperative
nutritional status |
| Normal | 82 | 150±7.2 | 52,400±2,500 | 312±11 |
| Poor | 18 | 156±7.5 | 50,800±5,100 | 316±17 |
| P-value | | 0.47 | 0.89 | 0.72 |
| Site of
carcinoma |
| Sigmoid colon | 26 | 148±5.2 | 49,800±2,800 | 314±13 |
| Rectum | 74 | 151±6.2 | 52,100±3,700 | 307±12 |
| P-value | | 0.62 | 0.34 | 0.45 |
| Dukes' stage |
| A | 16 | 148±8.9 | 48,600±5,300 | 314±19 |
| B | 37 | 151±7.4 | 54,300±4,100 | 309±13 |
| C | 47 | 144±6.2 | 51,000±4,400 | 311±15 |
| P-value | | 0.91 | 0.94 | 0.88 |
Discussion
Acute bowel obstruction is a major cause of
morbidity, increased hospitalization costs and emergency conversion
surgery (11,12). Diagnosis of bowel obstruction
traditionally occurs via classic signs including tachycardia,
hypotension, fever, constant pain, peritoneal signs, leukocytosis,
base deficit and metabolic acidosis (13) and abdominal CT (14). The immediate and appropriate
treatment of this condition is critical, however, there are no
accurate diagnostic methods or tools currently available (15). Although the combined evaluation of
clinical, laboratory and radiological observations is recommended,
the preoperative early diagnosis of bowel obstructions cannot be
made or excluded reliably by any identified parameters, individual
or combined or even by experienced clinical judgement (16).
The aim of the present study was to evaluate the
predictive value of peritoneal cytokines for the early diagnosis of
bowel obstructions in patients following surgery for colorectal
carcinoma. Although the value of plasma cytokines for the diagnosis
of PPOI has been evaluated in previous studies (17), it has not been investigated in
abdominal exudate.
Peritoneal cytokines respond extensively following
abdominal surgery and therefore must be a significant marker of
postoperative complications (9).
The IL-1β, IL-6 and TNF-α levels were measured on postoperative
days 1, 3 and 5 to investigate the correlation between changes in
cytokine levels and the development of PPOI. In the normal
postoperative progression, the peak of peritoneal cytokine
production is observed on postoperative day 1 and subsequently
decreases with time (18). The
increased levels of peritoneal cytokines, prior to marked clinical
symptoms, must be a significant marker to predict future
intraabdominal ileus.
Soybel and Zinner (19) reported that ileus is correlated with
the increased expression of local inflammatory cytokines and
chemokines, leukocyte infiltration into the muscularis and the
release of mediators from resident and infiltrating leukocytes.
These mediators are capable of directly inhibiting the contraction
of intestinal smooth muscle and subsequent progression of
ileus.
A systemic cytokine network has been suggested to
induce impaired gastric electrical activity with ileus status
(20). The local inflammatory
status may have a significant modulating role and correlations
between ileus and increased systemic levels of proinflammatory
cytokines (IL-1β, IL-6 and TNF-α) were also identified. Previous
studies (19) have revealed that
the dense network of macrophages specific to the muscularis is
rapidly activated during impaired intestinal motility, thus
initiating an inflammatory cascade of events, including the
upregulation of cytokines, chemokines and kinetically active
substances (21). This local
inflammatory status results in the recruitment and extravasation of
leukocytes into the circular muscle layer. In conjunction with an
increased expression of adhesion molecules, leukocytes inflitrate
through the muscularis externa. The secretion of various potent
leukocytic products directly succeeds and inhibits the contraction
of gastrointestinal smooth muscle.
At present, a marked number of clinical studies have
demonstrated the significance of cytokines as an early and reliable
diagnostic and prognostic tool in several conditions, including
infections, infectious and non-infectious SIRS, sepsis, acute
pancreatitis and other postoperative complications (22). However, compared with that of
systemic (plasma) cytokines, peritoneal cytokines respond
extensively following major abdominal surgery, indicating that the
measurement of peritoneal cytokines is a likely method to determine
postoperative inflammatory reaction (8) which may progress to POI. In future
studies, the preoperative systemic, as well as postoperative
systemic and peritoneal cytokine measurements are likely to be
performed together to investigate whether the cytokines in the
peritoneal fluid are affected by the systemic circulation. In
addition, the systemic and peritoneal cytokine levels following
surgery are likely to be compared to indicate which is the most
suitable for determining PPOI.
Results of the present study demonstrated that the
estimation of cytokine levels from abdominal exudate may prove to
be an early diagnostic tool that is likely to support the
decision-making process of surgeons for the early detection of PPOI
following colorectal surgery. The measurement of peritoneal
cytokines during the early postoperative period functions as a
useful diagnostic marker to predict future PPOI. Therefore, it must
allow for the appropriate therapeutic intervention to minimize
PPOI-related morbidity, similar to that of the use of biologics to
block cytokine action.
Acknowledgements
The present study was supported by the Science and
Technology Commission of Shanghai Municipality (nos. 10DJ1400504
and 09JC1410900) and the personnel training plan of Shanghai City
Health Bureau.
References
|
1
|
Bauer AJ and Boeckxstaens GE: Mechanisms
of postoperative ileus. Neurogastroenterol Motil. 16:54–60. 2004.
View Article : Google Scholar
|
|
2
|
Iyer S, Saunders WB and Stemkowski S:
Economic burden of postoperative ileus associated with colectomy in
the United States. J Manag Care Pharm. 15:485–494. 2009.PubMed/NCBI
|
|
3
|
Wolff BG, Weese JL, Ludwig KA, Delaney CP,
Stamos MJ, Michelassi F, Du W and Techner L: Postoperative
ileus-related morbidity profile in patients treated with alvimopan
after bowel resection. J Am Coll Surg. 204:609–616. 2007.
View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Takeuchi K, Tsuzuki Y, Ando T, Sekihara M,
Hara T, Yoshikawa M and Kuwano H: Clinical studies of strangulating
small bowel obstruction. Am Surg. 70:40–44. 2004.PubMed/NCBI
|
|
5
|
Firoozmand E, Fairman N, Sklar J and
Waxman K: Intravenous interleukin-6 levels predict need for
laparotomy in patients with bowel obstruction. Am Surg.
67:1145–1149. 2001.PubMed/NCBI
|
|
6
|
Hesse DG, Tracey KJ, Fong Y, Manogue KR,
Palladino MA Jr, Cerami A, Shires GT and Lowry SF: Cytokine
appearance in human endotoxemia and primate bacteremia. Surg
Gynecol Obstet. 166:147–153. 1988.PubMed/NCBI
|
|
7
|
Castell JV, Andus T, Kunz D and Heinrich
PC: Interleukin-6. The major regulator of acute-phase protein
synthesis in man and rat. Ann N Y Acad Sci. 557:87–101. 1989.
View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Jansson K, Redler B, Truedsson L, Magnuson
A, Matthiessen P, Andersson M and Norgren L: Intraperitoneal
cytokine response after major surgery: higher postoperative
intraperitoneal versus systemic cytokine levels suggest the
gastrointestinal tract as the major source of the postoperative
inflammatory reaction. Am J Surg. 187:372–377. 2004.
|
|
9
|
Herwig R, Glodny B, Kühle C, Schlüter B,
Brinkmann OA, Strasser H, Senninger N and Winde G: Early
identification of peritonitis by peritoneal cytokine measurement.
Dis Colon Rectum. 45:514–521. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Hotokezaka M, Mentis EP, Patel SP, Combs
MJ, Teates CD and Schirmer BD: Recovery of gastrointestinal tract
motility and myoelectric activity change after abdominal surgery.
Arch Surg. 132:410–417. 1997. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Artinyan A, Nunoo-Mensah JW,
Balasubramaniam S, Gauderman J, Essani R, Gonzalez-Ruiz C, Kaiser
AM and Beart RW Jr: Prolonged postoperative ileus-definition, risk
factors, and predictors after surgery. World J Surg. 32:1495–1500.
2008. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Lo OS, Law WL, Choi HK, Lee YM, Ho JW and
Seto CL: Early outcomes of surgery for small bowel obstruction:
analysis of risk factors. Langenbecks Arch Surg. 392:173–178. 2007.
View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Yamamoto T, Umegae S, Kitagawa T and
Matsumoto K: The value of plasma cytokine measurement for the
detection of strangulation in patients with bowel obstruction: a
prospective, pilot study. Dis Colon Rectum. 48:1451–1459. 2005.
View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Wiesner W, Khurana B, Ji H and Ros PR: CT
of acute bowel ischemia. Radiology. 226:635–650. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Bickell NA, Federman AD and Aufses AH Jr:
Influence of time on risk of bowel resection in complete small
bowel obstruction. J Am Coll Surg. 201:847–854. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Jeong WK, Lim SB, Choi HS and Jeong SY:
Conservative management of adhesive small bowel obstructions in
patients previously operated on for colorectal cancer. J
Gastrointest Surg. 12:926–932. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Maruna P, Frasko R and Gürlich R: Plasma
procalcitonin in patients with ileus. Relations to other
inflammatory parameters. Physiol Res. 57:481–486. 2008.PubMed/NCBI
|
|
18
|
Bertram P, Junge K, Schachtrupp A, Götze
C, Kunz D and Schumpelick V: Peritoneal release of TNFalpha and
IL-6 after elective colorectal surgery and anastomotic leakage. J
Invest Surg. 16:65–69. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Soybel DI and Zinner MJ: Ileus and the
macrophage. Ann Surg. 237:316–318. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Chachkhiani I, Gürlich R, Maruna P, Frasko
R and Lindner J: The postoperative stress response and its
reflection in cytokine network and leptin plasma levels. Physiol
Res. 54:279–285. 2005.PubMed/NCBI
|
|
21
|
Boeckxstaens GE: Neuroimmune interaction
in the gut: from bench to bedside. Verh K Acad Geneeskd Belg.
68:329–355. 2006.PubMed/NCBI
|
|
22
|
Nylen ES, O’Neill W, Jordan MH, Snider RH,
Moore CF, Lewis M, Silva OL and Becker KL: Serum procalcitonin as
an index of inhalation injury in burns. Horm Metab Res. 24:439–443.
1992. View Article : Google Scholar : PubMed/NCBI
|