Introduction
The incidence of basal cell carcinoma (BCC) is
increasing worldwide. As a result, the demand for novel and
effective treatment modalities for BCC is high (1). BCC is commonly treated with surgical
excision, curettage, carbon dioxide (CO2) laser ablation
or cryotherapy, depending on the tumor depth and the histological
subtype of the BCC. Photodynamic therapy (PDT) has been widely used
for the treatment of superficial BCC in preference to excision due
to its minimal invasiveness and satisfactory cosmetic results
(2). However, the efficacy of this
treatment modality is limited in the treatment of deeper lesions
and the more aggressive subtypes of BCC (3). Retreatment and recurrences of the
disease are frequent if the tumor depth is >2 mm. Therefore, in
order to improve the outcomes of BCC treatment, the present study
attempted to combine CO2 laser ablation with topical
methyl aminolevulinate (MAL) PDT and modified cryotherapy for the
treatment of variable BCC.
Materials and methods
Patients
In total, 8 patients (2 males and 6 females) with a
histological diagnosis of BCC (Table
I) were admitted to the Department of Dermatology, Keimyung
University Dongsan Hospital (Daegu, Republic of Korea) and included
in the present study. Written informed consent was obtained from
each patient. This study was approved by the Institutional Review
Board of Dongsan Medical Center (Daegu, Korea).
 | Table ICharacteristics of the patients
treated with carbon dioxide laser ablation in combination with
photodynamic therapy, followed by modified cryotherapy for BCC. |
Table I
Characteristics of the patients
treated with carbon dioxide laser ablation in combination with
photodynamic therapy, followed by modified cryotherapy for BCC.
| Case no. | Diagnosis | Gender | Age (years) | Location | Depth (mm) | No. of treatment
sessions | Follow up
(months) | Cosmetic outcome |
|---|
| 1 | Superficial BCC | F | 63 | Left thigh | 0.55 | 1 | 30 | PIH |
| 2 | Nodular BCC | F | 78 | Nose | 1.12 | 1 | 29 | Good |
| 3 | Nodular BCC | F | 67 | Nose | 3.75 | 1 | 30 | PIH |
| 4 | Nodular BCC | F | 77 | Right medial
canthus | 1.45 | 1 | 29 | Good |
| 5 | Nodular BCC | M | 64 | Left temple | 1.63 | 2 | 19 | PIH |
| 6 | Nodular BCC | F | 57 | Right upper lip | 2.54 | 2 | 16 | Good |
| 7 | Nodular BCC | F | 79 | Left cheek | 2.12 | 2 | 6 | Good |
| 8 | Infiltrative BCC | M | 61 | Right arm | 2.34 | 2 | 28 | Good |
Treatment methods
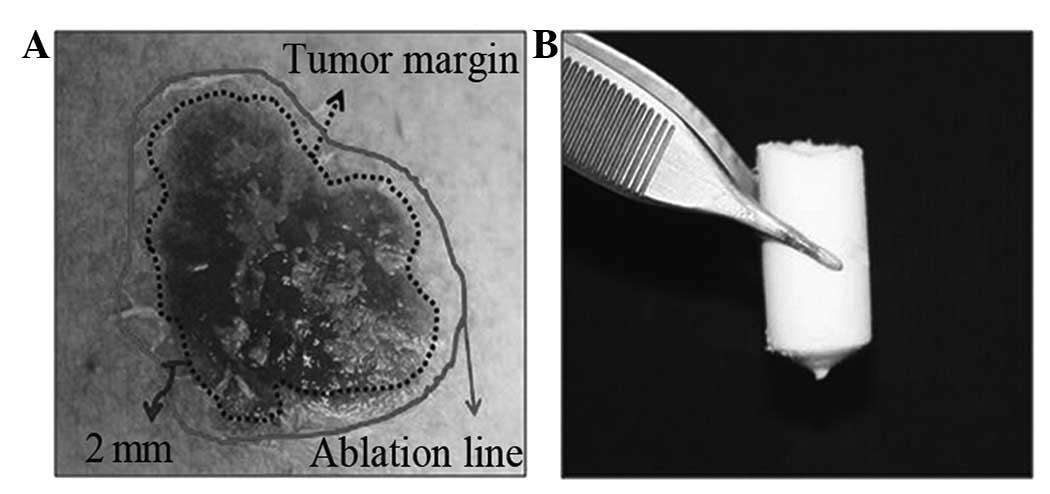
Following CO2 laser ablation with a 2 mm
margin (Fig. 1A), MAL (Metvix,
Galderma, Oslo, Norway) was applied to a thickness of 1 mm covering
the 2 mm of surrounding skin for 3 h. The lesion was then
illuminated with light-emitting diodes (LEDs; Aktilite Lamp,
Photocure ASA, Oslo, Norway) at a total intensity of 37
J/cm2 and with a distance of 7 cm from the lesion to the
light source. Following PDT, a cryostick constructed from solid
CO2 was applied to the lesion twice for 5 sec (Fig. 1B). Images of all the lesions were
obtained at baseline and then at 3 and 6 months. A skin biopsy from
the lesion was obtained to evaluate the response and to
histologically confirm complete healing.
Results
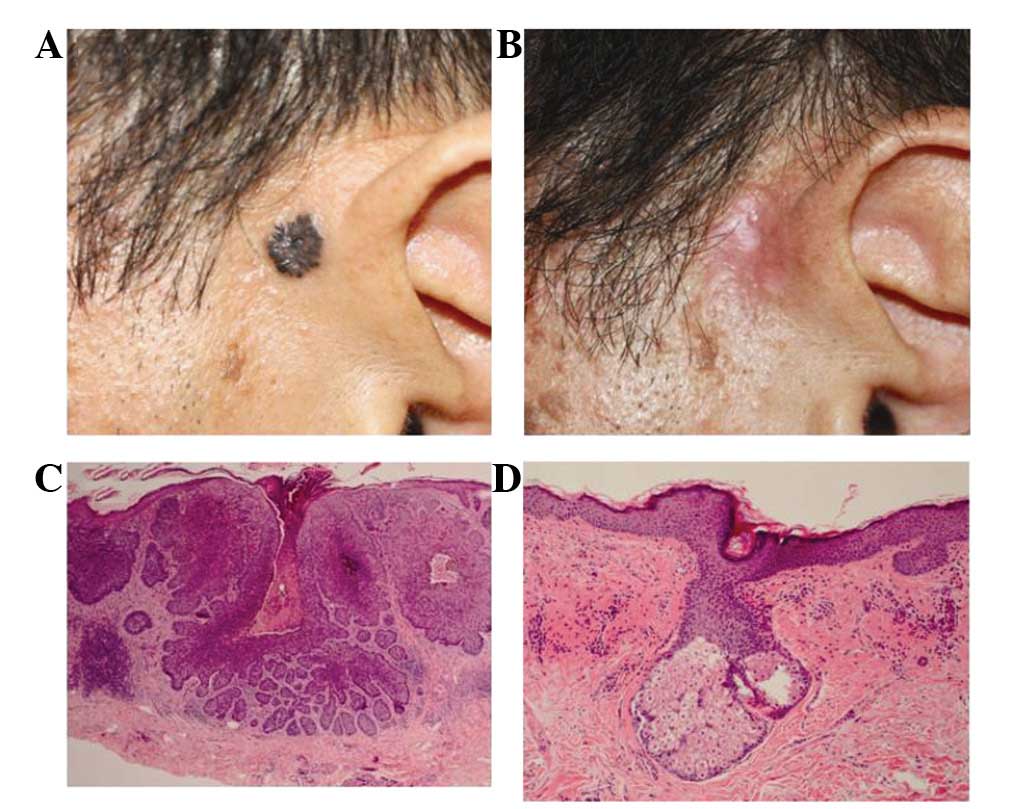
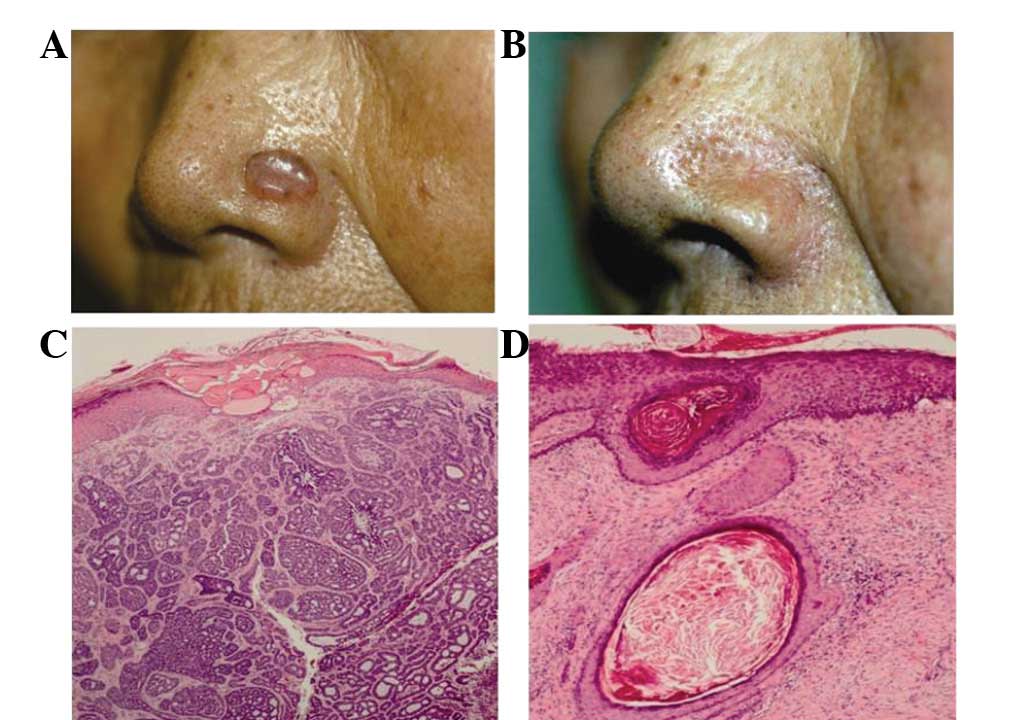
The mean age of the patients included in the study
was 68 years (range, 57–78 years). A total of 6 lesions were on the
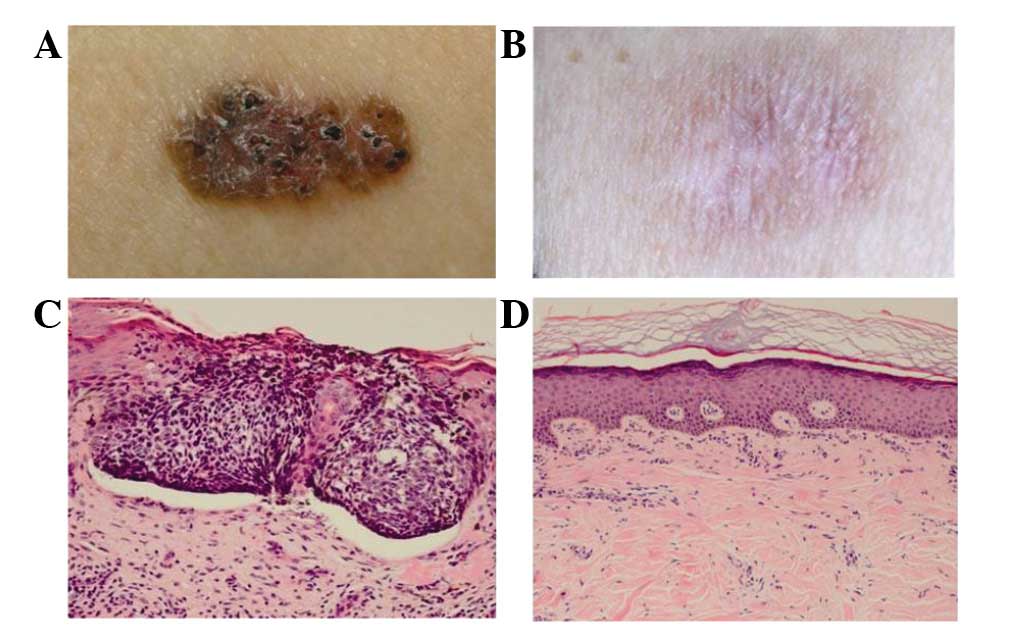
face (Figs. 2 and 3), with 1 on the thigh (Fig. 4) and 1 on the arm. The histological
subtypes of the BCC that were examined were varied, with 1
superficial, 6 nodular and 1 infiltrative (Table I). With regard to the tumor depth, 4
lesions were ≤2 mm deep and 4 lesions were >2 mm deep. The mean
follow-up period was 22 months (range, 6–30 months). During the
follow-up period, a total of 8 patients demonstrated a complete
response following treatment with CO2 laser ablation in
combination with PDT, followed by modified cryotherapy. In
addition, no recurrences of disease were observed during this
period (Figs 2 and 3). In total, 4 of the patients received 1
treatment session and 4 patients received 2 treatment sessions.
Certain patients experienced a mild burning sensation during
cryotherapy and the lesions exhibited post-inflammatory
hyperpigmentation with minimal scarring (Fig. 4).
Discussion
BCC is the most common type of skin cancer in
humans. Of all BCCs, 85% occur in the head and neck region
(4), therefore, the cosmetic
outcome is a particularly important issue in the treatment of BCC.
PDT is an effective option in the treatment of BCC due to its high
cure rate and satisfactory cosmetic outcome (5). However, the efficacy of PDT
monotherapy is limited in the treatment of deeper lesions (>2 mm
depth) and the more aggressive subtypes of BCC (3). Therefore, deep curettage provides a
favorable clinical and cosmetic short-term outcome following PDT
due to the reduction in lesion thickness (6). Thus, further treatment modalities are
required in addition to PDT for the treatment of the nodular and
aggressive subtypes of BCC. For example, Whitaker et al
reported that a combination of CO2 laser ablation and
PDT plays a synergistic role in the treatment of nodular BCC
(7).
In the present study, the data demonstrated that a
combination of CO2 laser ablation and topical MAL PDT,
followed by modified cryotherapy provided an effective method for
the treatment of nodular and superficial BCC. Patients diagnosed
with nodular BCC were completely healed with treated lesions
exhibiting minimal hyperpigmentation and no scarring. This combined
therapy was generally well tolerated in the patients, with the
exception of certain patients who experienced a transient burning
pain and erythema.
In the topical treatment of the deep, nodular and
infiltrative subtypes of BCC using PDT, the delivery of sufficient
photosensitizer and light to the full depth of the lesion is
critical. The usage of CO2 laser ablation is beneficial
since it removes the upper component of the BCC, thus potentially
enhancing the penetrating depth of PDT and maximizing the efficacy
of the treatment.
Conventional cryotherapy following PDT additionally
kills the remaining cancer cells by interrupting vital metabolic
cycles, destabilizing cell membranes, creating an adverse
hyperosmolar environment and forming water crystals (8). In the present study, a solid cryostick
was applied to the PDT lesion twice for 5 sec. The benefits of this
modified form of cryotherapy include its ability to trigger a
specific T lymphocyte response and to increase the activity of
natural killer cells by releasing tumor antigens and inflammatory
mediators. Thus, the application of a cryostick led to
immunomodulation rather than the death of the tumor cells. Due to
these synergistic effects, the present study demonstrated that this
combination treatment was efficacious in the treatment of nodular
and infiltrative subtypes of BCC, even when the tumor depth was
>2 mm.
To the best of our knowledge, this is the first
study to report the successful treatment of nodular BCC with a
combination of CO2 laser ablation and PDT, followed by
modified cryotherapy. We suggest that CO2 laser ablation
in combination with PDT, followed by modified cryotherapy is a
potential treatment option for nodular BCC.
References
|
1
|
Arits AH, Schlangen MH, Nelemans PJ and
Kelleners-Smeets NW: Trends in the incidence of basal cell
carcinoma by histopathological subtype. J Eur Acad Dermatol
Venereol. 25:565–569. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Szeimies RM, Ibbotson S, Murrell DF, et
al: A clinical study comparing methyl aminolevulinate photodynamic
therapy and surgery in small superficial basal cell carcinoma (8–20
mm), with a 12-month follow-up. J Eur Acad Dermatol Venereol.
22:1302–1311. 2008.PubMed/NCBI
|
|
3
|
Fantini F, Greco A, Del Giovane C, et al:
Photodynamic therapy for basal cell carcinoma: clinical and
pathological determinants of response. J Eur Acad Dermatol
Venereol. 25:896–901. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Miller SJ: Biology of basal cell carcinoma
(Part I). J Am Acad Dermatol. 24:1–13. 1991. View Article : Google Scholar
|
|
5
|
Rhodes LE, de Rie M, Enström Y, et al:
Photodynamic therapy using topical methyl aminolevulinate vs
surgery for nodular basal cell carcinoma: results of a multicenter
randomized prospective trial. Arch Dermatol. 140:17–23. 2004.
View Article : Google Scholar
|
|
6
|
Christensen E, Mørk C and Foss OA:
Pre-treatment deep curettage can significantly reduce tumour
thickness in thick Basal cell carcinoma while maintaining a
favourable cosmetic outcome when used in combination with topical
photodynamic therapy. J Skin Cancer. 2011:2403402011. View Article : Google Scholar
|
|
7
|
Whitaker IS, Shokrollahi K, James W,
Mishra A, Lohana P and Murison MC: Combined CO(2) laser with
photodynamic therapy for the treatment of nodular basal cell
carcinomas. Ann Plast Surg. 59:484–488. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Messeguer F, Serra-Guillen C, Echeverria
B, et al: A pilot study of clinical efficacy of imiquimod and
cryotherapy for the treatment of basal cell carcinoma with
incomplete response to imiquimod. J Eur Acad Dermatol Venereol.
26:879–881. 2012. View Article : Google Scholar : PubMed/NCBI
|