Introduction
Although rare, ethmoid adenocarcinoma is the most
frequent ethmoid tumor. Chronic exposure to wood dust is a risk
factor for its development (1,2).
Progression is generally locoregional with invasion of adjacent
structures, including the orbits, skull base, dura mater and brain.
The prognosis of this malignancy is dependent on the extent of the
disease at the time of diagnosis (3–6).
Distant metastasis via the leptomeninges, metastasis to the neck
nodes and hematogenous metastasis to distant organs have been
reported (7–12). New neurological deficits due to
metastasis are extremely rare and are usually an expression of
leptomeningeal dissemination (10–16).
The current case report presents a rare case of spinal cord
compression due to vertebroepidural metastasis of an ethmoid
adenocarcinoma. Written informed consent was obtained from the
patient.
Case report
Clinical presentation and diagnosis of
cancer
A 70-year-old male, who had previously been a
carpenter for 43 years, presented with a 4-month history of
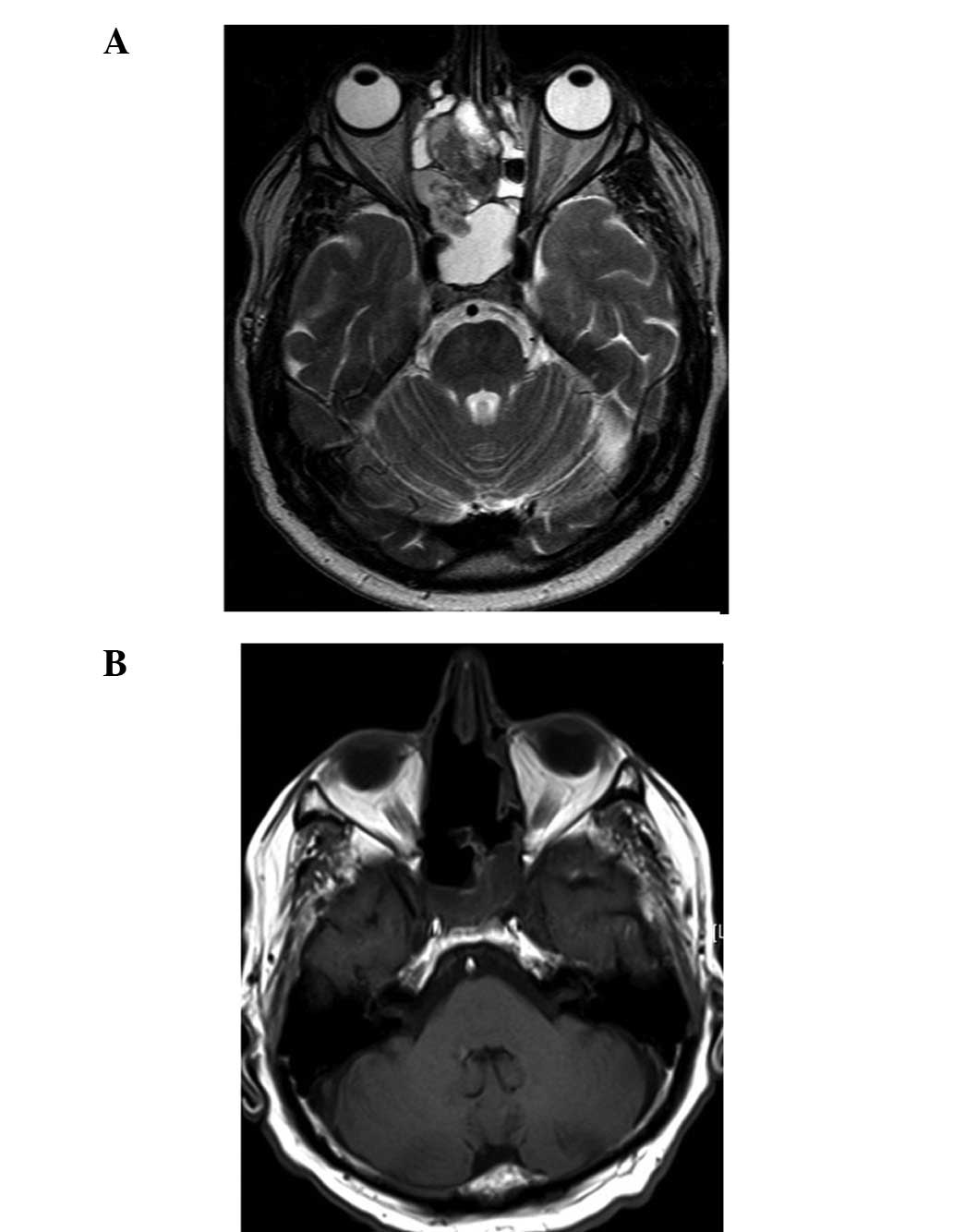
headaches with epistaxis. Enhanced head CT and MRI scans revealed a
right ethmoid tumor with dural invasion (T4bN0M0 in Roux
classification; Fig. 1A) (4,6). A
transnasal biopsy confirmed the diagnosis of an adenocarcinoma,
which was subsequently resected through a right paralateronasal
approach by a multidisciplinary team, including a neurosurgeon and
ENT surgeon (Fig. 1B). The
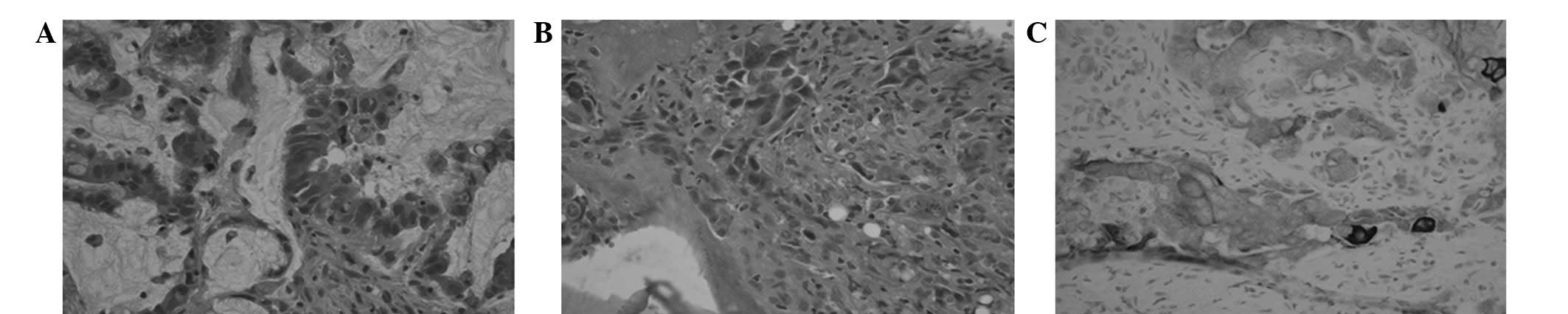
histology of the primary lesion revealed an ethmoid adenocarcinoma,
mucinous variant (Fig. 4A),
expressing cytokeratin 20 (CK20) and partially expressing CK7.
Treatment and clinical course
The patient underwent post-operative
intensity-modulated radiation therapy (60 Gy to the target volume).
Two months later, the patient was admitted to the emergency
department with an acute onset of the inability to empty the
bladder. In addition, the patient reported severe dorsal pain and
progressive lower limb weakness and numbness. A physical
examination revealed unexplained weight loss and lower extremity
weakness (3/5) to the point where the individual was no longer
mobile. Proprioception and sensation to pain and temperature were
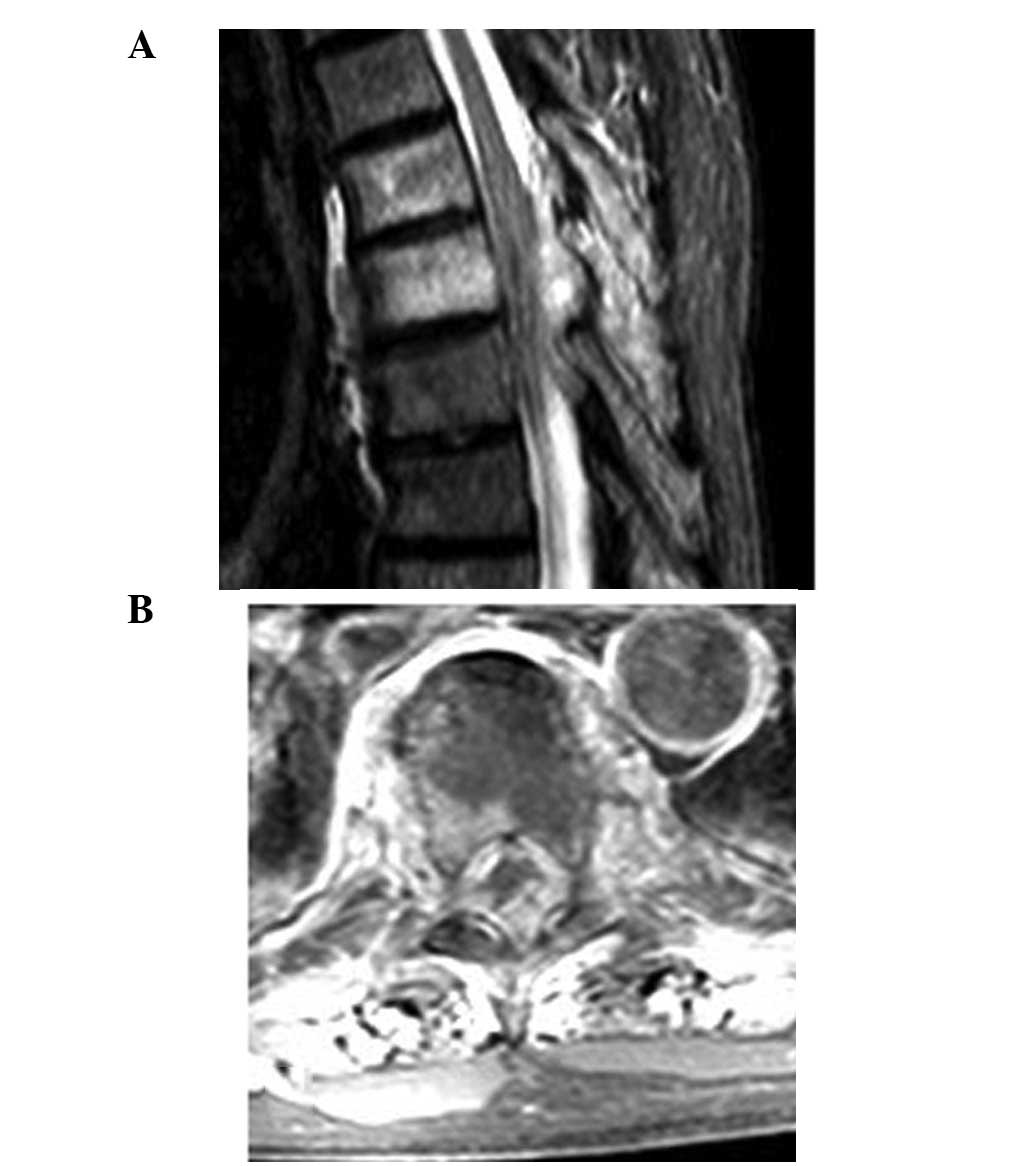
diminished from the xiphoid process downward. Gadolinium-enhanced
T1- and T2-weighted MRI scans revealed abnormal bone marrow signal
enhancement at T5 and T6 (Fig. 2A)
that was associated with an epidural mass that was encasing and
severely compressing the spinal cord at T6-T8 (Fig. 2B). In addition,
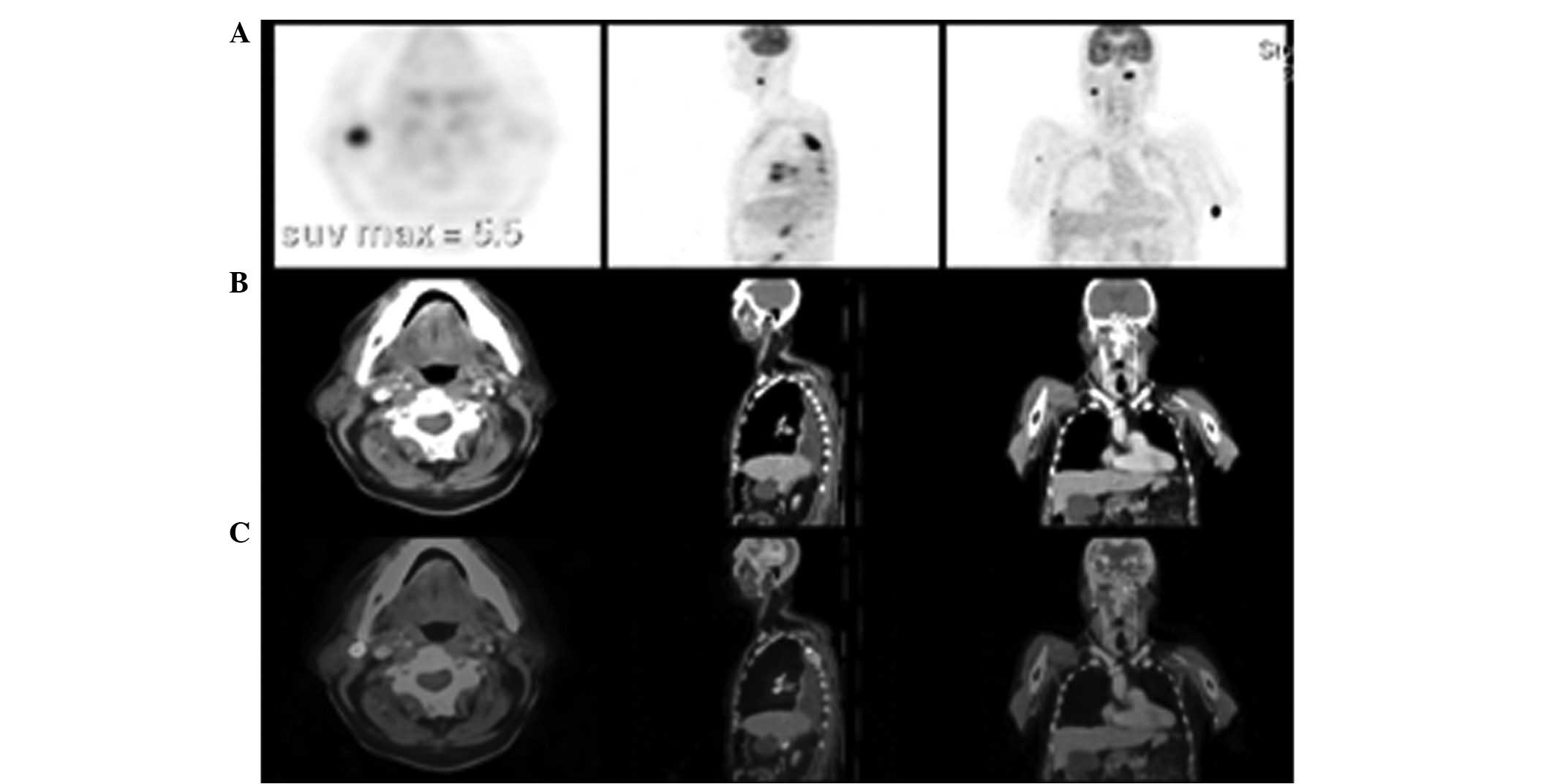
18F-fludeoxyglucose-positron emission tomography
(18FDG-PET) revealed diffuse metastatic dissemination to
the spine, the hilar, mediastinal and peritoneal lymph nodes, the
right parotid gland, the right gluteus, the lungs and each adrenal
gland (Fig. 3). By contrast, there
was no significant local hyperfixation, and a gadolinium-enhanced
brain MRI excluded locoregional recurrence and dural or brain
extension. A decompressive laminectomy and vertebroplasty were
performed and post-operative standard beam external radiotherapy
(48 Gy) was administered. This allowed for the partial remission of
pain, but no sensorimotor improvement. Following 6 weeks of
palliative and supportive care, the patient succumbed to his
condition. Histological and immunohistochemical studies confirmed
the diagnosis of epidural metastasis of an adenocarcinoma (Fig. 4B). Compared with the primary tumor,
the metastatic lesion was dedifferentiated, demonstrating a partial
expression of CK20 and no CK7 (Fig.
4C).
Discussion
Although rare, ethmoid adenocarcinomas account for
>50% of malignancies involving the ethmoid sinuses and ~15% of
all sinonasal malignancies (2,7). Their
progression is often locoregional with extension into the sinonasal
cavities, orbit and eventually the intracranial compartment
following infiltration of the dura mater. Meningeal extension (T4b
in Roux classification) is associated with poor prognosis (3,4).
Distant metastases are identified in 6–30% of cases
and are more often cerebromeningeal and osseous rather than
visceral and ganglionic (1,3,4,8).
Metastasis usually becomes evident between 13 and 19 months after
the diagnosis of the primary tumor, although in certain cases
metastases have been found as early as 2 months and as late as 42
months (3,9). Metastases may even occur in the
absence of local relapse (3,8).
Leptomeningeal carcinomatosis, with or without compressive
epiduritis, has been reported in a number of case studies to be
responsible for neurological impairment (9,10). The
clinical outlook is variable and may include cauda equina syndrome
(10,14), multiple involvement of the cranial
and spinal nerves (3,11,12)
and brain (8) or, extremely rarely,
spinal cord dysfunction (13). The
current study presents a case of spinal cord compression due to
vertebroepidural metastasis of an ethmoid adenocarcinoma, which is,
to the best of our knowledge, the second case described thus far
(13). The present case is more
recent and was examined pre-operatively by modern imaging studies,
including MRI and 18FDG-PET, instead of myelography. In
addition, histological and immunohistochemical analyses were
performed, which are key tools for diagnosis. The histology of the
primary lesion revealed an ethmoid adenocarcinoma, mucinous
variant, that was expressing CK20 and partially expressing CK7.
Compared with the primary tumor, the metastatic lesion was
dedifferentiated, revealing a partial expression of CK20 and no
CK7, which is not a rare observation (14). The expression of cytokeratins may
indicate colonic, gastric or prostatic adenocarcinoma as a primary
tumor, which more frequently leads to vertebroepidural metastasis
rather than ethmoid adenocarcinomas (14). These observations indicated that an
in-depth investigation was required for other forms of cancer,
which were excluded in the present case by whole-body CT and PET
scans and normal PSA levels.
Leptomeningeal seeding of ethmoid adenocarcinomas
may be hematogenous, driven by cerebrospinal fluid (CSF) flow or
occur through perivascular and perineural lymphatics (9,11,15).
Seeding appears to occur more often when the tumor invades the
intracranial compartment, as was consistent with observations of
the current study and of previous cases involving the surgical
opening of the dura mater (9,11,15).
However, there is no clear correlation between tumor extension and
the risk of leptomeningeal spread due to an insufficient number of
studies on this area at present (3,8). Two
mechanisms of invasion may be possible in the present case, namely
via the CSF or the bloodstream. The short delay between the initial
surgery and the diagnosis of vertebroepidural metastasis may
support the first mechanism if the surgery had a favorable effect.
However, metastasis may have already been present as pre-operative
spinal MRI was not performed prior to the initial surgery. By
contrast, multiple vertebral and systemic involvement supports the
hematogenous mechanism.
These observations indicate the current issues
associated with the initial management of patients affected by T4b
tumors, and the rarity of cases explains the lack of available
guidelines. Wen et al recommended a systemic search for
tumoral cells within the CSF prior to radical surgery to exclude
iatrogenic dissemination (7).
However, spinal tap sensitivity is only 50% and increases to 90% if
repeated twice (11).
Gadolinium-enhanced spinal MRI is the most reliable diagnostic
method for the identification of vertebroepidural metastasis,
although it does not always reveal leptomeningeal dissemination
(9). Despite the rarity of spinal
leptomeningeal metastasis of ethmoid adenocarcinomas, the use of
lumbar punctures and particularly gadolinium-enhanced spinal MRI,
may be indicated prior to and following surgery in cases of T4b
tumors. These procedures may also be recommended for more localized
forms in cases of inadvertent intraoperative opening of the dura
mater. Due to the possibility of late hematogenous dissemination, a
quarterly gadolinium-enhanced spinal MRI would be suitable.
However, at present, the prognosis of metastasis is extremely poor,
particularly in cases of leptomeningeal dissemination, and survival
times vary between 2 and 12 months following a diagnosis of
secondary localization (1,4,7,16).
In conclusion, vertebroepidural metastasis of
ethmoid carcinoma, although rare, must not be disregarded. Initial
intradural extension may favor the onset of metastasis and justify
a systematic search for neoplastic cells in the CSF and the
performance of pre-operative and post-operative gadolinium-enhanced
spinal MRI. Histological and immunohistochemical analyses are
important for the differential diagnosis of more frequently
occurring tumors and allow for establishment of a firm diagnosis.
The prognosis of this type of metastasis is poor and depends more
on the diffusion of the disease than on local recurrence. Due to
current improvements in survival associated with the primary tumor,
the incidence of spinal metastasis of ethmoid adenocarcinomas is
likely to increase in frequency in the near future, therefore
requiring appropriate diagnostic and therapeutic management.
References
|
1
|
de Gabory L, Maunoury A, Maurice-Tison S,
Merza Abdulkhaleq H, Darrouzet V, Bébéar JP and Stoll D: Long-term
single-center results of management of ethmoid adenocarcinoma: 95
patients over 28 years. Ann Surg Oncol. 17:1127–1134.
2010.PubMed/NCBI
|
|
2
|
Fontana L, Liétin B, Catilina P, Devif C,
Féneon B, Martin F, Mom T and Gilain L: Occupational exposure to
wood dust and nasal sinus cancer. Ann Otolaryngol Chir Cervicofac.
125:65–71. 2008.(In French).
|
|
3
|
Moreau JJ, Bessede JP, Heurtebise F,
Moufid A, Veysset P, Sauvage JP, Rhein B and Roullet B:
Adenocarcinoma of the ethmoid sinus in woodworkers. Retrospective
study of 25 cases. Neurochirurgie. 43:111–117. 1997.(In
French).
|
|
4
|
Roux FX, Pages JC, Nataf F, Devaux B,
Laccourreye O, Menard M and Brasnu D: Malignant ethmoid-sphenoidal
tumors. 130 cases. Retrospective study. Neurochirurgie. 43:100–110.
1997.(In French).
|
|
5
|
Stoll D, Bébéar JP, Truilhé Y, Darrouzet V
and David N: Ethmoid adenocarcinomas: retrospective study of 76
patients. Rev Laryngol Otol Rhinol (Bord). 122:21–29.
2001.PubMed/NCBI
|
|
6
|
Vieillot S, Boisselier P, Aillères N, Hay
MH, Dubois JB, Azria D and Fenoglietto P: Paranasal sinus
carcinoma. Cancer Radiother. 14(Suppl 1): S52–S60. 2010.(In
French).
|
|
7
|
Wen BC, Hussey DH, Clamon GH and Godersky
JC: Leptomeningeal carcinomatosis following craniofacial resection
of an ethmoid tumor. J Surg Oncol. 49:266–269. 1992. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
George B, Salvan D, Luboinski B,
Boissonnet H and Lot G: Malignant tumors of the ethmoid sinuses. A
homogenous series of 41 cases operated on by mixed approaches.
Neurochirurgie. 43:121–124. 1997.(In French).
|
|
9
|
Herrlinger U, Förschlera H, Kükerb W,
Meyermann R, Bamberg M, Dichgans J and Weller M: Leptomeningeal
metastasis: survival and prognostic factors in 155 patients. J
Neurol Sci. 223:167–178. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Newton P and Grennan DM: Ethmoid sinus
carcinoma metastasising to the cauda equina: a case report. J
Neurol Neurosurg Psychiatry. 46:585–586. 1983. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Béjot Y, Catteau A, Hervieu M, Giré P,
Caillier M, Bénatru I, Osseby GV, Soichot P, Moreau T and Giroud M:
Leptomeningeal dissemination after ethmoidal sinus adenocarcinoma
surgery: a rare complication. Rev Neurol (Paris). 164:189–193.
2008.(In French).
|
|
12
|
Rogowski J, Fosse S, Dupont J, Poitou L,
Valo I and Simon de Kergunic JPS: Adenocarcinoma of the ethmoid
with meningeal carcinomatosis. Presse Med. 40:209–211. 2011.(In
French).
|
|
13
|
Johns DR and Sweriduk ST: Spinal cord
compression due to ethmoid adenocarcinoma. Cancer. 60:1863–1865.
1987. View Article : Google Scholar
|
|
14
|
Wang NP, Zee S, Zarbo RJ, Bacchi CE and
Gown AM: Coordinate expression of cytokeratins 7 and 20 defines
unique subsets of carcinomas. Appl Immunohistochem. 3:99–107.
1995.
|
|
15
|
Baron MP, Cyteval C, Thomas E, Leroux JL,
Blotman F and Lamarque JL: Cauda equina syndrome disclosing
adenocarcinoma of the ethmoid. J Radiol. 74:363–365. 1993.(In
French).
|
|
16
|
Vellin JF, Achim V, Sinardet D,
Gabrillargues J, Mom T and Gilain L: Rapidly developing
leptomeningeal carcinomatosis following anterior skull base
surgery: a case report. Auris Nasus Larynx. 34:565–567. 2007.
View Article : Google Scholar : PubMed/NCBI
|