Introduction
The benefit of a multidisciplinary approach in head
and neck cancer patients was demonstrated by a phase III trial from
the UK that was published in the late nineties. In this trial, 350
T2-T4 N0-N2 oral cavity or oropharynx cancer patients were
randomized to either undergo surgery and post-operative conformal
radiotherapy or irradiation alone. The trial was closed early, as a
significant difference in favor of the combined treatment arm was
noted at 23 months for overall survival, cause-specific survival
and local control (1). In head and
neck cancers that are associated with high-risk factors, including
lymph node involvement with extracapsular extension (ECE),
post-operative radiochemotherapy is mandatory.
However, post-operative 3D conformal radiotherapy
(3D-CRT) has certain limitations, including xerostomia, mandible
necrosis and trismus. These toxicities may be reduced by using
intensity-modulated radiotherapy (IMRT) (2–4).
Furthermore, repeated computed tomography (CT) scans
may be performed during the course of radiotherapy directly in the
treatment room in order to optimize the position of the patient
prior to administering IMRT [image-guided radiation therapy
(IGRT)]. Therefore, potential losses in the local control due to
missing the target may be avoided (5,6).
The present case is an example of how IGRT allows a
safe dose delivery of highly conformal treatment plans for rare
patient setups in head and neck radiotherapy. Written informed
consent was obtained from the patient’s family.
Case report
Presentation
A 71-year-old male, with a body weight of 50 kg and
a height of 1.62 m, presented with a visible superficial ulcer with
poorly-defined margins on the right side of the tongue. The patient
complained of oral pain and dysphagia that had lasted for several
months. The patient had a history of drinking 1 beer/day and a
smoking history of 30 pack years. The past medical history included
heavy chronic obstructive pulmonary disease (COPD), pulmonary
tuberculosis, arterial hypertension, peripheral arterial occlusive
disease with bilateral stenosis of the internal carotid arteries
and liver cirrhosis. The biopsy revealed a poorly-differentiated
squamous cell carcinoma of the floor of the mouth.
Treatment
The surgery involved a tracheotomy to assure the
airways remained open and a dissection of levels I–IV on the right
side and I–III on the left side of the neck. A radical surgical
tumor excision and reconstruction, with a microvascular anastomosed
free flap from the anterolateral thigh (ALT), was then performed.
Due to continued heavy tracheal secretion as a result of severe
COPD, the tracheal cannula was not removed.
The definitive tumor-node-metastasis (TNM) status
was pT2 (2.5 cm) pN2b (3/39 with extracapsular extension) G3 Pn1 L0
V0 R0 (≥0.2 cm to the floor of the mouth, ≥1 cm to all the other
sites). The multidisciplinary head and neck tumor board recommended
adjuvant therapy. Prior to adjuvant therapy, the patient underwent
a percutaneous endoscopic gastrostomy (PEG). Every time the patient
was placed in the supine position during the radiotherapy setup,
the patient experienced severe coughing attacks. No coughing was
observed while sitting or lying on the side in a lateral position.
Several changes of the tracheal cannula did not improve the
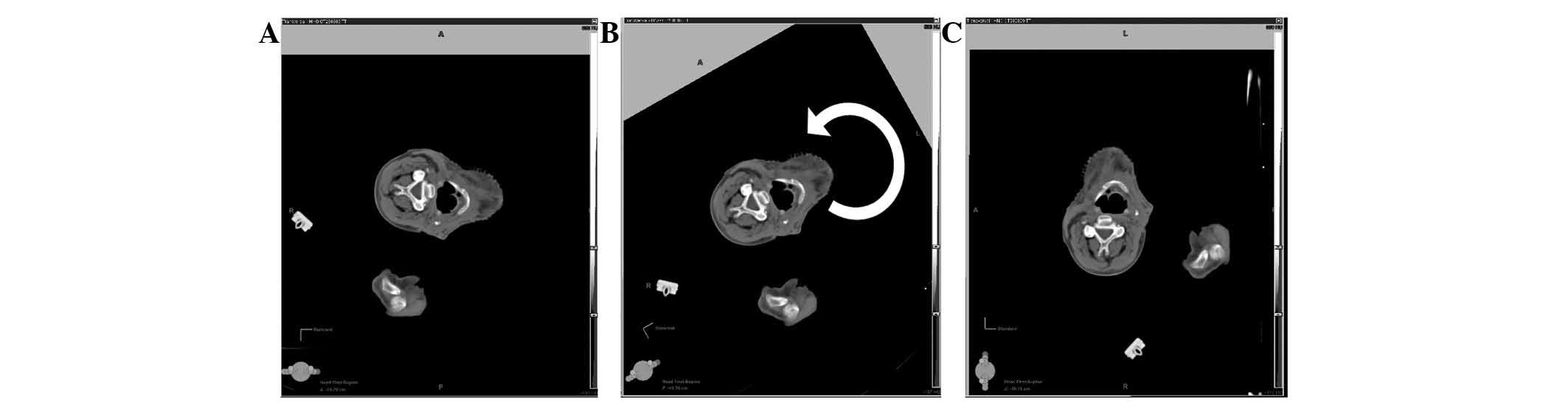
coughing. A lateral position was decided upon (Fig. 1) utilizing a head mask and a vacuum
cushion (BodyFIX; Medical Intelligence, Schwabmünchen,
Germany).
Due to the age of the patient, comorbidities and
insufficient renal function (clearance 47 ml/min), no
platinum-based chemotherapy was administered.
Results
In order to contour the planning target volume
(PTV), software was required that allowed the rotation of the CT
images at 90 degrees to the normal view that radiation oncologists
are used to while contouring (Fig.
2). The contouring was performed using Eclipse (Varian Medical
Systems, Palo Alto, CA, USA). The tumor clinical target volume
(CTV) was defined as the gross tumor volume (GTV) delineated on a
pre-operative CT, including the visible post-operative changes on
the post-operative CT plus a safety margin of 10 mm. The elective
nodal-CTV was defined according to the literature (7,8).
In-ward radiotherapy was performed using a
TomoTherapy machine (Accuray Incorporated, Sunnyvale, CA, USA).
Daily image guidance (IG) was performed using an incorporated
mega-voltage CT (MVCT). The overall treatment time was 6.5 weeks.
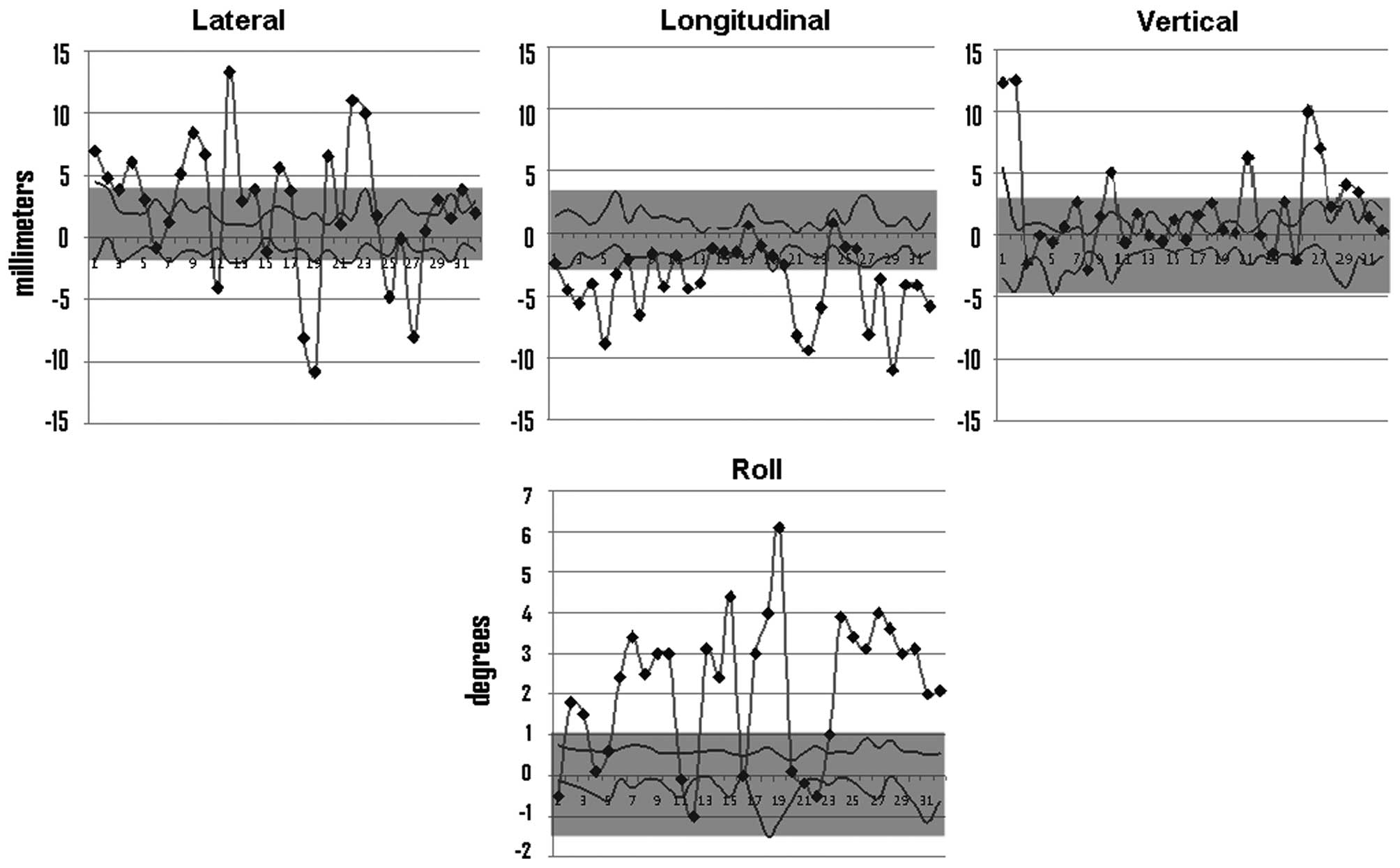
The daily setup errors in the translational directions and the
rotational direction (roll) are presented in Fig. 3.
The patient tolerated the treatment well. At the end
of the radiotherapy, the patient presented with Common Terminology
Criteria for Adverse Events (CTCAE) grade 3 mucositis and CTCAE
grade 1 dermatitis. A combined PEG-oral food intake was possible
during the entire treatment time.
Follow-up
The patient underwent regular follow-up sessions
every three months. Seven months after the surgery, the patient had
experienced no more problems with deglutition and the tracheotomy
was closed. At nine months after radiotherapy, the patient had no
xerostomia, no swallowing dysfunction, localized submental edema,
mild voice alteration and moderate skin induration. However, the CT
revealed a tumor recurrence at the floor of the mouth, which was
histologically proven.
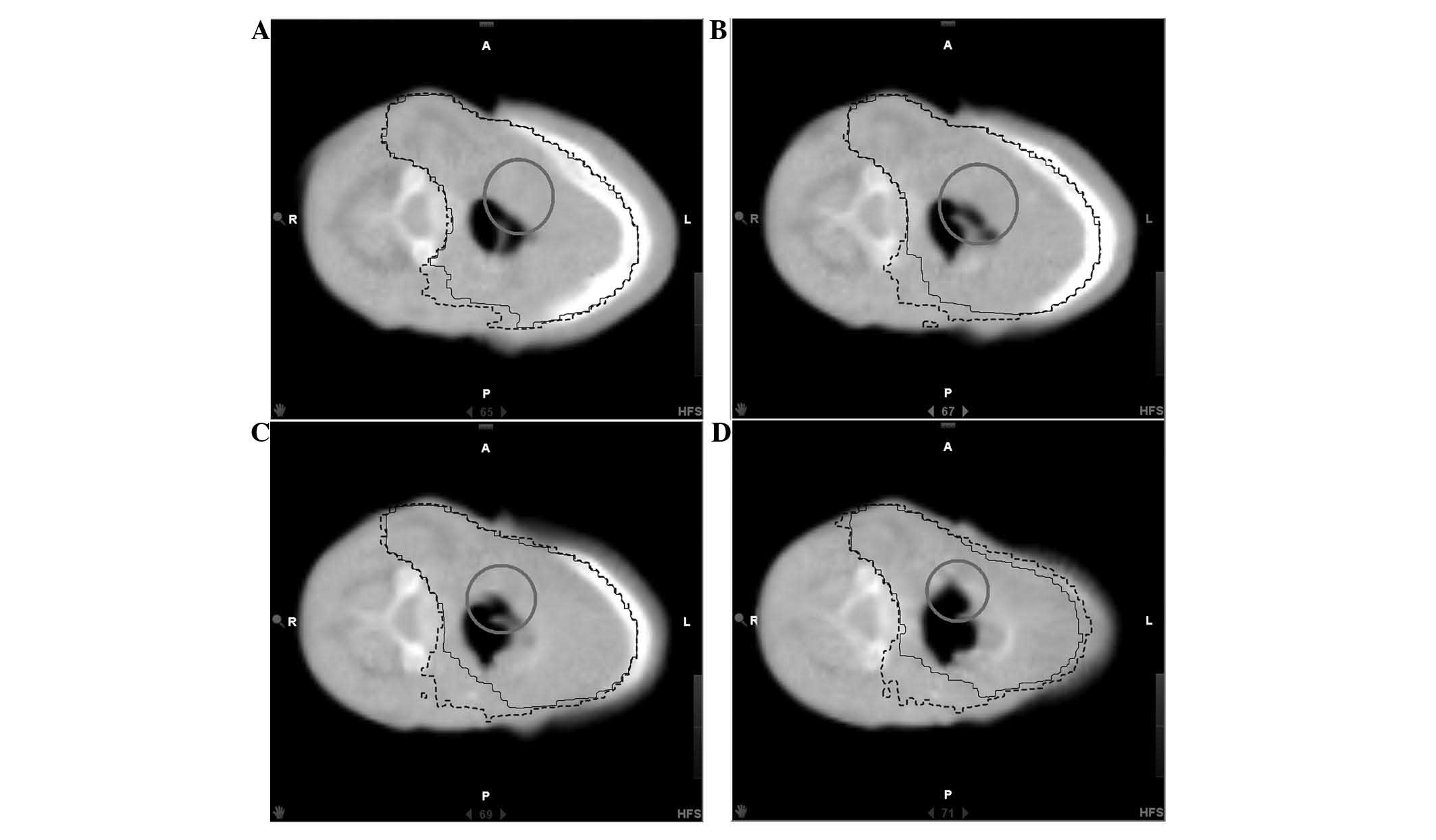
An evaluation of the planned dose was insufficient
in this case. An assessment of the impact of setup and soft tissue
shrinkage on the actual daily delivered dose was necessary.
Therefore, retrospective recalculations of the doses were performed
on each of the 32 daily MVCTs. All the daily doses were summed up
(9). Fig. 4 depicts the actual delivered 95%
isodose on the last MVCT. The recurrence was localized in field,
within the 95% isodose.
The multidisciplinary head and neck board
recommended palliative chemotherapy, however the patient succumbed
due to tumor bleeding prior to the start of chemotherapy.
Discussion
The present case is an example of how novel
radiotherapy techniques may be used to enhance head and neck
oncological treatment.
Due to severe coughing attacks that were caused by
the supine position, the patient in the present study was not able
to be treated in the standard supine position. Several options were
discussed, including not performing radiotherapy treatment at all
or choosing a prone or lateral positioning for radiotherapy. Due to
the high-risk tumor constellation, a local treatment was considered
necessary. However, few immobilization devices are available that
allow a mask fixation in an alternative position to the supine one.
There is a mask system available for craniospinal irradiation that
permits a prone position with a head mask (10), however, the use of a prone position
is not possible with a patient with a PEG, as they are consequently
not able to lie on their abdomen.
Therefore, an individualized, lateral position was
chosen. The lateral position, though tolerated well by the patient,
raised several problems with regard to the reproducibility of the
setup. The lateral position is more unstable than the supine
position (11). Thus, there was a
risk of inadvertently delivering a high dose to healthy tissue.
Therefore, the options were either to deliver a lower dose to the
PTV by 3D-CRT, with a lower probability of achieving local control,
or to deliver the standard dose with an increased risk of toxicity.
IMRT is known to reduce toxicity (3,4)
without compromising the dose to the target volumes. Taking the
high-risk situation into account and the importance of adjuvant
treatment, IMRT (helical tomotherapy) was performed with
delineation and dose prescription according to the available
guidelines for standard supine head and neck treatment (7,8). Daily
CT-guided IGRT was performed in order to ensure the reproducibility
of setup.
The setup errors for this patient (Fig. 3) were higher than the reported setup
errors for the supine position in head and neck radiotherapy, which
are normally within 2–4 mm (12,13).
Thus, the decision to treat such a patient with IMRT without daily
IGRT would have been risky.
The combination of IMRT with daily IGRT translated
into low toxicities at the follow-up appointments. No xerostomia or
swallowing dysfunction and only a mild submental edema were
observed.
However, the tumor recurred. The question was raised
as to whether the setup uncertainties, although compensated by
daily CT-IGRT, in combination with the steep dose gradients of
helical tomotherapy may have caused an underdosage of the planning
target regions. A simple correlation of the recurrence site with
the dose on the planning CT would have been incomplete for several
reasons. Firstly, the patient may have had a slight alternative
position during radiotherapy compared with the planning CT.
Secondly, head and neck patients often undergo soft tissue changes
during radiotherapy (5).
Generally, if it may be assumed that patients are
rigid bodies, setup uncertainties may be perfectly compensated for
by daily IGRT. However, deformations of organs occur during
fractionated radiotherapy, including a slightly varied curvature of
the spinal cord, an alternative position of the chin and shoulders
and/or shrinkage of the soft tissues. A perfect alignment, in which
the organs lie exactly in the same position as during the planning
CT and thus the delivered dose is exactly the same as the
calculated dose on the planning CT, is not feasible.
In order to determine the impact of interfractional
uncertainties and of soft tissue deformations on the delivered
dose, the actual delivered dose was recalculated on every daily
MVCT and all the daily delivered doses were summed up. The summed
dose was not completely accurate, as non-rigid registration was not
used. However, the dose represented an approximation of the actual
delivered dose. The recurrence was localized in-field, within the
95% actual delivered isodose (Fig.
4). This is consistent with other studies on the recurrence
sites of head and neck tumors in association with the isodoses on
the planning CT (14). Thus,
lateral positioning with daily-corrected setup errors did not
jeopardize the accurate delivery of the dose to the target
volume.
In selected cases of patients with head and neck
cancers who are unable to tolerate the supine position, lateral
positioning and high precision treatment is possible using daily
IGRT.
References
|
1
|
Robertson AG, Soutar DS, Paul J, et al:
Early closure of a randomized trial: surgery and postoperative
radiotherapy versus radiotherapy in the management of intra-oral
tumours. Clin Oncol (R Coll Radiol). 10:155–160. 1998. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Daly ME, Lieskovsky Y, Pawlicki T, et al:
Evaluation of patterns of failure and subjective salivary function
in patients treated with intensity modulated radiotherapy for head
and neck squamous cell carcinoma. Head Neck. 29:211–220. 2007.
View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Studer G, Studer SP, Zwahlen RA, et al:
Osteoradionecrosis of the mandible: minimized risk profile
following intensity-modulated radiation therapy (IMRT).
Strahlenther Onkol. 182:283–288. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Eisbruch A, Kim HM, Terrell JE, Marsh LH,
Dawson LA and Ship JA: Xerostomia and its predictors following
parotid-sparing irradiation of head-and-neck cancer. Int J Radiat
Oncol Biol Phys. 50:695–704. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Duma MN, Kampfer S, Wilkens JJ, Schuster
T, Molls M and Geinitz H: Comparative analysis of an image-guided
versus a non-image-guided setup approach in terms of delivered dose
to the parotid glands in head-and-neck cancer IMRT. Int J Radiat
Oncol Biol Phys. 77:1266–1273. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Chen AM, Cheng S, Farwell DG, et al:
Utility of daily image guidance with intensity-modulated
radiotherapy for tumors of the base of skull. Head Neck.
34:763–770. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Chao KS, Wippold FJ, Ozyigit G, Tran BN
and Dempsey JF: Determination and delineation of nodal target
volumes for head-and-neck cancer based on patterns of failure in
patients receiving definitive and postoperative IMRT. Int J Radiat
Oncol Biol Phys. 53:1174–1184. 2002.PubMed/NCBI
|
|
8
|
Grégoire V, Eisbruch A, Hamoir M and
Levendag P: Proposal for the delineation of the nodal CTV in the
node-positive and the post-operative neck. Radiother Oncol.
79:15–20. 2006.PubMed/NCBI
|
|
9
|
Orban de Xivry J, Castadot P, Janssens G,
et al: Evaluation of the radiobiological impact of anatomic
modifications during radiation therapy for head and neck cancer:
can we simply summate the dose? Radiother Oncol. 96:131–138.
2010.PubMed/NCBI
|
|
10
|
Rades D, Holtzhauer R, Baumann R, Leuwer M
and Karstens JH: Craniospinal axis irradiation in children.
Treatment in supine position including field verification as a
prerequisite for anesthesia without intubation. Strahlenther Onkol.
175:409–412. 1999.
|
|
11
|
Marks JE and Haus AG: The effect of
immobilisation on localisation error in the radiotherapy of head
and neck cancer. Clin Radiol. 27:175–177. 1976. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Schubert LK, Westerly DC, Tomé WA, et al:
A comprehensive assessment by tumor site of patient setup using
daily MVCT imaging from more than 3,800 helical tomotherapy
treatments. Int J Radiat Oncol Biol Phys. 73:1260–1269. 2009.
View Article : Google Scholar
|
|
13
|
Gilbeau L, Octave-Prignot M, Loncol T,
Renard L, Scalliet P and Grégoire V: Comparison of setup accuracy
of three different thermoplastic masks for the treatment of brain
and head and neck tumors. Radiother Oncol. 58:155–162. 2001.
View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Chen AM, Jennelle RL, Sreeraman R, et al:
Initial clinical experience with helical tomotherapy for head and
neck cancer. Head Neck. 31:1571–1578. 2009. View Article : Google Scholar : PubMed/NCBI
|