Introduction
Multiple primary neoplasms are defined as cases of
two or more simultaneous abnormal growths of tissue, which are
presumed to be of separate origin in one person. The neoplasms may
be histologically similar or different and may be identified in the
same or different sites (1). With
the improvement of diagnostic techniques, the progressive
lengthening of life expectancy and the increased long-term survival
of patients with malignancy, there have recently been an
subsequently increasing number of patients diagnosed with multiple
primary neoplasms.
Osteoclastoma and anaplastic astrocytoma are
relatively common malignant neoplasms in their respective fields.
Synchronous osteoclastoma and anaplastic astrocytoma in the same
individual, however, has not been previously reported. The present
study describes the case of a 46-year-old male patient with
synchronous primary malignant tumors of the femoral trochanter and
brain.
Case report
A 46-year-old male presented to the Department of
Orthopedics, The First Affiliated Hospital of Nanchang University
Medical School (Nanchang, Jiangxi, China) with a complaint of
intermittent pain in the left hip for six months and aggravation of
this symptom one month previous to admittance. The medical and
family history of the patient was not significant. The general
physical examination was normal, with the exception of limited
movement and percussion pain in the left hip. A central nervous
system examination revealed normal mental capabilities, a
functioning motor and sensory system and no neck rigidity. All the
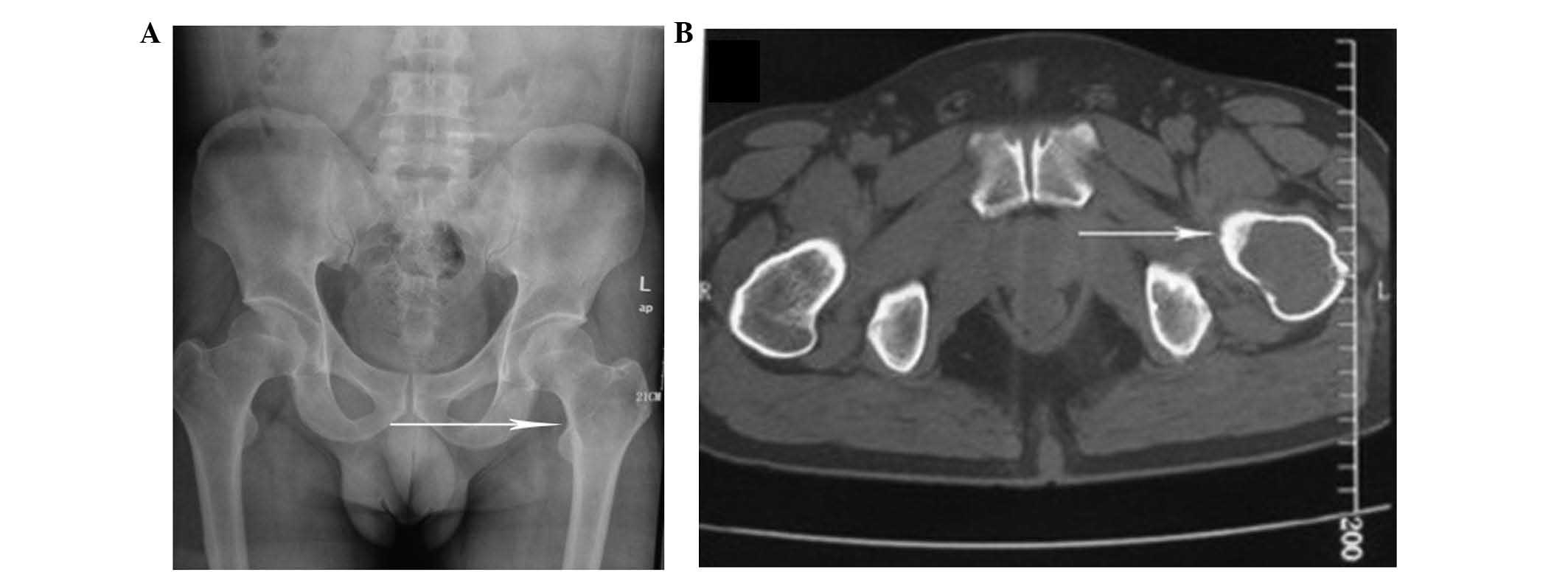
cranial nerves were intact. X-ray and computed tomography (CT;
Fig. 1) of the left hip revealed a
femoral trochanteric lesion and a suspected osteoclastoma. The
patient underwent left femoral tumor curettement with bone cement
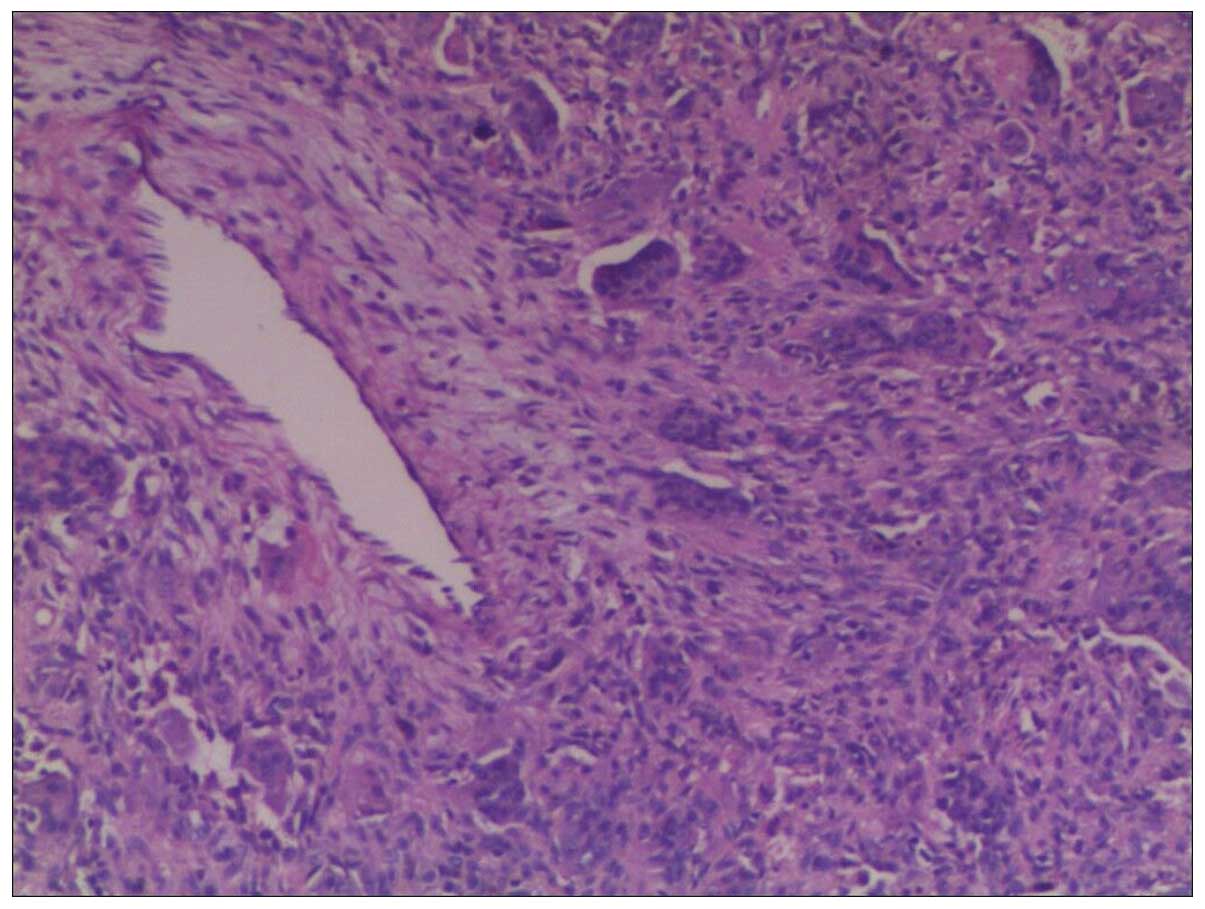
implantation. Intraoperative and post-operative histological
examinations revealed an osteoclastoma (Fig. 2). One week after the surgery, the
patient was discharged without any complications. However, the
patient was admitted to hospital again two weeks later due to a
sudden epileptic seizure that lasted for 4–5 min. The patient also
felt significant pain in the left hip subsequent to regaining
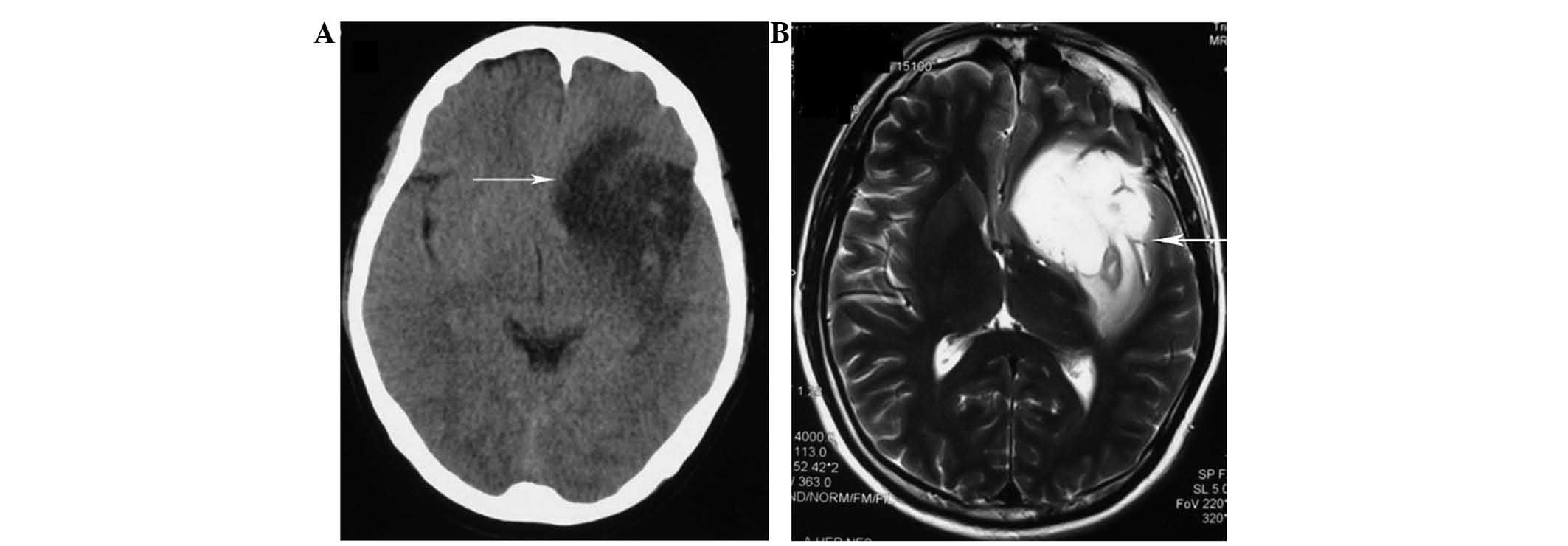
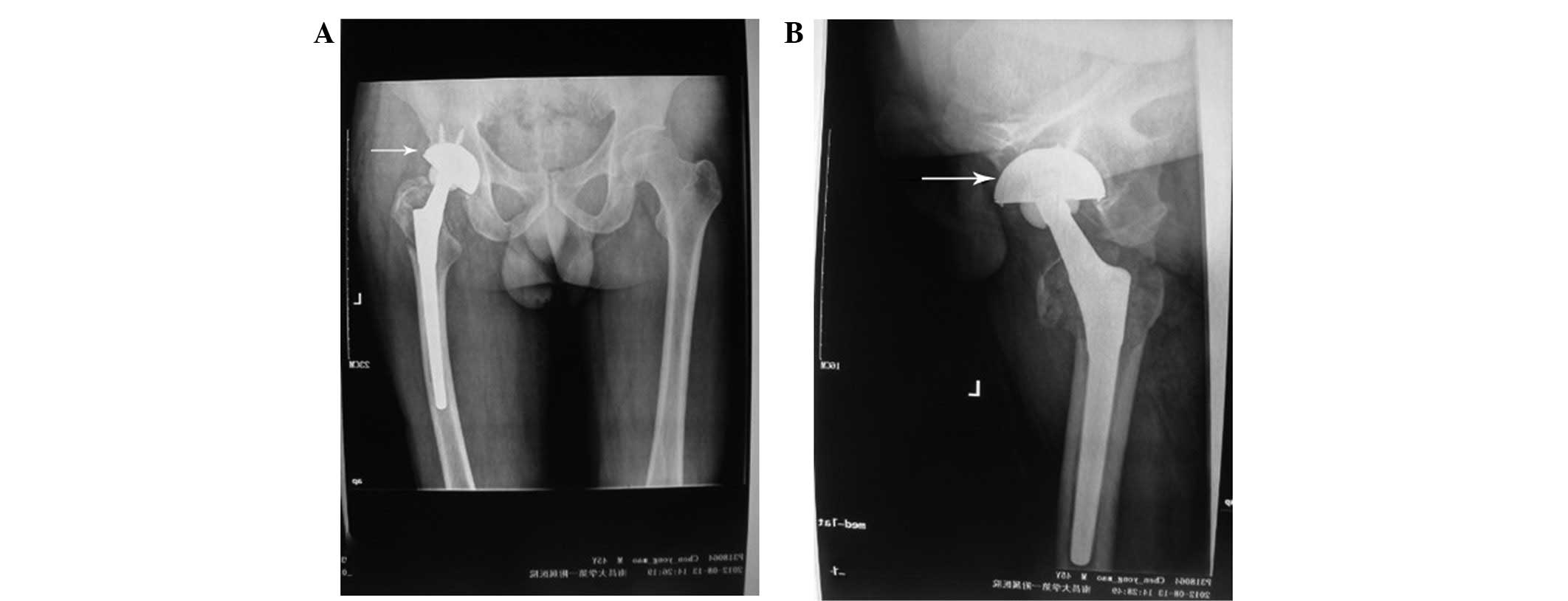
consciousness. X-ray of the pelvis (Fig. 3) revealed a fracture of the left
femoral neck and CT of the brain (Fig.
4A) revealed a lamellar and low-density shadow in the left
frontotemporal region of the brain. Cranial magnetic resonance
imaging (MRI; Fig. 4B) revealed an
abnormal signal intensity in the left frontotemporal region of the
brain, indicating a suspected metastatic tumor or glioma. The
patient underwent a left lateral fissure craniotomy and a gross
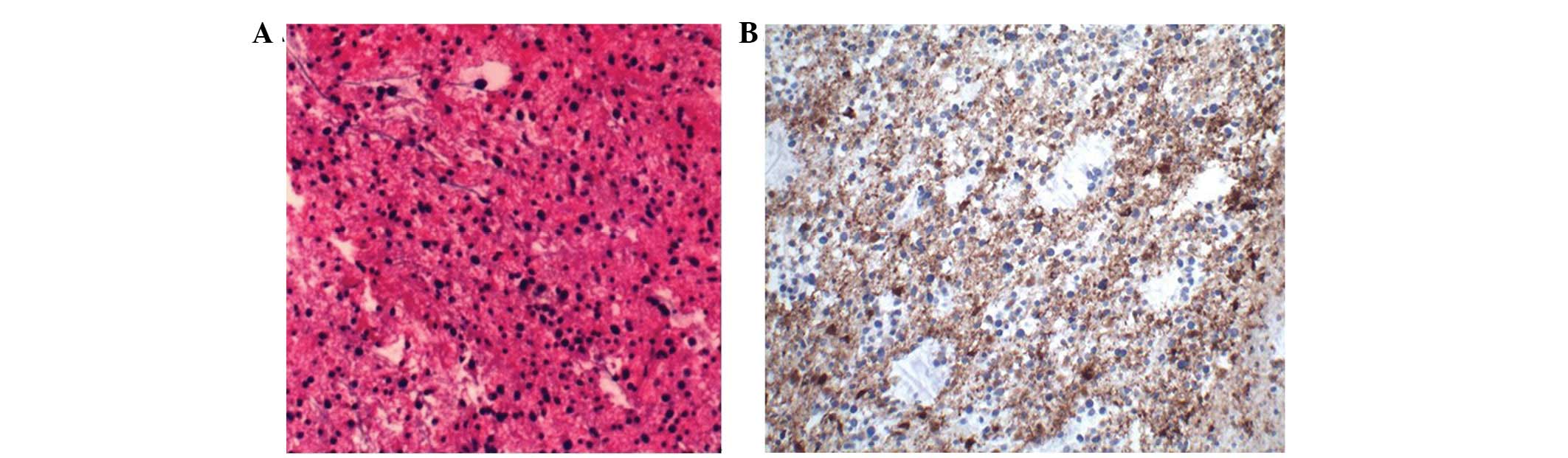
total resection of the lesion. An anaplastic astrocytoma (World
Health Organization scale grade III) was diagnosed following an
examination of a tissue sample (Fig.
5). Subsequently, the patient underwent an additional total hip
arthroplasty (THA) due to the fracture of the left femoral neck
(Fig. 6). The post-operative period
was uneventful and the patient was referred to the Department of
Oncology two weeks later. The patient was administered adjuvant
radiotherapy with (total dose, 60 Gy) and 6 cycles of chemotherapy
as follows: Temozolomide was administered at a dose of 250 mg on
days 1–5 and the course was repeated every 28 days. The patient was
doing well with no evidence of local or distant recurrence more
than six months after the surgery. Approval for this study was
obtained from the ethical review committee of The First Affiliated
Hospital of Nanchang University Medical School and all the
investigations were conducted in conformity with the ethical
principles of research. Informed consent was obtained from the
patient for participation in the study.
Discussion
Multiple primary malignant tumors in an individual
are relatively rare. In a review of the literature on multiple
primary malignant neoplasms, the overall incidence of multiple
primary malignancies has been recorded as 0.73–11.7% (2).
In 1889, Billroth (3) published the first documented
occurrence of multiple primary malignancies. In 1932, Warren and
Gates (4) recommended the following
standard for the classification of multiple primary neoplasms: i)
Each tumor must be distinct; ii) each tumor must present a definite
picture of malignancy; and iii) the chance of one tumor being a
metastasis of the other must be excluded. In 1977, Moertel
(5) proposed the following
definitions of multiple primary neoplasms, which are
classifications that remain widely used today: i) Multifocal, the
two distinct malignancies arise in the same organ or tissue; ii)
systematic, arising in anatomically or functionally allied organs
of the same system; iii) paired, arising in paired organs; and iv)
random, occurring as a co-incidental or accidental association in
unrelated sites. Moertel et al(6) also classified multiple primary
neoplasms into two groups, synchronous, where the neoplasms appear
at the same time or within 6 months, and metachronous, where the
malignancies develop by turn (>6 months). Howe (1) classified multiple primary neoplasms as
those that are observed at the same time or within two months as
synchronous multiple primary neoplasms and these cancers develop at
more than a two-month interval as metachronous multiple primary
neoplasms.
The pathogenesis of multiple primary neoplasms
remains unclear, but previous studies (7,8) have
indicated that certain mechanisms, including genetic and
immunological susceptibility, family history, perennial exposure to
carcinogens, radiotherapy and chemotherapy for primary neoplasms,
may play significant roles in the occurrence of multiple primary
neoplasms. Additionally, Schottenfeld (9) believed that the two neoplasms may
possess a shared etiology if the incidence of a subsequent neoplasm
is significantly higher among those with a previous primary
cancer.
In the patient of the present study, the malignant
features were histopathologically proven in each tumor. Each tumor
was pathologically categorized as a separate type. The tumor that
was detected in the left femoral trochanter was an osteoclastoma
and the tumor in the brain was an anaplastic astrocytoma. These
findings may also support the fact that these two neoplasms
occurred in a random and synchronous manner.
Osteoclastoma is one of the most obscure and
discussed bone tumors, and the histogenesis of the tumor is
uncertain as the histology does not predict the clinical outcome.
The World Health Organization has classified osteoclastoma as ‘an
aggressive, potentially malignant lesion’ (10). Previous studies have shown that 80%
of osteoclastomas have a benign course, with a local rate of
recurrence of 20–50%, and that ~10% undergo malignant
transformation at recurrence, with 1–4% experiencing pulmonary
metastases even in benign cases (11–14).
Astrocytoma is the most common neuroglial tumor, but
is more commonly located in the cerebrum, leptomeninges and spinal
cord, and is usually present with other associated focal
neurological signs and symptoms (15). The designation of a tumor as an
anaplastic astrocytoma reflects a distinct histological
classification of malignant glioma characterized by an abundance of
pleomorphic astrocytes with evidence of mitosis. Although there has
been advancement in available treatments, including surgical
resection, radiation therapy and chemotherapy, the majority of
tumors recur within a few years and these recurrent tumors are more
refractory to subsequent therapies. The survival of patients with
malignant glioma remains poor, with a median survival of 2 years
for patients with anaplastic astrocytoma (16,17).
Proverbially, the early diagnosis of malignancy
prior to the appearance of clinical symptoms is important, and
screening procedures, including pathological and imaging
examinations, should be emphasized as soon as possible.
Furthermore, the possibility of a second or third malignant lesion
should be considered for patients with primary cancer. The
prognosis of patients with multiple primary malignant tumors may be
determined independently by the stage of each malignancy. A study
by Di Martino et al(18)
identified that although the mean lifetime of 18 months and the
5-year survival rate of 11.9% have been observed in patients with
synchronous neoplasms, an early diagnosis and aggressive treatment
of surgery may prolong and improve the quality of the life of the
patient.
The patient in the present study suffered from
synchronous appearance of osteoclastoma and anaplastic astrocytoma,
which is rare and previously unreported in the medical
literature.
Acknowledgements
The authors would like to thank the patient for
providing us with informed written consent for publication of this
case study.
References
|
1
|
Howe HL: A review of the definition for
multiple primary cancers in the United States. Workshop
Proceedings; December 4–6, 2002; Princeton. North American
Association of Central Cancer Registries; New Jersey, Springfield
(IL): May. 2003
|
|
2
|
Demandante CG, Troyer DA and Miles TP:
Multiple primary malignant neoplasms: case report and a
comprehensive review of the literature. Am J Clin Oncol. 26:79–83.
2003. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Billroth CAT: Die allgemeine chirurgische
pathologie und therapie. Handbuch für Studirende und Aerzte. Reimer
G: Berlin: pp. 9081889
|
|
4
|
Warren S and Gates O: Multiple primary
malignant tumors: A survey of the literature and a statistical
study. Am J Cancer. 16:1358–1414. 1932.
|
|
5
|
Moertel CG: Multiple primary malignant
neoplasms: historical perspectives. Cancer. 40(Suppl 4):
S1786–S1792. 1977. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Moertel CG, Dockerty MB and Baggenstoss
AH: Multiple primary malignant neoplasms. Cancer. 14:221–248. 1961.
View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Noh SK, Yoon JY, Ryoo UN, et al: A case
report of quadruple cancer in a single patient including the
breast, rectum, ovary, and endometrium. J Gynecol Oncol.
19:265–269. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Li FP: Second malignant tumors after
cancer in childhood. Cancer. 40:1899–1902. 1977. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Schottenfeld D: Multiple primary cancers.
Cancer Epidemiology and Prevention. Schottenfeld D and Fraumeni JF
Jr: Oxford University Press; New York, NY: pp. 1370–1387. 1996
|
|
10
|
Schajowicz F: Histological Typing of Bone
Tumours. Springer-Verlag; Berlin: 2nd edition. pp. 20–22. 1993
|
|
11
|
Dahlin DC, Cupps RE and Johnson RE Jr:
Giant-cell tumor: a study of 195 cases. Cancer. 25:1061–1070. 1970.
View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Goldengerg RK, Campbell CJ and Bonfiglio
M: Giant cell tumor of bone. An analysis of two hundred and
eighteen cases. J Bone Joint Surg Am. 52:619–664. 1970.PubMed/NCBI
|
|
13
|
Cheng JC and Johnston JO: Giant-cell tumor
of bone. prognosis and treatment of pulmonary metastases. Clin
Orthop Relat Res. 338:205–214. 1997. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Tubbs WS, Brown LR, Beabout JW, Rock MG
and Unni KK: Benign giant-cell tumor of bone with pulmonary
metastases: clinical findings and radiological appearance of
metastases of 13 cases. AJR Am J Roentgenol. 158:331–334. 1992.
View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Gupta B and Raina J: Fascicular multiple
ocular motor nerve paresis as first presentation of anaplastic
astrocytoma. Indian J Ophthalmol. 55:458–460. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
See SJ and Gilbert MR: Anaplastic
astrocytoma: diagnosis, prognosis, and management. Semin Oncol.
31:618–634. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Desjardins A, Reardon DA and Vredenburgh
JJ: Current available therapies and future directions in the
treatment of malignant gliomas. Biologics. 3:15–25. 2009.PubMed/NCBI
|
|
18
|
Di Martino E, Sellhaus B, Hausmann R,
Minkenberg R, Lohmann M and Esthofen MW: Survival in second primary
malignancies of patients with head and neck cancer. J Laryngol
Otol. 116:831–838. 2002.
|