Introduction
As the fourth most common cause of cancer-related
mortality, esophageal cancer has high a incidence and mortality
rate (1). According to statistics,
the incidence rate for esophageal cancer was 22.14/100,000
individuals in 2009, accounting for 7.74% of all new cancer cases.
The mortality rate was 16.77/100,000 individuals, accounting for
9.29% of cancer-related mortalities (2). Conventional treatment of esophageal
cancer includes surgery, radiotherapy and chemotherapy. However,
the 5-year survival rate has not yet improved. Recurrence and
metastasis remain the main causes of mortality in esophageal cancer
patients. It has been reported that lymph node metastasis (LNM) is
the most common type of thoracic esophageal cancer recurrence with
a rate of 94% (3). Cervical and
mediastinal LNM compress the trachea causing tracheal stenosis and
affecting respiratory function, which is a more serious
complication.
The use of an expandable metallic stent has been
reported to be an effective treatment modality for the palliative
treatment of malignant esophageal and inoperable tracheal tumors or
esophagorespiratory fistulae (4–6).
The aim of the present study was to evaluate the
safety and clinical effectiveness of the placement of metallic
expandable stents for the palliative treatment of malignant airway
obstruction due to esophageal cancer with LNM compressing or
infiltrating the trachea.
Patients and methods
Patient information
A retrospective review of 11 patients who underwent
tracheal stent placement between November 2009 and January 2013 was
performed. The characteristics of the patients are summarized in
Table I. The patient group was
comprised of 7 males and 4 females (age range, 58–75 years; mean,
64.5 years). The primary cancer in all the patients was thoracic
esophageal cancer, and all the patients underwent surgical
resection. Of these patients, 9 were pathologically confirmed with
squamous cell carcinoma (6 males and 3 females) and 2 with
adenocarcinoma (1 male and 1 female). All the patients were treated
with chemotherapy following surgery (the specific chemotherapy
methods are unknown). LNM was identified on the post-operative
follow-up computed tomography (CT) images between 3 and 36 months.
All LNMs were in contact with the trachea and caused its
compression (8 upper mediastinal and 3 cervical), with varying
degrees of dyspnea. Two patients with sudden severe airway
obstruction were administered emergency intubation to relieve the
dyspnea. These patients were transferred to the intensive care unit
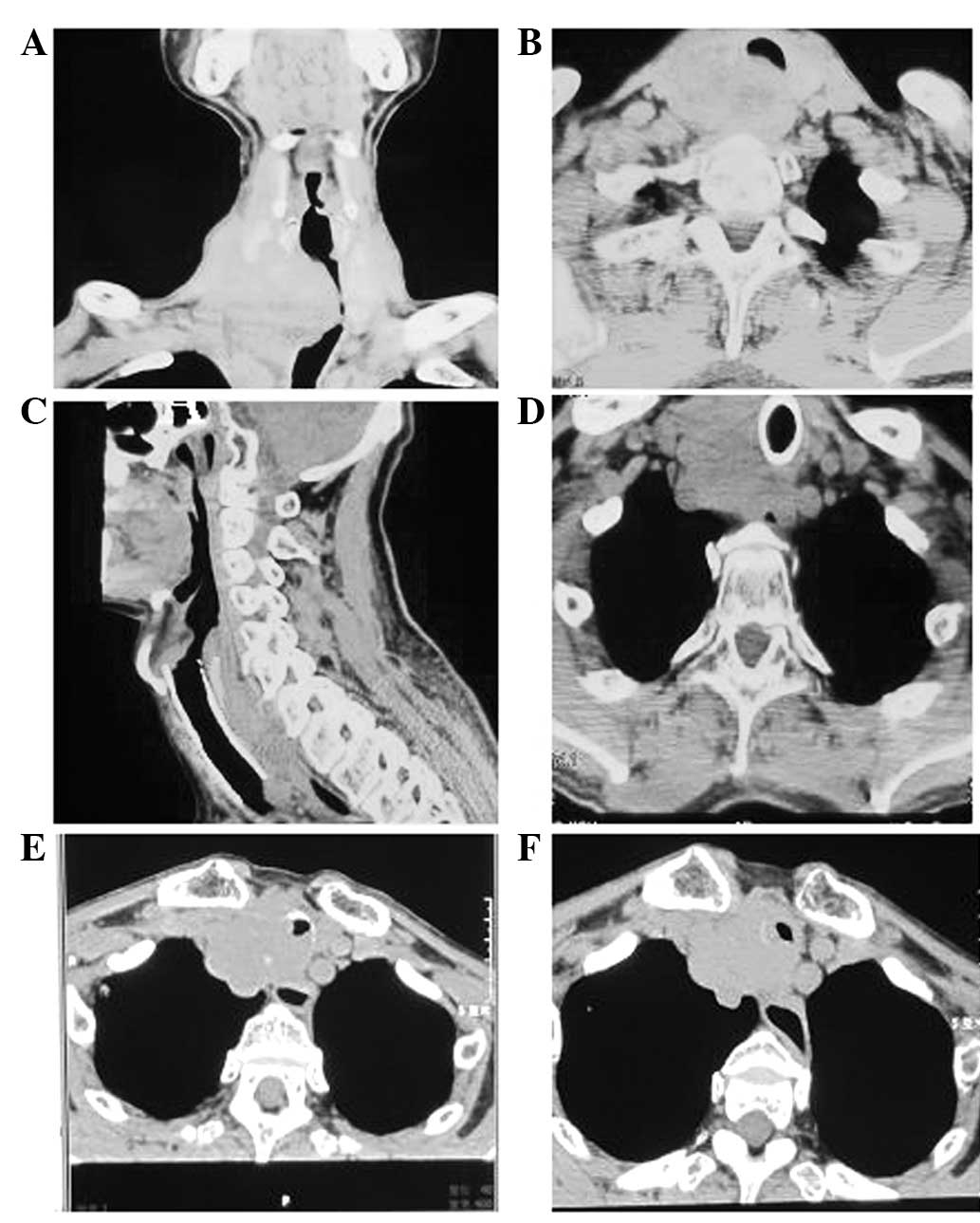
(ICU). The crude estimate mean degree of tracheal stenosis was 68%
(range, 60–75%) according to pre-operative cervical and chest CT
images (Fig. 1A and B). The mean
length of tracheal stenosis was 2.6 cm (range, 2–4 cm). The
criterion of dyspnea was assessed by the modified Borg scale
(7) and the average score was
recorded as 7 (range, 5–10). Other function tests, including
measurements of heart rate (HR), oxygen saturation
(SpO2), measured by oximetry, and respiratory rate (R),
were performed prior to stent placement. Written informed consent
was obtained from the patients.
 | Table IPatient characteristics. |
Table I
Patient characteristics.
| Characteristics | n |
|---|
| No. of patients | 11 |
| Gender |
| Male | 7 |
| Female | 4 |
| Mean age, years
(range) | 64.5 (58–75) |
| Pathology of primary
tumor |
| Squamous cell | 9 |
| Adenocarcinoma | 2 |
| Location of LNM |
| Upper
mediastinal | 8 |
| Cervical | 3 |
| Symptoms |
| Dyspnea | 11 |
| Pyrexia | 3 |
| Cough | 7 |
| Purulent sputum | 1 |
Stent placement
In this study a polyurethane-covered tracheal stent
was used (Micro-Tech Co., Ltd., Nanjing, China). The stent is an
alloy of 55% nickel and 45% titanium, and has thermal memory,
completing its deformation when the temperature is between 20 and
36ºC. The length of the stent was selected based on the extent of
the tracheal stenosis. A measurement 2 cm longer than the vertical
length of the involved segment was selected in order to have 1 cm
at the upper and lower ends of the stent without violation of the
trachea. The diameter of the stent was 18 or 20 mm, depending on
the specific circumstances.
General anesthesia and electrocardiography were used
and blood pressure (BP), heart rate and SpO2 were
measured in all patients. The induction of anesthesia was performed
with a bolus of propofol (2.5 mg/kg), fentanyl (0.001 mg/kg) and
cisatracurium (0.15 mg/kg), then propofol (6 mg/kg/h) maintained
throughout the procedure. Under bronchoscopic guidance, a
0.035-inch exchange guidewire (Radifocus M; Terumo, Tokyo, Japan)
was inserted through the mouth across the stricture. The stent
delivery catheter was then inserted through the guidewire across
the stricture and fixed in the correct location. Once the stent was
fully placed, the stent delivery catheter was removed.
Clinical evaluation of therapy
Post-operatively, all the patients received medical
treatment in the form of systemic and inhalational ambroxol
hydrochloride (15 mg), chymotrypsin (4,000 units) and dexamethasone
(10 mg). Wide-spectrum antimicrobial therapy (cefotiam, 2 g/day)
was applied to the patients with symptoms of infection. All cases
were assessed for the improvement of respiratory function, Borg
score, heart rate and SpO2 at 1 day post-surgery. All
the patients were observed for new complaints of discomfort,
including coughing, hemoptysis, dysphagia, chest pain and change of
voice. Post-operative X-ray was performed on the day of surgery to
confirm the position of the stent.
Follow-ups were performed routinely for each patient
every month. All patients underwent CT scanning.
Statistical analysis
The dyspnea scores, heart rate, SpO2 and
R prior to and following stent placement were analyzed using a
Wilcoxon signed-rank test using SPSS (version 18.0; SPSS, Inc.,
Chicago, IL, USA). P<0.05 was considered to indicate a
statistically significant difference.
Results
A total of 13 stents were successfully placed in 11
patients (Fig. 1C and D), without
any morbidity or mortality. Two patients received double stent
placement since the first stent was not long enough (the length of
the tracheal stenosis was assessed and determined to be
insufficient prior to surgery). The R of all patients demonstrated
immediate improvement post-operatively. The two ICU patients were
extubated and transferred out of the unit following stent
placement. The Borg score was evaluated 1 day after stent
application. The mean score of the dyspnea decreased significantly
from 7.0 to 0.9 (Wilcoxon signed-rank test, P<0.01), the mean HR
decreased from 127.7 to 85.5 bpm (Wilcoxon signed-rank test,
P<0.01), the mean R decreased from 34.4 to 22.6 breaths/min
(Wilcoxon signed-rank test, P<0.01) and the mean SpO2
increased from 85.2 to 96.7% (Wilcoxon signed-rank test, P<0.01)
(Table II).
 | Table IIMean Borg score, HR, R and
SpO2. |
Table II
Mean Borg score, HR, R and
SpO2.
| Time | Borg score | HR, bpm | R, breaths/min | SpO2,
% |
|---|
| Prior to stent | 7.0±1.6 | 127.7±4.9 | 34.4±2.2 | 85.2±2.8 |
| After stent | 0.9±0.5 | 85.5±2.8 | 22.6±0.9 | 96.7±1.4 |
| P-value | <0.01 | <0.01 | <0.01 | <0.01 |
No stent migration or expectoration occurred in any
patient. A small amount of bleeding occurred in one patient
following stent placement, which was controlled by irrigation with
cold saline and adrenaline. No esophageal compression or fistulae
occurred. Regrowth of the tumor tissue at the lower end of the
stent occurred in two cases and sputum retention occurred in five
cases. One of these patients exhibited yellowish and purulent
sputum and subsequently succumbed from the increased sputum content
and consequent pneumonia. Halitosis and bad odor occurred in four
cases, while varying degrees of irritating cough occurred in all
the patients and chest pain was present in two cases, without
dysphagia. Post-operative X-ray and CT scans verified that the
stents were in good positions.
The patients were followed up for 14 days to 12
months subsequent to stent placement. Eight patients survived
following stent application. Two patients succumbed due to tumor
impingement causing tracheal stenosis and one patient succumbed due
to serious infection.
Discussion
Esophageal cancer is one of the more common
malignancies, with high rates of morbidity and mortality. Surgical
resection with radical esophagectomy and lymphadenectomy is
currently the principal methodology for the treatment of esophageal
cancer. However, LNM, including cervical, chest and abdominal
metastasis, may occur in the early stages (1). Li et al(3) and Cai and Xin (8) reported that cervical and upper
mediastinal LN had higher metastasis rates than thoracic LN. LNM is
the most common type of thoracic esophageal cancer recurrence, and
Chen et al(9) reported that
mediastinal LNM accounted for 78.8%. The patients in the present
study all had primary thoracic esophageal tumors. Eight patients
presented with upper mediastinal LNM and three with cervical LNM.
As one of the most serious complications of esophageal cancer LNM,
infringement and compression of the trachea may lead to severe
airway obstruction, thus affecting lung function (5). The principal presenting symptoms in
the present cases included dyspnea, coughing, a purulent sputum,
obstructive pneumonia or combinative syndromes. Oxygen inhalation
and wide-spectrum antimicrobial therapy were ineffective and the
symptoms did not improve. Two patients received emergency
intubation and were transferred to the ICU. Such patients as these,
who have a poor prognosis, may not benefit from surgery with a
curative goal. Instead they require palliative care with the aim of
improving their quality of life.
The first use of an expandable metallic stent for a
case of post-operative bronchial stenosis was presented by Wallace
et al(10). Since then,
metallic stents have been widely used in alleviating symptoms in
the majority of patients with airway obstructions. The
effectiveness of metallic stent implants has been evaluated based
on changes in lung function (5,11,12).
Previous studies have addressed the use of expandable metallic
stents in malignant tracheobronchial strictures and
esophagorespiratory fistulae (6,13). In
the present study, a total of 13 stents were successfully placed in
11 patients. Respiratory function was demonstrated to be
significantly improved in all the patients following tracheal stent
placement (Borg score; P<0.01). HR and R were significantly
decreased (P<0.01) and SpO2 was significantly
increased (P<0.01). Yanagihara et al(14) reported two cases with malignant
tracheal obstruction; following insertion of the Ultraflex stent,
respiration was immediately improved. With regard to complications,
the major and minor complications that develop following stent
placement include stent migration, expectoration, coughing,
hemorrhage, dysphagia, chest pain, retention of secretions,
halitosis and tumor regrowth. Stent migration has been reported
previously (5,15), and in malignant diseases stent
migration has been reported to occur in ~10% of cases (16). No stent migration or expectoration
occurred in the present study patients. Post-operative irritating
coughing occurred in all patients and chest pain occurred in two
patients, which were both relieved after 3 days. Patients
experienced discomfort following stent placement. Halitosis and bad
odor occurred in four cases and disappeared with antibiotics. It is
reported that a bad odor results from the colonization of the stent
with bacteria and fungi (17). A
small amount of bleeding occurred in one patient following stent
placement, which was controlled by irrigation with cold saline and
adrenaline. No patients experienced dysphagia. Sputum retention
occurred in five patients; four were relieved with inhalation of
ambroxol hydrochloride, chymotrypsin and dexamethasone, and one
patient succumbed from increased sputum levels and subsequent
pneumonia. Regrowth of the tumor is the most serious complication.
It has been reported that laser debulking relieves this type of
airway obstruction (5). In the
patients in the present study, regrowth of the tumor tissue
occurred in two patients at the lower end of the stent, which
caused tracheal stenosis (Fig. 1E and
F). These patients stopped treatment and then succumbed from
dyspnea.
In conclusion, metallic expendable stent placement
is an effective and safe method for malignant airway obstruction.
It is easily inserted under general anesthesia using bronchoscopy,
alleviating dyspnea and improving the quality of life of patients
with advanced cancer. Additionally, it allows patients to continue
chemotherapy or radiotherapy.
References
|
1
|
Wei W, Yang J, Zhang S, et al: Esophageal
cancer mortality trends during the last 30 years in high risk areas
in China: comparison of results from national death surveys
conducted in the 1970’s, 1990’s and 2004–2005. Asian Pac J Cancer
Prev. 12:1821–1826. 2011.PubMed/NCBI
|
|
2
|
Chen W, He Y, Zheng R, et al: Esophageal
cancer incidence and mortality in China, 2009. J Thorac Dis.
5:19–26. 2013.
|
|
3
|
Li CL, Zhang FL, Wang YD, et al:
Characteristics of recurrence after radical esophagectomy with
two-field lymph node dissection for thoracic esophageal cancer.
Oncol Lett. 5:355–359. 2013.PubMed/NCBI
|
|
4
|
Baron TH: Expandable metal stents for the
treatment of cancerous obstruction of the gastrointestinal tract. N
Engl J Med. 344:1681–1687. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Gaafar AH, Shaaban AY and Elhadidi MS: The
use of metallic expendable tracheal stents in the management of
inoperable malignant tracheal obstruction. Eur Arch
Otorhinolaryngol. 269:247–253. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Shin JH, Song HY, Ko GY, et al:
Esophagorespiratory fistula: long-term results of palliative
treatment with covered expandable metallic stents in 61 patients.
Radiology. 232:252–259. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
No authors listed. Dyspnea. Mechanisms,
assessment, and management: a consensus statement American Thoracic
Society. Am J Respir Crit Care Med. 159:321–340. 1999. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Cai WJ and Xin PL: Pattern of relapse in
surgical treated patients with thoracic esophageal squamous cell
carcinoma and its possible impact on target delineation for
postoperative radiotherapy. Radiother Oncol. 96:104–107. 2010.
View Article : Google Scholar
|
|
9
|
Chen G, Wang Z, Liu XY and Liu FY:
Recurrence pattern of squamous cell carcinoma in the middle
thoracic esophagus after modified Ivor-Lewis esophagectomy. World J
Surg. 31:1107–1114. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Wallace MJ, Charnsangavej C, Ogawa K, et
al: Tracheobronchial tree: expandable metallic stents used in
experimental and clinical applications. Work in progress Radiology.
158:309–312. 1986.PubMed/NCBI
|
|
11
|
Vergnon JM, Costes F, Bayon MC and Emonot
A: Efficacy of tracheal and bronchial stent placement on
respiratory functional tests. Chest. 107:741–746. 1995. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Hauck RW, Romer W, Schulz C, et al:
Ventilation perfusion scintigraphy and lung function testing to
assess metal stent efficacy. J Nucl Med. 38:1584–1589.
1997.PubMed/NCBI
|
|
13
|
Shin JH, Kim SW, Shim TS, et al: Malignant
tracheobronchial strictures: palliation with covered retrievable
expandable nitinol stent. J Vasc Interv Radiol. 14:1525–1534. 2003.
View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Yanagihara K, Mizuno H, Wada H and Hitomi
S: Tracheal stenosis treated with self-expanding nitinol stent. Ann
Thorac Surg. 63:1786–1789. 1997. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Remacle M, Lawson G, Jamart J and Keghian
J: Progressive experience in tracheal stenting with expendable
stents. Eur Arch Otorhinolaryngol. 260:369–373. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Zakaluzny SA, Lane JD and Mair EA:
Complications of tracheobronchial airway stents. Otolaryngol Head
Neck Surg. 128:478–488. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Noppen M, Piérard D, Meysman M, Claes I
and Vincken W: Bacterial colonization of central airways after
stenting. Am J Respir Crit Care Med. 160:672–677. 1999. View Article : Google Scholar : PubMed/NCBI
|