Introduction
Small cell carcinoma is one of the histopathological
subtypes that demonstrates aggressive clinical behavior and most
commonly arises in the lung. However, albeit rare, it can occur at
extrapulmonary sites, such as the gastrointestinal tract,
pancreatobiliary system, salivary gland, uterine cervix and urinary
tract. Extrapulmonary small cell carcinoma comprises ~4% of all
small cell carcinomas. Extrapulmonary small cell carcinomas share
histopathological and immunohistochemical features with their
pulmonary counterpart. The tumor cells are small in size and
relatively uniform. They have scant cytoplasm, powdery chromatin
and inconspicuous nucleoli. Mitotic figures and apoptotic bodies
are commonly observed, and the presence of geographic necrosis is
also characteristic. Immunohistochemically, the neoplastic cells
show positive immunoreactivity for neuroendocrine markers, such as
chromogranin A, synaptophysin and CD56 (1,2).
The occurrence of small cell carcinoma is rare in
the urinary bladder and prostate, and its incidence is reported to
be 0.3–0.7% and 0.5–2% of all primary carcinomas of the urinary
bladder and prostate, respectively (1,2).
Although the histopathological features of small cell carcinoma of
the urinary bladder are well-recognized, only a few reports on the
cytological features of the urine specimen of this type of tumor
have been documented (3–8). Moreover, the urinary cytological
features of small cell carcinoma of the prostate have rarely been
reported (9). In this retrospective
study, we analyzed the urinary cytological features of small cell
carcinoma of the urinary bladder and prostate and discuss the
usefulness of cytological examination of urine specimen for this
type of tumor.
Materials and methods
Urine specimens from patients at Shiga University of
Medical Science Hospital (Shiga, Japan) diagnosed
histopathologically as small cell carcinoma of the urinary bladder
or prostate were retrieved. Four urine specimens from four patients
were available in this study. The specimens were all voided urine
samples that were obtained preceding the patients' surgical
procedure or cystoscopy. The cytological specimens were
Papanicolaou-stained and analyzed for cytological features,
including background, number of neoplastic cells, cellular
arrangement, cell size and shape, as well as nuclear features.
Tissues from cystoscopic, surgical resections or
biopsy were fixed by formalin and embedded in paraffin. Tissue
sections were stained with hematoxylin and eosin, and subjected to
immunohistochemistry using an autostainer (BenchMark XT system;
Ventana Medical Systems Inc., Tucson, AZ, USA) according to the
manufacturer's instructions. The following primary antibodies were
used: Mouse monoclonal antibody against CD56 (CD564; Novocastra
Laboratories, Ltd., Newcastle upon Tyne, UK), mouse monoclonal
antibody against chromogranin A (DAK-A3; DAKO Cytomation, Glostrup,
Denmark) and mouse monoclonal antibody against synaptophysin
(27G12; Novocastra Laboratories, Ltd.). The study was approved by
the ethics committee of Shiga University of Medical Science (Shiga,
Japan). Written informed consent was obtained from the
patients.
Results
Clinicopathological features
Table I summarizes
the clinicopathological features of four cases of small cell
carcinoma of the urinary bladder and prostate. This study included
two urinary bladder and two prostate cases. All cases were elderly
men (average age, 74 years; range, 64–82 years). Multiple liver
metastases (case 1) and direct urinary bladder invasion (cases 3
and 4) were detected by imaging analyses.
 | Table IClinicopathological features of small
cell carcinoma of the urinary bladder and prostate. |
Table I
Clinicopathological features of small
cell carcinoma of the urinary bladder and prostate.
| | | | Cytological
features | Histopathological and
immunohistochemical features |
|---|
| | | |
|
|
|---|
| Case no. | Age (years) | Gender | Location | Background | Number of tumor
cells | Cellular
arrangement | Other component | Immunohistochemical
features |
|---|
| 1 | 77 | Male | Urinary bladder | Clean | Many | Small clusters | Carcinoma in
situ | Syn(+), CD56(+),
Chr(−) |
| 2 | 82 | Male | Urinary bladder | Inflammatory | A few | Small clusters | None | Syn(+), CD56(+),
Chr(−) |
| 3 | 64 | Male | Prostate | Inflammatory | Many | Small clusters | Adenocarcinoma | Syn(+), CD56(+),
Chr(−) |
| 4 | 73 | Male | Prostate | Inflammatory | A few | Small clusters to
single | Adenocarcinoma | Syn(+), CD56(+),
Chr(−) |
Cytological findings
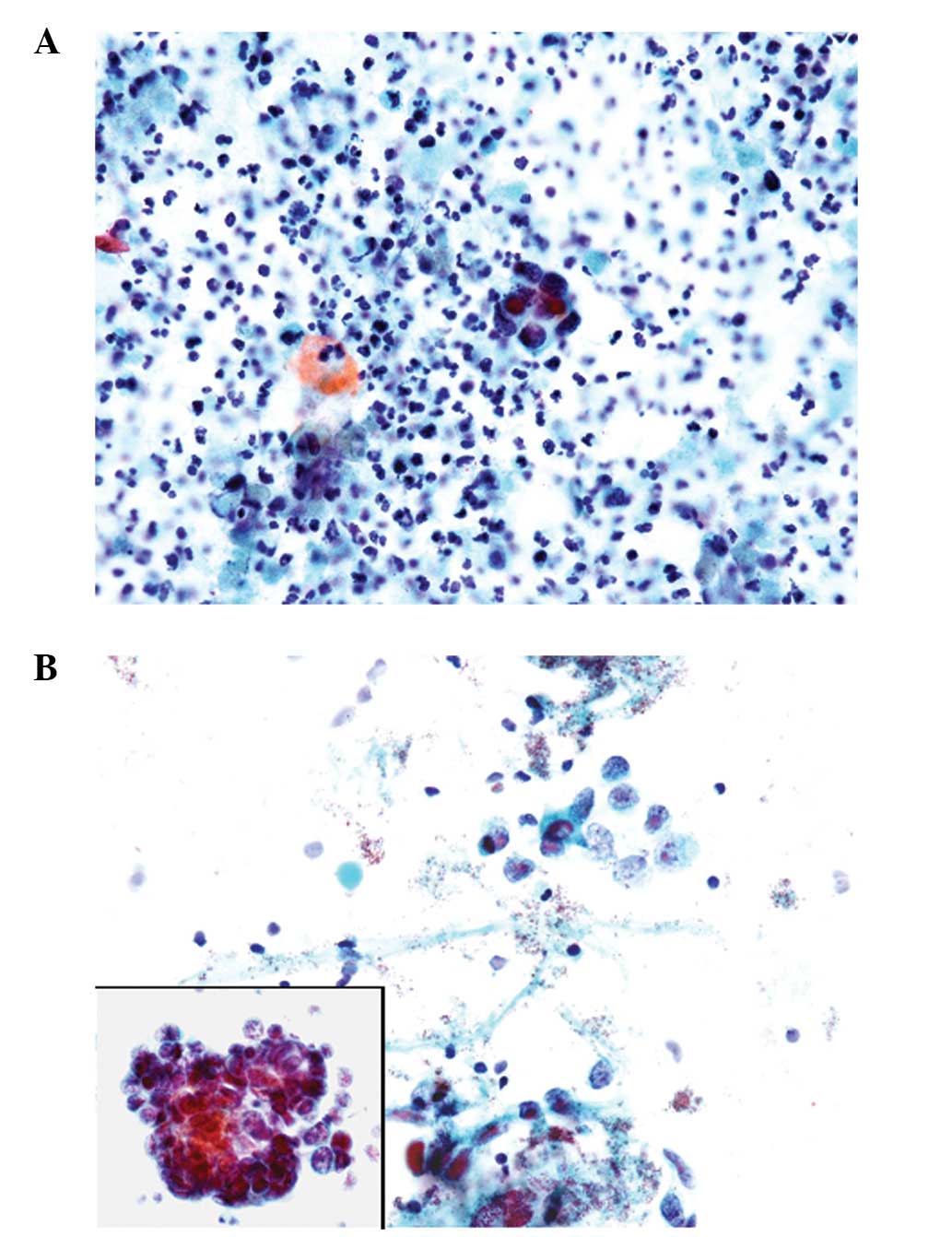
The cytological features of the four cases are
summarized in Table I. The
background of the urine specimens was mostly inflammatory, in which
numerous neutrophils were present. Necrotic material was also
occasionally observed in cases 2–4 (Fig. 1A), whereas the background was clean
in case 1. A number of tumor cells were observed in one urinary
bladder case (case 1) and one prostate case (case 3); however, only
a few neoplastic cells were present in cases 2 and 4. The
neoplastic cells were small in size, had scant cytoplasm and a high
nuclear/cytoplasmic ratio, and were arranged in small clusters or
occasionally as single cells (Fig. 1A
and B). The tumor cell clusters demonstrated prominent nuclear
molding (Fig. 1B). The nuclei of
the neoplastic cells were round to oval in shape with finely
granular chromatin containing inconspicuous nucleoli (Fig. 1A and B). Neither conventional
urothelial carcinoma nor adenocarcinoma components were observed in
the cytological specimens of any of the cases.
Histopathological findings
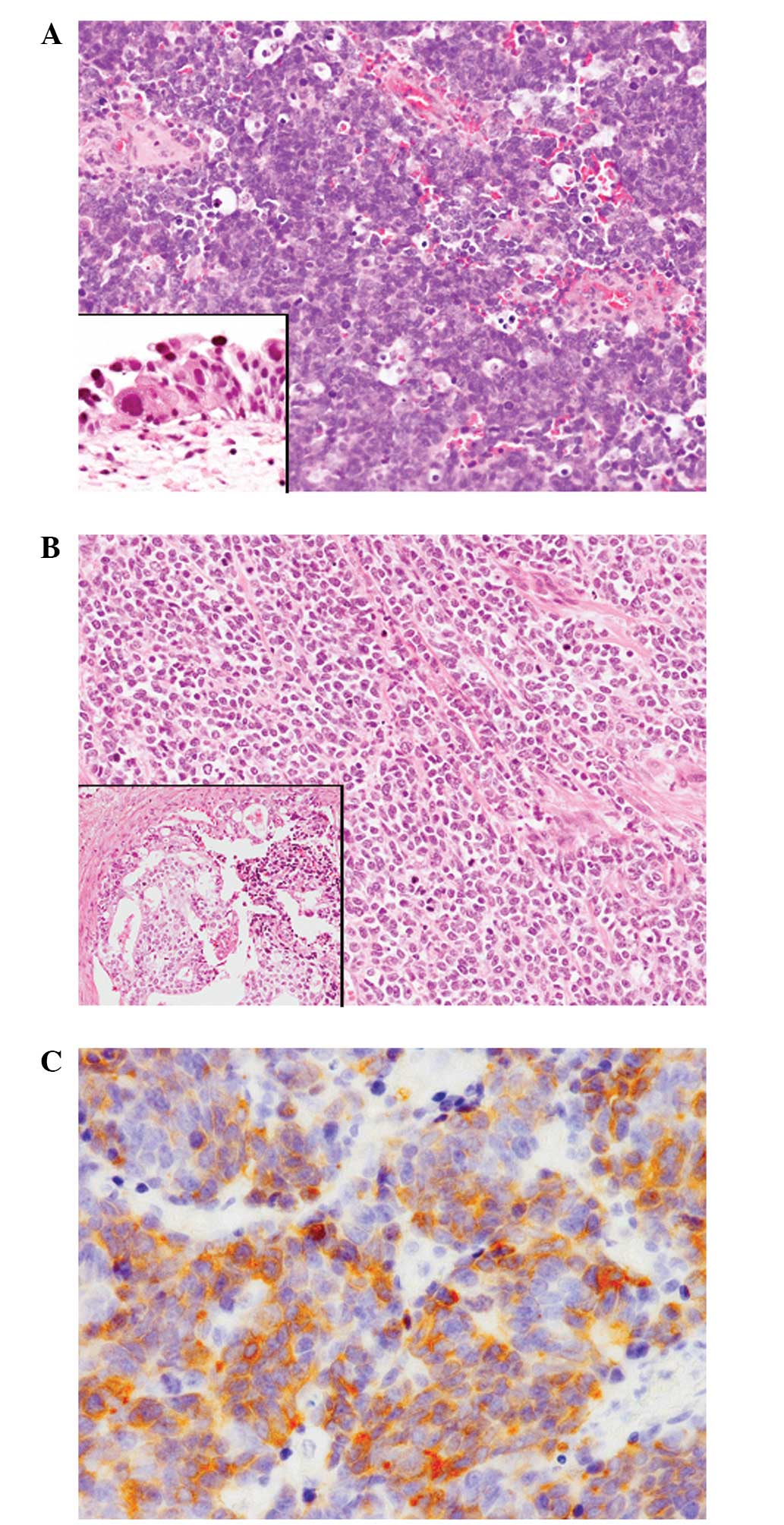
The urinary bladder and prostate cases showed
fundamentally the same histopathological features. Diffuse
proliferation of the small-sized neoplastic cells with occasional
geographic necrosis was observed. These tumor cells had scant
cytoplasm and round to oval hyperchromatic nuclei without nucleoli
(Fig. 2A and B). Mitotic figures
and apoptotic bodies were frequently observed (Fig. 2A and B). Direct invasion into the
urinary bladder or the prostate portion of the urethra was observed
in cases 3 and 4.
A carcinoma in situ component was present in
the surrounding bladder mucosa in case 1 (Fig. 2A, inset); however, no other
components were detected in case 2. A conventional adenocarcinoma
component was present in the two prostate cases (Fig. 2B).
Immunohistochemical findings
Synaptophysin and CD56 were diffusely expressed in
all four cases (Fig. 2C); however,
none of these cases presented positive immunoreactivity for
chromogranin A.
Discussion
The cytological examination of urine specimens is
important in the detection, diagnosis and follow-up of patients
with bladder cancer. It is well-recognized that cytological
examination of urine specimens has high sensitivity for detection
of conventional high-grade urothelial carcinoma (10). Additionally, the cytological
features of rare histopathological variants of urothelial
carcinoma, such as micropapillary, nested and sarcomatoid, have
also been described (11–16). However, prostate cancer cells are
rarely identified in the urinary cytological specimen (17), and it has been recognized that
routine examination of urine cytology for detection of prostate
cancer is not recommended due to low sensitivity (18).
The cytological features of previously reported
cases of small cell carcinoma of the urinary bladder are as
follows: i) isolated single cells or small groups of the neoplastic
cells are present in a hemorrhagic and inflammatory background; ii)
nuclear molding is characteristic; iii) the tumor cells are small
to medium in size with scant cytoplasm and have a high
nuclear/cytoplasmic ratio; and iv) the nuclei are hyperchromatic
containing finely granular chromatin without inconspicuous nucleoli
(3–8). These cytomorphological features
correspond to those of pulmonary small cell carcinoma and are also
the same as those of the previously reported cytological features
of small cell carcinoma of the prostate (9). The cytological features of the current
four cases of small cell carcinoma of the urinary bladder and
prostate are identical to the abovementioned features.
Small cell carcinoma of the bladder frequently has
another histopathological component, which is present in 40–50% of
cases (19). The most common
component is a conventional urothelial carcinoma, including
carcinoma in situ, followed by squamous cell carcinoma and
adenocarcinoma (1). Case 1 in the
present study had a carcinoma in situ component. Therefore,
other carcinoma components, such as conventional high-grade
urothelial component, can be detected in the urinary cytological
specimen; although, a conventional urothelial carcinoma component
was not observed in the urinary cytological specimen of case 1. von
Hoeven and Artymyshyn reported the cytological features of 13 cases
of small cell carcinoma of the urinary bladder (6). The cases included nine cases of mixed
small cell carcinoma: One case of urothelial dysplasia, three cases
of carcinoma in situ, three cases of invasive urothelial
carcinoma, one case of adenocarcinoma, and one case of
adenocarcinoma and squamous cell carcinoma. Among 31 urine
specimens from those mixed small cell carcinoma cases, only nine
specimens had exclusively non-small cell type carcinoma cells, and
the remaining 22 specimens included only small cell carcinoma
components (6). In contrast, Acs
et al reported the cytological characteristics of six cases
of small cell carcinoma of the urinary bladder (3). In five of the cases, the majority of
tumor cells in the urine specimens belonged to conventional
urothelial cell carcinoma component, leading to a cytodiagnosis of
urothelial carcinoma in these cases (3). Therefore, the authors claimed that the
presence of conventional urothelial carcinoma component can mask
the coexisting small cell carcinoma component (3). Moreover, high-grade urothelial
carcinoma may occasionally resemble small cell carcinoma. However,
the presence of cellular pleomorphism and prominent nucleoli, as
well as lack of nuclear molding, aid in distinguishing conventional
urothelial carcinoma from small cell carcinoma (3,5). Small
cell carcinoma shows characteristic cytological features; thus,
careful observation of the urinary cytological specimen can lead to
a correct diagnosis even if a conventional urothelial carcinoma
component is present, since this type of tumor shows a highly
aggressive clinical course and early diagnosis is important
(1).
In addition, small cell carcinoma of the prostate
frequently has a conventional adenocarcinoma component. According
to the largest study of this type of tumor reported by Wang and
Epstein, pure small cell carcinoma was observed in 54 of 95 (57%)
cases with the remaining cases admixed with conventional prostate
adenocarcinoma (2). The current two
prostate cases also had a conventional adenocarcinoma component.
However, conventional adenocarcinoma was not detected in the urine
specimen in the two cases. It is speculated that conventional
adenocarcinoma components were present within the prostate, whereas
small cell carcinoma components had directly invaded into the
urinary bladder or the prostatic portion of the urethra in the two
cases, resulting in the presence of only the small cell carcinoma
component in the urine specimen. Small cell carcinoma of the
prostate also shows an aggressive clinical course (20), thus early detection is required for
appropriate treatment. This report indicates that a cytodiagnosis
of this type of tumor may be possible since it frequently invades
into the urinary bladder or prostatic portion of the urethra.
In conclusion, we described the cytological features
of four cases of small cell carcinoma of the urinary bladder and
prostate. The cytological features of this type of tumor are
characteristic. Therefore, careful observation of the urine
specimen can lead to a correct diagnosis of small cell carcinoma of
the urinary bladder. In addition, a cytodiagnosis of prostate small
cell carcinoma may also be possible.
References
|
1
|
Zhao X and Flynn EA: Small cell carcinoma
of the urinary bladder. A rare, aggressive neuroendocrine
malignancy. Arch Pathol Lab Med. 136:1451–1459. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Wang W and Epstein JI: Small cell
carcinoma of the prostate. A morphologic and immunohistochemical
study of 95 cases. Am J Surg Pathol. 32:65–71. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Acs G, Gupta PK and Baloch ZW:
Cytomorphology of high-grade neuroendocrine carcinoma of the
urinary tract. Diagn Cytopathol. 23:92–96. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Yamaguchi T, Imamura Y, Shimamoto T, et
al: Small cell carcinoma of the bladder. Two cases diagnosed by
urinary cytology. Acta Cytol. 44:403–409. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Ali SZ, Reuter VE and Zakowski MF: Small
cell neuroendocrine carcinoma of the urinary bladder. A
clinicopathologic study with emphasis on cytologic features.
Cancer. 79:356–361. 1997. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
van Hoeven KH and Artymyshyn RL: Cytology
of small cellcarcinoma of the urinary bladder. Diagn Cytopathol.
14:292–297. 1996.
|
|
7
|
Borghi L, Bianchini E and Altavilla G:
Undifferentiated small-cell carcinoma of the urinary bladder:
report of two cases with a primary urinary cytodiagnosis. Diagn
Cytopathol. 13:61–65. 1995. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Rollins S and Schumann GB: Primary urinary
cytodiagnosis of a bladder small-cell carcinoma. Diagn Cytopathol.
7:79–82. 1991. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Nguyen-Ho P, Nguyen GK and Villanueva RR:
Small cell anaplastic carcinoma of the prostate: report of a case
with positive urine cytology. Diagn Cytopathol. 10:159–161. 1994.
View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Brown FM: Urine cytology. It is still the
gold standard for screening? Urol Clin North Am. 27:25–37.
2000.
|
|
11
|
Zhu B, Rohan SM and Lin X: Urine
cytomorphology of micropapillary urothelial carcinoma. Diagn
Cytopathol. 41:485–491. 2013. View
Article : Google Scholar : PubMed/NCBI
|
|
12
|
Nicolas MM, Jagirdar JS, Arisco AM and
Valente PT: Micropapillary carcinoma of the urinary bladder: report
of a case and review of its cytologic features. Diagn Cytopathol.
39:784–787. 2011. View
Article : Google Scholar : PubMed/NCBI
|
|
13
|
Sakuma T, Furuta M, Mimura A, Tanigawa N,
Takamizu R and Kawano K: Urine cytology of micropapillary carcinoma
of the urinary bladder. Diagn Cytopathol. 39:852–856. 2011.
View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Cardillo M, Reuter VE and Lin O: Cytologic
features of the nested variant of urothelial carcinoma. A study of
seven cases. Cancer. 99:23–27. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Iwa N, Ito S, Takegaki Y, et al: Cytologic
features of sarcomatoid carcinoma of the urinary bladder: a case
report. Diagn Cytopathol. 41:536–541. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Arita N, Ishida M, Yoshida K, et al:
Sarcomatoid variant of urothelial carcinoma: Cytological analysis
of three cases. Oncol Lett. 5:49–52. 2013.PubMed/NCBI
|
|
17
|
Tyler KL and Selvaggi SM: Morphologic
features of prostatic adenocarcinoma on ThinPrep®
urinary cytology. Diagn Cytopathol. 39:101–104. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Varma VA, Fekete PS, Franks MJ and Walther
MM: Cytologic features of prostatic adenocarcinoma in urine: a
clinicopathologic and immunocytochemical study. Diagn Cytopathol.
4:300–305. 1988. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Mazzucchelli R, Morichetti D,
Lopez-Beltran A, et al: Neuroendocrine tumours of the urinary
system and male genital organs: clinical significance. BJU Int.
103:1464–1470. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Umemura K, Nakagawa G, Chikui K, et al: A
useful treatment for patients with advanced mixed-type small cell
neuroendocrine carcinoma of the prostate: A case report. Oncol
Lett. 5:793–796. 2013.PubMed/NCBI
|