Introduction
Infection is the leading cause of morbidity and
mortality among patients with hematological malignancies (1). Previously, Gupta et al
retrospectively studied six cases with tuberculosis among 382 acute
lymphoblastic leukemia patients with febrile episodes; the rate of
infection with tuberculosis was 1.57% (2). Patients with hematological
malignancies have been reported to develop tuberculosis during or
following chemotherapy (1,3). In addition, the diagnosis of
tuberculosis is often difficult to determine due to its atypical
symptoms, various radiographic observations and other examinations,
such as negative purified protein derivative (PPD) skin test.
Therefore, it is necessary to pay more attention to these
patients.
The current study describes a case of scrofula and
pulmonary tuberculosis with acute myelocytic leukemia (AML).
Notably, the tuberculosis infection may have existed prior to the
diagnosis of AML and then become aggravated during and following
the chemotherapy. In addition, the patient presented with fever,
lymphadenopathy and hemophagocytosis in the bone marrow. The
current case report highlights that clinicians must be alerted to
atypical characteristics of tuberculosis infection, particularly
among patients with hematological malignancies.
Case report
In November 2010, a 23-year-old male was referred to
the Hematology Clinic of the Second Xiangya Hospital (Changsha,
China) with a fever and dry cough for one week. The patient’s blood
routine (BR) showed a white blood cell count of
76.8×109/l, hemoglobin count of 6.6 g/dl, red blood cell
count of 1.87×1012/l and platelet count of
31×109/l, with 87.80% neutrophils. Subsequently, the
patient was admitted to the Department of Hematology (The Second
Xiangya Hospital, Central South University, Changsha) for further
evaluation. The patient had no history of tuberculosis in the
family.
On admission, the patient had a body temperature of
39.0°C. No abnormality was identified on physical examination. In
the peripheral blood work, lactic dehydrogenase (LDH) was high at
937.5 μ/l (upper limit of normal, 245.0 μ/l) and bone marrow
aspiration revealed 77% myeloblasts. Peroxidase staining was
positive and immunophenotype examination revealed that these cells
had originated from myeloblastic cell lines. In addition, AML1/ETO
fusion gene expression was positive. X-ray chest radiograph showed
enlargement of the left hilar, laminar shadow and marginal
infiltration in the right lower lung lobe. Therefore, the diagnosis
of AML-M2a was determined and the induction chemotherapy was
initiated, with empiric antibiotics.
However, although the BR and bone marrow aspiration
indicated that the patient had achieved remission 14 days following
the first cycle of chemotherapy, the patient continued to complain
of repeated irregular fever and occasional frothy sputum, which did
not respond to the broad-spectrum antibiotic and antimycotic
treatments. During that time, sputum acid-fast smear was negative
three times, and blood and sputum cultures for bacteria and fungi
were sterile five times.
One month following the completion of the induction
chemotherapy, the patient was administered the second cycle of
chemotherapy. In order to identify the origin of the fever, bone
marrow aspiration was performed again, which presented the
morphology of myeloblasts to be roughly normal, accounting for 3%,
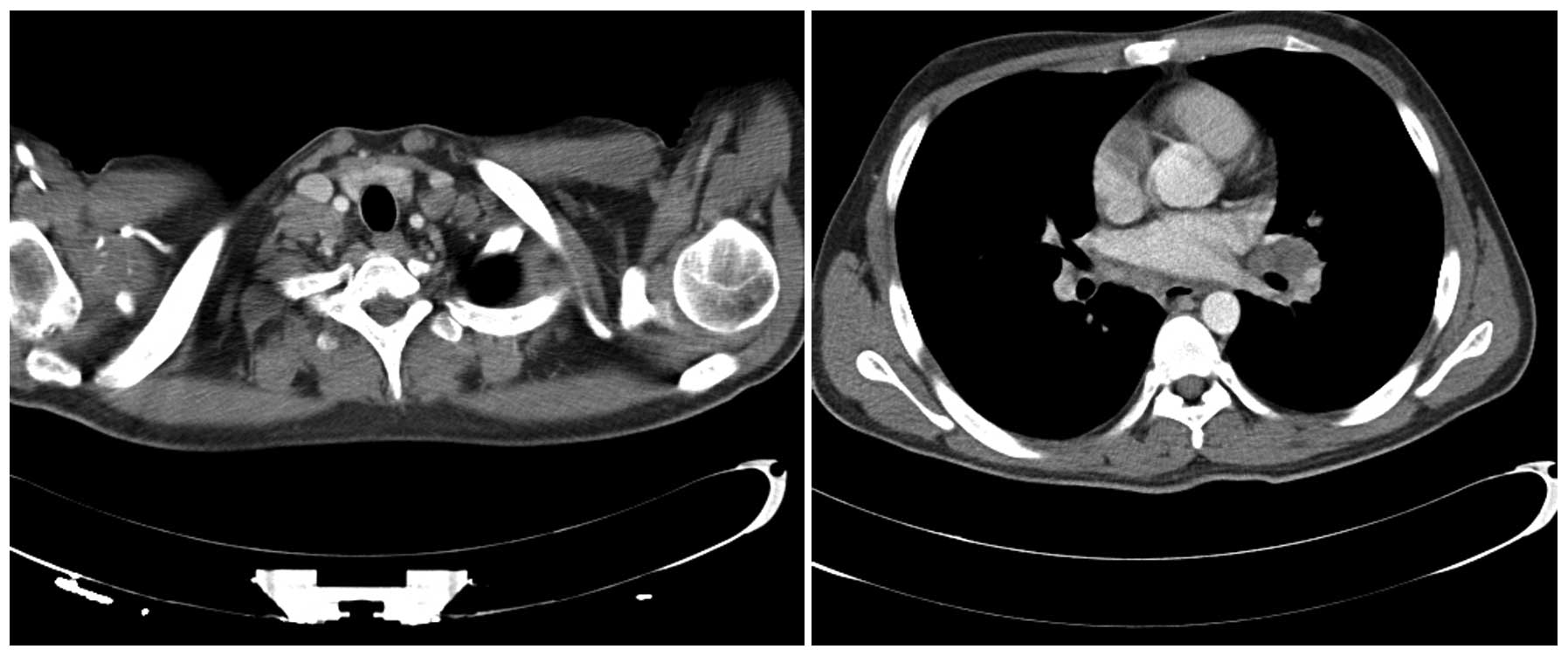
with occasional hemophagocytosis. Computed tomography (CT) of the
brain, abdomen and pelvis showed splenomegaly; chest CT identified
multiple enlarged lymph nodes in the bilateral supraclavicular
fossa, mediastinum and left hilus and a number of lymph nodes that
had become confluent masses, with a maximum size of 3×4 cm
(Fig. 1). In addition, the blood
C-reactive protein levels were 81.70 mg/l (upper limit of normal,
8.00 mg/l), ferritin levels were 2,098.27 ng/ml (upper limit of
normal, 274.66 ng/ml), LDH levels were 382.5 μ/l and fibrinogen
levels were 522 mg/dl (upper limit of normal, 400 mg/dl). The
immunological examination for infections of bacteria, viruses and
parasites suggested PPD-antibody (Ab) IgG (+), MycoDot™ (+), Widal
reaction (−) and galactomannan (GM) test (−), and cardiac color
ultrasound revealed marginal pericardial effusion. The patient
exhibited 8 mm of induration in response to the PPD skin test. The
patient was administered a diagnostic treatment, including
isoniazid, rifampicin, pyrazinamide and fluoroquinolones. One week
later, due to poor liver function, the rifampicin was terminated
and the patient was discharged with prescriptions for isoniazid and
pyrazinamide only, in January, 2011.
One month later, the patient was referred to our
department again for the second consolidation chemotherapy with no
complaints of fever and cough. However, several peanut-sized lymph
nodes were palpated in the right supraclavicular fossa and
subclavicular area, without tenderness. CT revealed enlarged lymph
nodes in the bilateral supraclavicular fossa, mediastinum and left
hilus. Some of the nodes had merged into masses, the maximum
diameter of which was 3 cm. The air tube and bronchus were
marginally compressed and bilateral pleural thickening was
observed. The patient then underwent surgical excision of the
supraclavicular fossa lymph node. The histology of the specimen
showed caseous necrosis, epithelioid cell nodules and multinuclear
giant cells (Fig. 2A). However, the
acid fast bacilli (AFB) staining of this specimen was negative. Due
to the liver dysfunction (high levels of transaminase and total
bilirubin), only two antituberculosis drugs (isoniazid and
ethambutol) and the second consolidation chemotherapy were
administered simultaneously. The surgical incision healed well and
the patient was discharged with prescriptions for these two
antituberculosis drugs and liver protective drugs.
During the ensuing two months, the patient
frequently had a cough with no fever and the biopsy incision became
infected, covered by a yellow-green pyogenic moss. BR, bone marrow
aspiration and AML1-ETO fusion gene showed that the patient had
achieved complete remission. In addition, chest CT revealed a few
massive dot shadows in the left upper lobe, with obscured edges and
evidently enlarged lymph nodes of the mediastinum and left hilus,
with the neighboring bronchus compressed and narrowed. Due to the
fact that the tuberculosis had been poorly controlled and lung
deterioration was radiographically observed, chemotherapy was
interrupted. The patient received three antituberculosis drugs
(isoniazid, rifapentin and ethambutol). Two months following the
initiation of the three antituberculosis drug treatments, the
patient continued to occasionally present with a mild fever during
the afternoon; however, the patient’s temperature returned to
normal levels without special treatment. In addition, the dry cough
continued and a yellow-green purulent ulcer continued to exist in
the biopsy incision, the size of which was 1.0×0.5 cm. The patient
exhibited 22 mm of induration in response to the PPD skin test and
GM test (−), PPD-IgG Ab (+) and MycoDot™ (+). Chest CT showed a
nodular shadow in the dorsal segment of right lower lung, with
rough edges, thickening bilateral bronchovascular bundles and
multiple enlarged lymph nodes in the mediastinum. CT-guided
percutaneous needle lung biopsy (PNLB) and fiberoptic bronchoscopy
(FB) were performed. PNLB was performed several times, but all
attempts failed to reach the nodule, as shown by CT. The results of
FB revealed that red granulomatous materials existed at the opening
of the left main bronchus, where the submucosa was swollen and
congested. In addition, the opening of the left lingular bronchus
exhibited red granulomatous elements, without obstruction of the
lumen. However, red granulomatous materials and white necrotic
elements obstructed the opening when the biopsy was performed.
These observations were consistent with the diagnosis of bronchial
tuberculosis (lesions of the left main bronchus, left lingular lobe
and left lower lobe) and scrofula (ruptured lumens). The pathology
of the specimen showed abundant coagulative necrosis, epithelioid
nodules and a few Langhans giant cells (Fig. 2B). The AFB staining of the biopsy
specimen and lavage fluid were negative. However, considering the
patient’s poor liver function and adverse reaction of liver damage
by rifapentine, isoniazide and ethambutol, plus strong liver
protective drugs were administered. Simultaneously, the fifth cycle
of chemotherapy was initiated. During hospitalization, the
patient’s cough improved. To date, the patient’s condition has
remained stable and the AML is in remission. The patient was
monitored for one year, without tuberculosis and leukemia relapse.
The patient provided written informed consent.
Discussion
Commonly, the symptoms of tuberculosis, which
include fever, cough, lymphadenopathy and loss of appetite and
weight, are atypical (1,4), making the diagnosis more difficult.
Persistent pyrexia in patients with malignant hematological
disorders, in remission, may serve as a diagnostic marker for
tuberculosis (5). The fever of the
present patient existed prior to the diagnosis of AML and continued
from admission to the remission period. In addition, the empiric
antibiotics appeared to be inefficient, even when AML was in
remission, which led to the suspicion of other uncommon reasons,
such as tuberculosis infection.
Long-lasting hematogenous, lymphogenous,
endobronchial and local spread of the disease results in variable
radiological appearances (6).
Previously, Al-Anazi et al considered that the radiographic
appearances of tuberculosis, in descending order, were as follows:
Areas of pulmonary consolidation consistent with pneumonia; nodular
shadows consistent with pulmonary fibrosis; calcification, pleural
effusions or lymph node enlargement; and cavity formation or
miliary shadows (7). However, Chen
et al found that the typical observations of tuberculosis in
descending order of occurence were mediastinal lymphadenopathy,
pleural effusion and fibrocalcific lesions on chest imaging
(1). In a previous study of 1,161
patients admitted to hospital for tuberculosis, the cervical lymph
nodes were most frequently involved (63.3%), followed by the
mediastinal lymph nodes (26.7%) and axillary lymph nodes (8.3%)
(8). Mediastinal lymphadenopathy
may occur as a complication of pulmonary tuberculosis or as a
primary disease without pulmonary involvement (9). Lymph node tuberculosis is an important
issue in developed countries and must be considered in differential
diagnosis. In addition, negative results for the identification of
Mycobacterium tuberculosis in the lymph nodes does not
exclude the diagnosis of lymph node tuberculosis (8). With the exception of the involvement
of the lymph nodes or lungs, disseminated tuberculosis involves a
number of other organs, which may be confused with Candida
(10). In the present case, the CT
initially presented mediastinal and hilar enlarged lymph nodes,
followed by supraclavicular fossa lymphadenopathy and, thus, AML
infiltration was suspected. However, several cycles of chemotherapy
did not resolve the lymphadenopathy, even when the patient had
achieved complete remission. AML infiltration was excluded, and
nodular shadows and obstructive pneumonia appeared as the disease
became aggravated in the chest CT. Therefore, it was necessary to
differentiate between tuberculosis, fungal infection and
lymphoma.
In a previous study by Chen et al, positive
culture(s) of Mycobacterium from sputum and/or tissue were
determined as the standard for establishing the diagnosis of
tuberculosis in adults (1).
However, a number of patients had no sputum or complained only of a
dry cough when without extensive infiltration of the lung or
pleural effusion, or developed extrapulmonary tuberculosis only. In
addition, immunosuppressed patients are less likely to exhibit
positive sputum staining for AFB (6,11). In
the current case report, the patient had a prolonged dry cough and
even when the patient coughed white frothy sputum, the sputum
staining for AFB and sputum cultures for fungi and bacteria were
all negative. Bronchoalveolar lavage is reported to be an effective
technique for patients with hematological malignancies and
pulmonary tuberculosis (12).
Biopsy of the target lesion showing granulomas, positive AFB
staining and culture for mycobacteria are essential to
differentiate tuberculosis infection from other infections
(11,13). Certain previous studies have
considered polymerase chain reaction as one of the diagnostic
methods for M. tuberculosis (3,10,11).
In the present study, the pathology of biopsy specimens from the
supraclavicular fossa lymph node and lung nodular by FB showed
caseous necrosis, epithelioid cell nodules and multinuclear giant
cells. However, the staining of biopsy specimens and bronchial
lavage fluid were all negative.
Immunosuppressed patients are less likely to develop
a positive tuberculin skin test (6). However, the current patient exhibited
a marked response to the PPD skin test and PPD IgG Ab in the blood
was also positive, which aided the diagnosis of tuberculosis. Among
a number of patients with hematological malignancies, the patients
developed tuberculosis during or following consolidation or
maintenance chemotherapy (3,6,13).
For tuberculosis with hematological disorders, the main
predisposing factors were cytotoxic chemotherapy and steroid
therapy, in descending order (7).
However, in the current study, the onset of tuberculosis was prior
to the diagnosis of AML and this disseminated during chemotherapy.
The deterioration of tuberculosis may have been caused by the
immunosuppressive therapy. However, the correlation between
tuberculosis onset and AML remains unclear.
Good clinical response to tuberculosis treatment has
been reported in adult patients with underlying hematological
malignancies treated with isoniazid, rifampicin, pyrazinamide and
ethambutol for two months followed by isoniazid and rifampicin for
an additional four to 10 months (14). Occasionally, empirical
antituberculosis therapy is necessary when the clinical and
radiological features are markedly suggestive of tuberculosis,
particularly in patients living in endemic areas (7). The response to antituberculosis
treatment has been defined when patients become afebrile and the
lesions subside, which may be considered as possible evidence for
the establishment of tuberculosis (3). In the current case report, the patient
was administered three antituberculosis drugs as diagnostic
treatment prior to the definite diagnosis of tuberculosis. The
patient became afebrile later, which increased the suspicion of
tuberculosis. Due to the patient’s elevated liver enzymes, only two
antituberculosis drugs were administered and tuberculostatic
therapy was interrupted for a period of time. Additionally, the
patient demonstrated poor compliance, which delayed diagnosis and
aggravated the conditions. With the aid of the constitutive BM
infiltration, radiographic examination, morphological observations
of the two biopsies and the beneficial effect of antituberculosis
drugs, the diagnosis of tuberculosis was finally determined and the
patient’s symptoms and radiographic observations improved.
In conclusion, the current case report presents a
case of scrofula and pulmonary tuberculosis developing with AML. It
is important to distinguish tuberculosis in adults with AML from
other causes of fever, mediastinal masses in radiographic
observations and hemophagocytosis in the bone marrow. We highlight
the importance of being aware that these conditions may coexist,
and clinicians must be careful to identify the occurrence of new
and rapidly progressive symptoms in patients with an established
diagnosis, in case of adverse outcomes due to delayed diagnosis and
treatment.
References
|
1
|
Chen CY, Sheng WH, Cheng A, Tsay W, Huang
SY, Tang JL, Chen YC, Wang JY, Tien HF and Chang SC: Clinical
characteristics and outcomes of Mycobacterium tuberculosis
disease in adult patients with hematological malignancies. BMC
Infect Dis. 11:3242011.PubMed/NCBI
|
|
2
|
Gupta A, Singh M, Singh H, Kumar L, Sharma
A, Bakhshi S, Raina V and Thulkar S: Infections in acute myeloid
leukemia: an analysis of 382 febrile episodes. Med Oncol.
27:1037–1045. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Mishra P, Kumar R, Mahapatra M, Sharma S,
Dixit A, Chaterjee T, Choudhry DR, Saxena R and Choudhry VP:
Tuberculosis in acute leukemia: a clinico-hematological profile.
Hematology. 11:335–340. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
De La Rosa GR, Jacobson KL, Rolston KV,
Raad II, Kontoyiannis DP and Safdar A: Mycobacterium
tuberculosis at a comprehensive cancer centre: active disease
in patients with underlying malignancy during 1990–2000. Clin
Microbiol Infect. 10:749–752. 2004.
|
|
5
|
Iuldasheva NE, Karachunskĭ MA and Pivnik
AV: Clinical picture of tuberculosis with concomitant
hemoblastoses. Ter Arkh. 76:49–51. 2004.(In Russian).
|
|
6
|
Klossek A, Dannenberg C, Feuerhahn MR and
Körholz D: Pulmonary tuberculosis in a child receiving intensive
chemotherapy for acute myeloblastic leukemia. J Pediatr Hematol
Oncol. 26:64–67. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Al-Anazi KA, Al-Jasser AM and Evans DA:
Infections caused by Mycobacterium tuberculosis in patients
with hematological disorders and in recipients of hematopoietic
stem cell transplant, a twelve year retrospective study. Ann Clin
Microbiol Antimicrob. 6:162007.PubMed/NCBI
|
|
8
|
Geldmacher H, Taube C, Kroeger C,
Magnussen H and Kirsten DK: Assessment of lymph node tuberculosis
in northern Germany: a clinical review. Chest. 121:1177–1182. 2002.
View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Karanth N, Prabhash KP, Karanth PN, Shet
T, Banavali SD and Parikh P: Mediastinal lymphadenopathy in a
patient with previously treated T-cell acute lymphoblastic
leukaemia. Med J Aust. 188:117–118. 2008.
|
|
10
|
Lee DG, Choi JH, Kim YJ, Lee S, Min CK,
Kim DW, Lee J, Min WS, Shin WS and Kim CC: Hepatosplenic
tuberculosis mimicking disseminated candidiasis in patients with
acute leukemia. Int J Hematol. 73:119–121. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Lancioni C, LaBeaud AD, Esper F, Abughali
N and Auletta J: Pulmonary tuberculosis presenting as fever without
source in a pediatric patient with acute lymphoblastic leukemia.
Pediatr Blood Cancer. 53:1318–1320. 2009.
|
|
12
|
Cordani S, Manna A, Vignali M and Tascini
C: Bronchoalveolar lavage as a diagnostic tool in patients with
hematological malignancies and pneumonia. Infez Med. 16:209–213.
2008.
|
|
13
|
Ahn JS, Yang DH, Kim YK, Cho SH, Kim IY,
Lee JJ, Chung IJ and Kim HJ: Multiple intracranial tuberculomas
mimicking granulocytic sarcomas in acute myeloid leukemia. J Korean
Med Sci. 22(Suppl): S171–S173. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Khan B, Ahmed P, Ullah K, Hussain CA,
Hussain I and Raza S: Frequency of tuberculosis in haematological
malignancies and stem cell transplant recipients. J Coll Physicians
Surg Pak. 15:30–33. 2005.PubMed/NCBI
|