Introduction
Paraganglioma is a neoplasm that develops from the
chromaffin tissue of the sympathetic nervous system situated
outside the adrenal medulla (1). It
is also referred to as extra-adrenal pheochromocytoma.
Paragangliomas of the urinary bladder account for <1% of all
bladder tumors and 6% of all extra-adrenal pheochromocytomas
(2). Bladder paraganglioma is
similar to adrenal pheochromocytoma, the majority of which secrete
catecholamines and cause symptoms of pheochromocytoma and bladder
tumors, including headache, palpitations and fainting, which are
particularly associated with micturition and hematuria.
Paraganglioma of the urinary bladder is rarely encountered and its
biological behavior is uncertain. In addition, the prognosis of
bladder paraganglioma has not been well established. The present
study describes a 28-year-old female with non-functioning
paraganglioma of the urinary bladder and presents a supplementary
review of the previously published cases and literature.
Case report
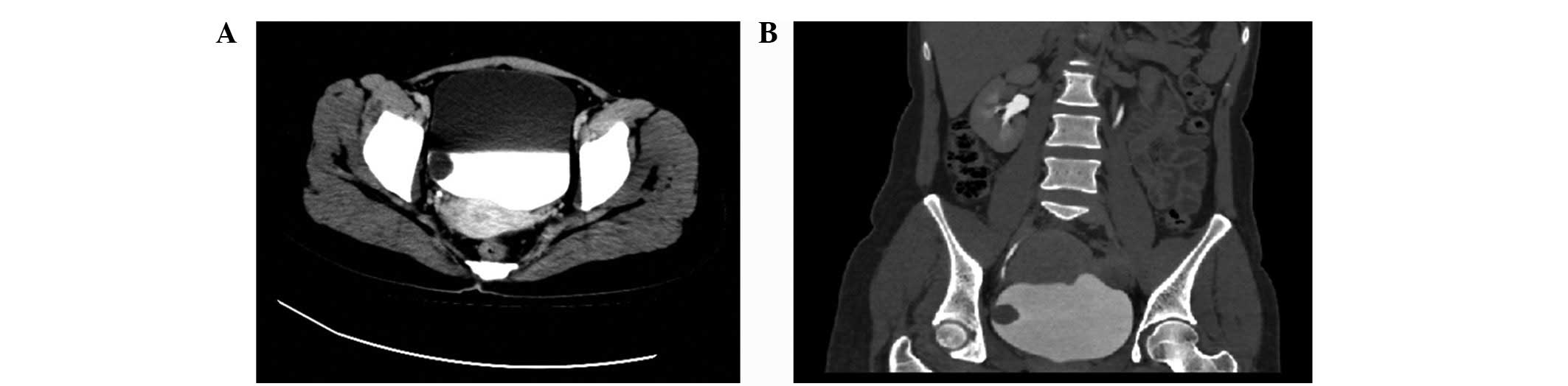
A neoplasm of the urinary bladder was identified
during a routine examination of a 28-year-old female patient, three
days later the patient was admitted to the Peking University
Shenzhen Hospital (Shenzhen, China). The patient had no abdominal
symptoms, had been in good health, with no previous medical
problems, and had no specific family past medical or drug history.
The patient did not complain of headache and had no history of
hypertension. Routine hematological examination and biochemical
tests were within normal limits and physical examination showed no
evidence of hypertensive disease. Ultrasonography revealed an
abnormal mass on the right lateral wall of the urinary bladder and
computed tomography (CT) of the abdomen showed a solitary tumor
protruding into the bladder. This was confirmed by cystoscopy
demonstrating a protruding tumor on the right wall of the bladder
with normal mucosa, measuring 2.0×2.0 cm (Fig. 1A and B). No sign of any metastatic
disease was found on ultrasound examination or CT scans of other
abdominal organ systems. On the basis of the first diagnosis of
bladder tumor, a transurethral resection was performed and the
procedure was uneventful with no hypertension or occurrence of
massive bleeding. Postoperative recovery was good and at three
months follow-up the patient felt well, with no signs of
recurrence.
Pathological examination of the tumor
indicated paraganglioma
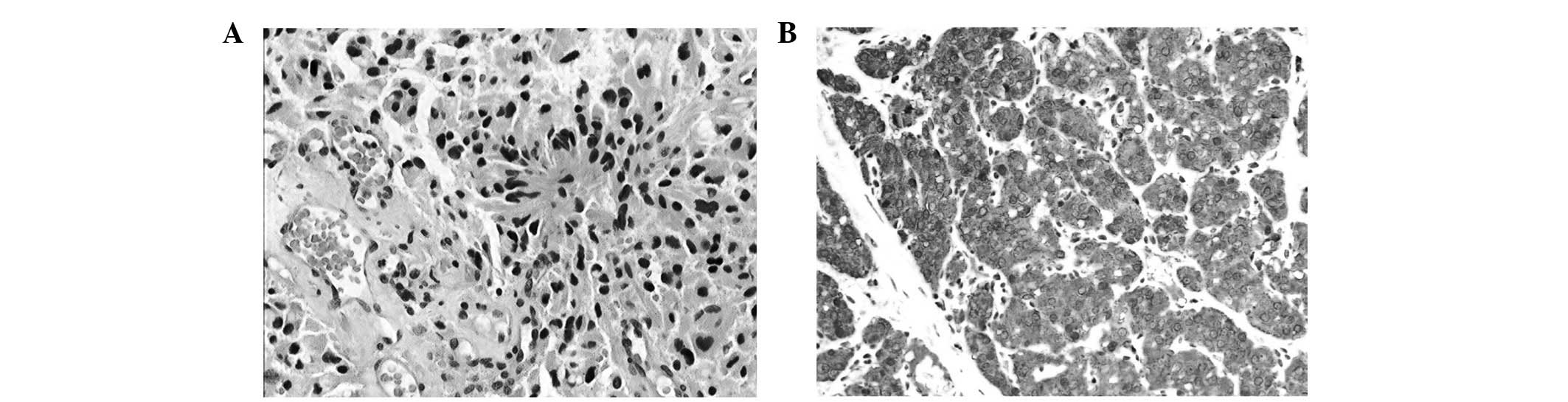
On histopathological evaluation, the tumor cells
were arranged in a nested pattern (Fig.
2A). The histopathological examination showed positive staining
for NSE, Syn, CgA and CD56, sustentacular cells stained positive
for S-100 and the Ki-67 staining revealed a proliferation index of
<2%, compatible with paraganglioma (Fig. 2B). Written informed consent was
obtained from the patient. The collection and use of clinical data
were reviewed and approved by the Peking University Shenzhen
Hospital (Shenzhen, China) Ethics Committees.
Discussion
Pheochromocytoma is a rare tumor with an estimated
800 cases diagnosed yearly in the USA, of which ~10% are
extra-adrenal or paragangliomas (1). The most common sites for paraganglioma
include the carotid body, jugular foramen, mediastinum, organ of
Zuckerkandl and periaortic region (3). Paraganglioma of the urinary bladder is
rarely encountered and non-functioning bladder paraganglioma is
even rarer. The first case of bladder paraganglioma was reported in
1953 (4). The underlying mechanism
of bladder paraganglioma remains unclear. Previous studies have
shown that bladder paraganglioma occurs more frequently in females
than males (female/male ratio is 3:1), primarily during the second
and third decades of life (5). The
majority (83%) of paragangliomas of the urinary bladder are
hormonally active (6). The main
symptoms include headache, tachycardia, sweating and paroxysmal
hypertension, particularly during micturition. Therefore, when the
presence of paraganglioma of the urinary bladder is suspected,
endocrine tests must be performed, including catecholamines and
vanillylmandelic acid in a 24-h urine sample, serum epinephrine and
others. However, non-functioning paragangliomas are rarer and more
difficult to diagnose due to their non-secreting nature (6). Clinically, the patient provided no
history of hypertension, headache or flushing that would suggest a
diagnosis of paraganglioma. Therefore, endocrine screening for
paraganglioma was not considered in the management of the patient.
However, not all patients have typical test results if blood or
urine samples are not collected at the occurrence of typical
symptoms.
Preoperative location and qualitative analysis are
extremely important in confirming the diagnosis. B ultrasound, CT
and magnetic resonance imaging may be of great use in localizing
the tumor (7–9). Ultrasound shows the tumor as a
submucosal homogeneous mass, with a clear outline, continuous
mucosa, abundant blood supply and a possible cystic or necrotic
appearance at its center. CT shows the association between the mass
and bladder mucosa and muscular and peri-tissue (7,8).
I131-methyliodobenzylguanidine (MIBG) is an analog of
norepinephrine and is absorbed by the paraganglioma tissue.
I131-MIBG has been used in diagnosing and localizing extra-adrenal
paraganglioma with a specificity close to 100% and a sensitivity
approaching 90% (10). Positron
emission tomography (PET) offers even higher accuracy than MIBG
scans in the localization of paragangliomas due to the higher
spatial resolution of PET scanning (11,12).
The tumors in cystoscopy appear as globular submucosal masses
protruding into the bladder with an intact surface, continuous
mucosa and abundant blood supply. However, the significance of
cystoscopy is limited as, when the tumor is functional, it greatly
induces blood pressure fluctuations and causes difficulties when
the bladder is irrigated, unless the necessary medicines and
instruments are available. Biopsy under cystoscopy is not
recommended since it has a low positive rate, risk of bleeding and
may provoke a hypertensive crisis.
For the majority of asymptomatic bladder
paragangliomas, a definitive diagnosis may be reached only by
histology. The tumors show histological features similar to adrenal
pheochromocytomas and the cells usually grow in a characteristic
nested Zellballen pattern. Immunohistochemical staining is required
for a definitive diagnosis. Chromogranin, synaptophysin and NSE may
aid the identification of neural tissue and neuroendocrine cells
(13). A positive staining with
synaptophysin, NSE, CD56, NSE, Syn, CgA and S-100 was observed in
the present case, which was compatible with paraganglioma. Between
5 and 15% of the paragangliomas of the urinary bladder are said to
be cancerous. However, no histological criteria have been
established to distinguish between benign and malignant tumors.
Only the appearance of local invasion or distant metastases
confirms that the tumor is cancerous (14).
The majority of paragangliomas are sporadic in
nature, but ~10% of these tumors may be associated with genetic
disorders, such as familial paraganglioma, neurofibromatosis type
1, von Hippel-Lindau, Carney triad and multiple endocrine neoplasia
type 2 (15). Therefore, it has
been suggested that all patients with extra-adrenal or multifocal
pheochromocytoma, or a family history, must undergo genetic
testing.
The most effective management is surgical resection,
including transurethral resection and partial or total cystectomy.
The perioperative preparation and treatment may not be simplified,
particularly for patients who exhibit characteristic paroxysmal
hypertension during micturition. It is necessary to stabilize
hypertension prior to surgery, using α-blocking agents
(phenoxybenzamine) or calcium channel blockers for two weeks to
inhibit the release of catecholamine and expand the blood volume,
which is similar to the management for adrenal pheochromocytoma.
Occasionally, it is difficult to determine a definitive
preoperative diagnosis, resulting in insufficient preparation,
which complicates the transurethral resection since unexpected
intraoperative hypertensive crisis and bleeding may occur (16). With the advances in laparoscopy
techniques, laparoscopic partial cystectomy has become the
treatment of choice. However, the optimal management mode remains
uncertain. Due to the multilayer involvement of the bladder wall,
open surgery to perform partial cystectomy is recommended.
Transurethral resection is considered to be feasible in tumors of
<2 to 3 cm in size without deep parietal infiltration (2). In the present case, a transurethral
resection was successfully performed. Intraoperative blood pressure
remained stable during surgery and the margins were negative for
tumor. Radiation therapy has been advocated for patients who are
unable to undergo surgery or for unresectable tumors (17).
Regular follow-up is necessary to detect late
recurrences (18). It must be
life-long and include cystoscopy, plasma or urinary tests and
imaging study. No consensus has been established for the frequency
of these measures; however, we suggested at least an annual
follow-up for those patients who are asymptomatic or whenever
clinically indicated.
Non-functioning bladder paraganglioma is easily
misdiagnosed. Transurethral resection for bladder paraganglioma may
be a treatment of choice, offering several advantages, including
reduced invasion, rapid recovery and early discharge from the
hospital, but the optimal management mode remains uncertain. A
definitive diagnosis may be reached only by histology and no
histological criteria have been established to distinguish between
benign and cancerous tumors. Long-term annual follow-up is
recommended in all paragangliomas.
Acknowledgements
This work was supported by the National Natural
Science Foundation of China (no. 81101922), the Medical Scientific
Research Foundation of Guangdong Province of China (nos. A2012584
and A2013606) and the Science and Technology Development Fund
Project of Shenzhen (no JCYJ20130402114702124).
References
|
1
|
Elder EE, Elder G and Larsson C:
Pheochromocytoma and functional paraganglioma syndrome: no longer
the 10% tumor. J Surg Oncol. 89:193–201. 2005.
|
|
2
|
Pastor-Guzmán JM, López-García S,
Giménez-Bachs JM, Ruíz-Mondejar R, Cañamares-Pabolaza L,
Atiénzar-Tobarra M, et al: Paraganglioma of the bladder:
controversy regarding treatment. Urol Int. 73:270–275.
2004.PubMed/NCBI
|
|
3
|
Lee KY, Oh YW, Noh HJ, Lee YJ, Yong HS,
Kang EY, Kim KA and Lee NJ: Extraadrenal paragangliomas of the
body: imaging features. AJR Am J Roentgenol. 187:492–504. 2006.
View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Zimmerman IJ, Biron RE and MacMahan HE:
Pheochromocytoma of the urinary bladder. N Engl J Med. 249:25–26.
1953. View Article : Google Scholar
|
|
5
|
Yadav R, Das AK and Kumar R: Malignant
non-functional paraganglioma of the bladder presenting with
azotemia. Int Urol Nephrol. 39:449–451. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Kontani K, Okaneya T and Takezaki T:
Recurrent granular cell tumour of the bladder in a patient with von
Recklinghausen’s disease. BJU Int. 84:871–872. 1999.PubMed/NCBI
|
|
7
|
Vahidi K, Joe BN, Meng M, Coakley FV and
Yeh BM: Review of atypical pelvic masses on CT and MRI: expanding
the differential diagnosis. Clin Imaging. 31:406–413. 2007.
View Article : Google Scholar
|
|
8
|
Vyas S, Kalra N, Singh SK, Agarwal MM,
Mandal AK and Khandelwal N: Pheochromocytoma of urinary bladder.
Indian J Nephrol. 21:198–200. 2011. View Article : Google Scholar
|
|
9
|
Wang H, Ye H, Guo A, et al: Bladder
paraganglioma in adults: MR appearance in four patients. Eur J
Radiol. 80:e217–e220. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Brink I, Hoegerle S, Klisch J and Bley TA:
Imaging of pheochromocytoma and paraganglioma. Fam Cancer. 4:61–68.
2005. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Pacek K, Eisenhofer G and Goldstein DS:
Functional imaging of endocrine tumors: role of positron emission
tomography. Endocr Rev. 25:568–580. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Ilias I and Pacak K: Anatomical and
functional imaging of metastatic pheochromocytoma. Ann N Y Acad
Sci. 1018:495–504. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Kovacs K, Bell D, Gardiner GW, Honey RJ,
Goguen J and Rotondo F: Malignant paraganglioma of the urinary
bladder: Immunohistochemical study of prognostic indicators. Endocr
Pathol. 164:363–369. 2005. View Article : Google Scholar
|
|
14
|
Dahia PL: Evolving concepts in
pheochromocytomas and paraganglioma. Curr Opin Oncol. 18:1–8. 2006.
View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Young WF Jr: Paragangliomas: clinical
overview. Ann N Y Acad Sci. 1073:21–29. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Ikeda M, Endo F, Shiga Y, Oguchi T, Yshi
M, Hattori K and Muraishi O: Cystoscopy-assisted partial cystectomy
for paraganglioma of the urinary bladder. Hinyokika Kiyo.
54:611–614. 2008.(In Japanese).
|
|
17
|
Srirangalingam U, Khoo B, Walker L,
MacDonald F, Skelly RH and George E: Contrasting clinical
manifestations of SDHB and VHL associated chromaffin tumours. Endoc
Relat Cancer. 16:515–525. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Maddocks RA and Fagan WT Jr: Paraganglioma
of bladder with recurrence ten years later. Urology. 7:430–432.
1976.PubMed/NCBI
|