Introduction
Primary pituitary gland cancers are rarely observed,
and when they occur, they usually arise from pre-existing,
secreting, invasive macro-adenoma (1). Adrenocorticotropic hormone (ACTH)- and
prolactin (PRL)-secreting tumours are the most common (1). Overall, <140 pituitary carcinomas
have been reported in the related English literature. The
undifferentiated type of pituitary carcinomas are reported even
less. Thus, despite the study by Furth et al which implied
that there was correlation between radiotherapy and pituitary
tumors, the true correlation between radiotherapy and pituitary
cancer remains undetermined (2).
The present study describes the case of a patient diagnosed with
pituitary cancer four months after completing surgery and
post-operative chemoradiotherapy for hypopharyngeal cancer.
Case report
A 57-year-old male was consulted at Taipei Medical
University Hospital, Taipei, Taiwan) for initial presentations of
odynophagia and dysphagia. The patient was later diagnosed with
stage IV hypopharyngeal squamous cell carcinoma. The patient
underwent a laryngopharyngectomy with left radical neck dissection
followed by post-operative concurrent chemoradiotherapy with
cisplatin 3.85 mg/kg (total dose 250 mg) and irradiation of 6,600
cGy in 33 fractions. Imaging studies prior to and during treatment
showed no abnormalities in the skull base region. However, four
months after completing the treatment, the patient developed the
symptoms of double vision and ptosis within a few days. Upon
examination, there was limited medial motion of the left eye.
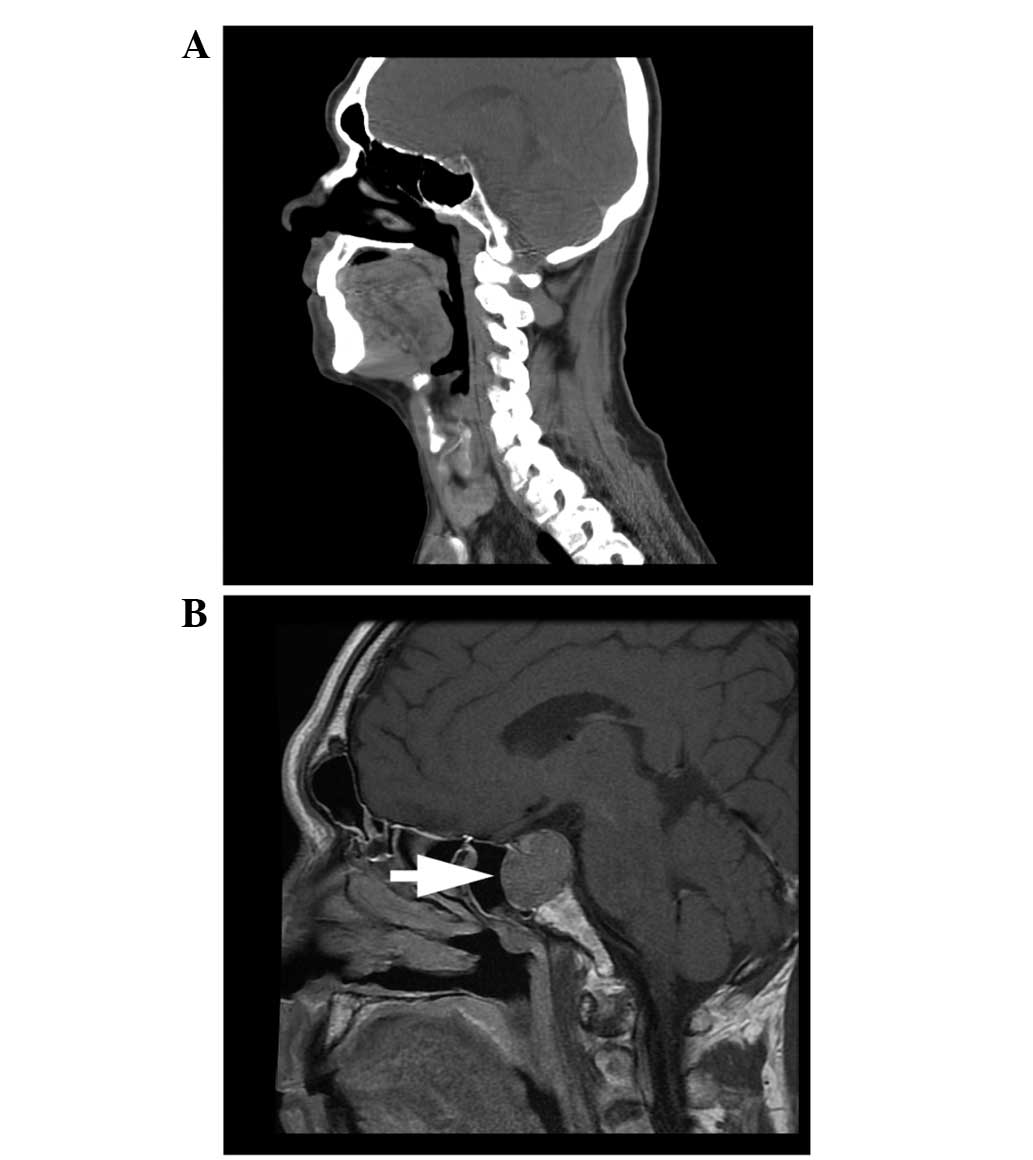
Subsequent magnetic resonance imaging (MRI) revealed a well-defined
mass at the pituitary fossa that partially obliterated the
posterior lobe (Fig. 1). Surgical
removal of the tumour was performed through a transnasal endoscopic
approach.
Grossly, the tumour appeared brown and soft
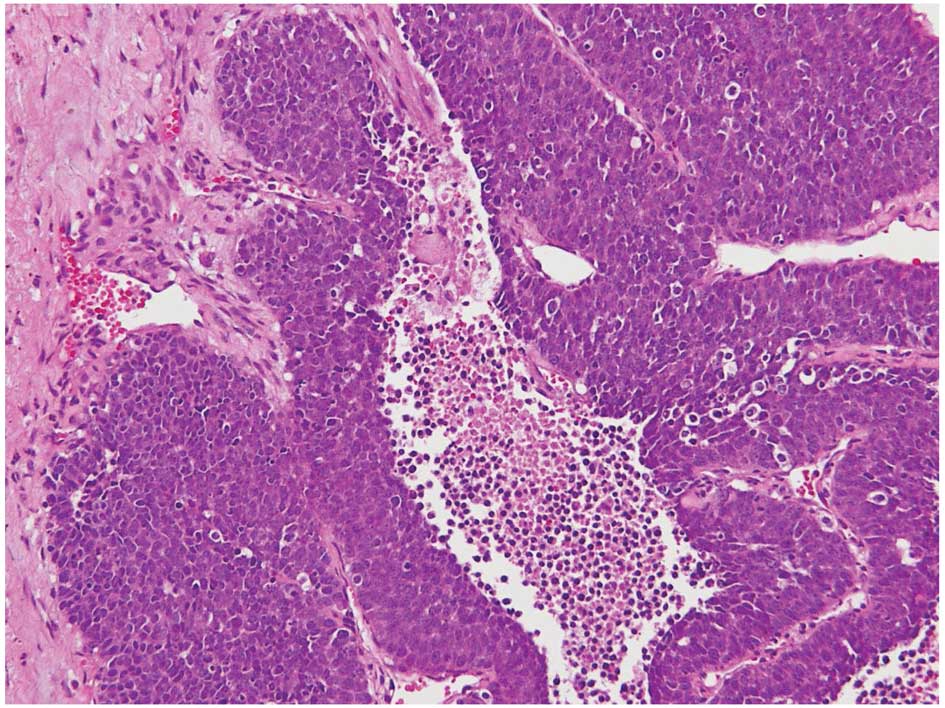
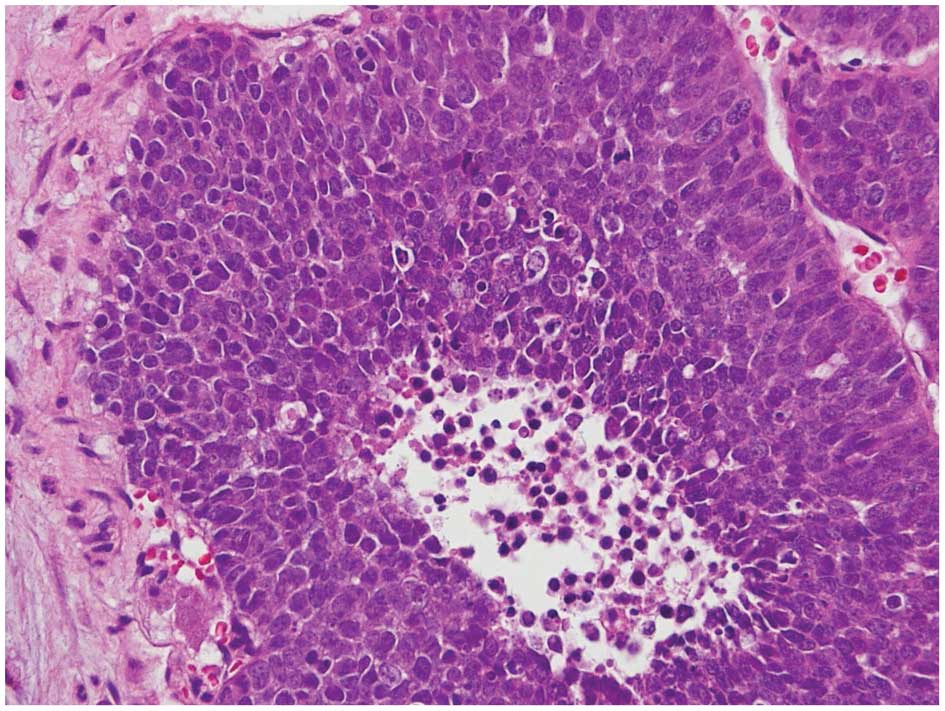
(Fig. 2). Microscopically, it
contained small blue round tumour cells in a solid sheet pattern,
with focal tumour necrosis (Fig.
3). Focal haemorrhage and multi-nucleated giant cell formation
within the stroma were also observed. The tumour cells revealed a
high nucleo-cytoplasmic ratio, hyperchromatic nuclei, occasional
nucleoli and frequent mitoses (Fig.
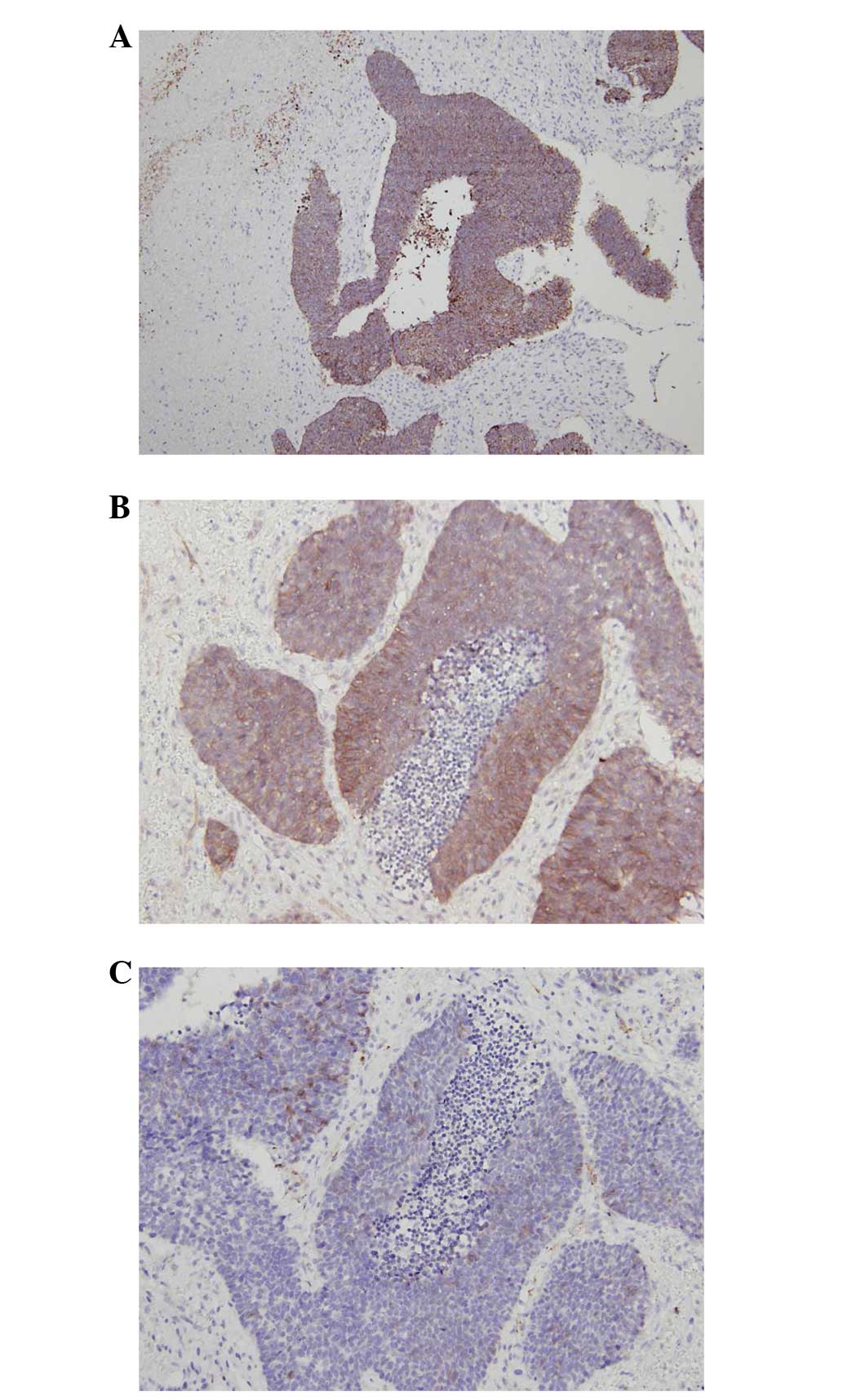
4). As observed using immunohistochemistry, the tumour cells
were diffusely weak to moderately positive for cytokeratin,
diffusely positive for cluster of differentiation (CD)117, focally
positive for CD56 and negative for cytokeratin (CK)7, CK20,
chromogranin, synaptophysin, CK5/6, p63, S-100 and CD99 (Fig. 5). Based on the morphology and
immunoprofile, the diagnosis was of a poorly-differentiated
carcinoma with focal neuroendocrine differentiation.
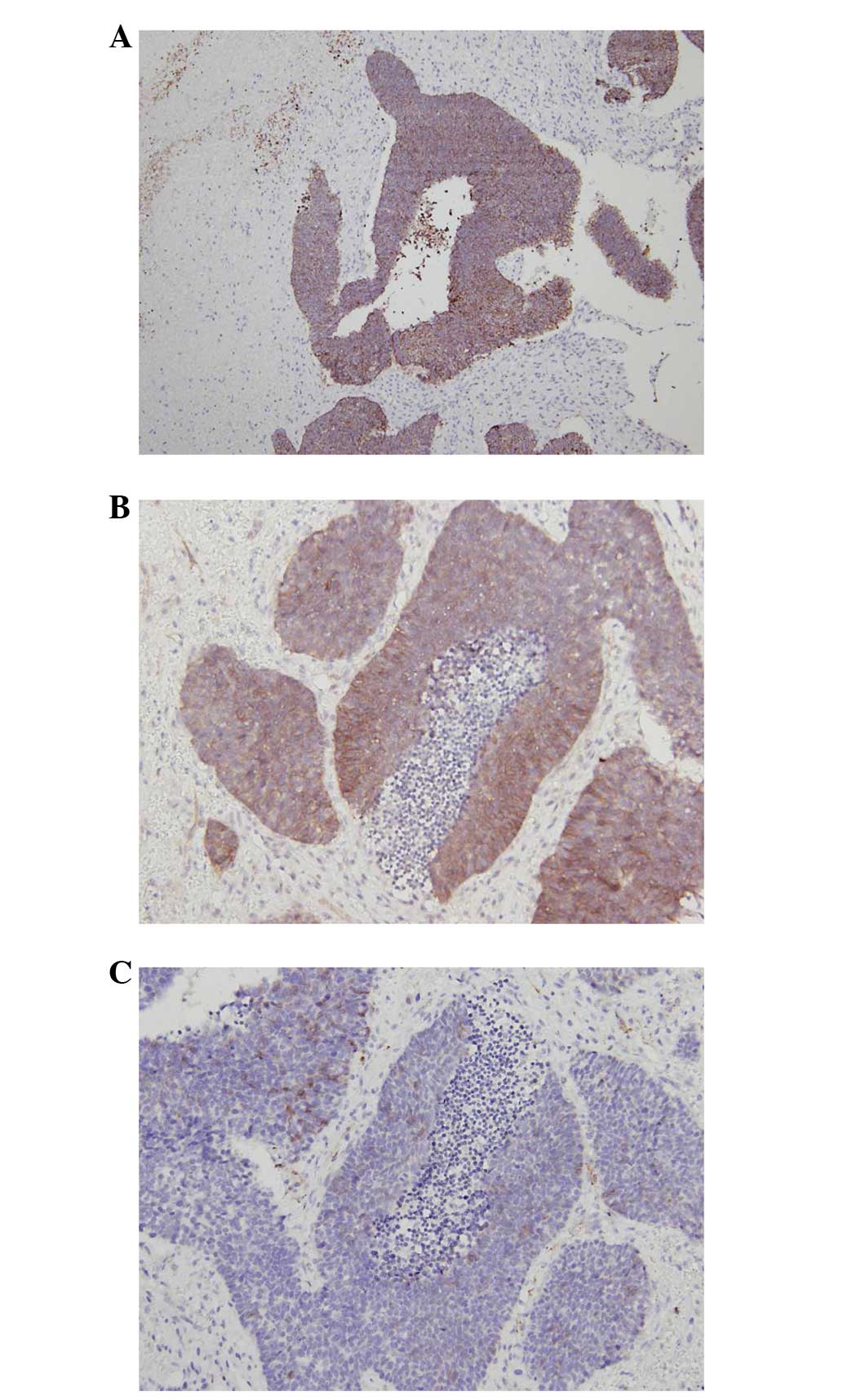 | Figure 5By immunohistochemistry, the tumour
cells were diffusely weak to moderately positive for cytokeratin
(A), diffusely positive for cluster of differentiation (CD)117
(magnification, ×100), (B) focally positive for CD56
(magnification, ×200) and (C) negative for cytokeratin (CK)7, CK20,
chromogranin, synaptophysin, CK5/6, p63, S-100 and CD99
(magnification, ×200). |
Following resection of the pituitary tumour, the
patient received six cycles of chemotherapy with dacarbazine,
epirubicin and cisplatin, and adjuvant irradiation to the skull
base of up to 5,000 cGy in 25 fractions. The tumour did not appear
to be responsive to the treatment. Primary tumour progression was
noted during the post-operative treatment, and the patient
developed bilateral vocal fold paralysis and intermittent, but
massive, nasal bleeding. Whole spine MRI revealed several bone
metastases complicated by pathological compression fractures at the
T4–T5 level, with spinal cord compression. The patient’s general
condition continued to deteriorate until he succumbed due to
multiple organ failure. Written informed consent was obtained from
the patient’s family.
Discussion
In total, ~10–20% of the general population may have
pituitary tumours (3). Of all
pituitary tumours, the most common type is a pituitary adenoma. The
diagnosis of benign, non-invasive pituitary tumours also includes
hyperplasia, adenomas, cranio-pharyngiomas, meningiomas and
pituicytomas. The prevalence of benign pituitary adenomas is ~16.7%
(4). Pituitary malignancies include
primary and metastatic cancers. Pituitary carcinomas are extremely
rare, accounting for only 0.1–0.2% of all pituitary tumours
(5). Common sites of metastasis
include local areas such as the brain, spinal cord, lepto-meninges
and cervical lymph nodes, or systemic areas, such as the liver,
ovaries and bone (5). The majority
of metastatic pituitary carcinomas originate from the breast and
lungs, although other origins include the thyroid, prostate and
salivary gland (6).
Pituitary tumours, both benign and malignant, are
usually found with the following clinical observations: i)
Oversecretion of certain hormones; and ii) subsequent ‘mass
effects’ causing visual field impairment, headaches, diplopia or
other neurological deficits (7).
However, diagnoses occasionally turn out to be based on an
incidental finding, with no clinical signs or symptoms.
Similar to benign pituitary adenomas, pituitary
carcinomas are classified into hormone-secreting, invasive
macro-adenomas and non-secreting carcinomas. Non-secreting
pituitary carcinomas usually result in symptoms caused by mass
effect. Among the secreting pituitary carcinomas, 42% produce ACTH
while others produce PRL, growth hormone (GH), luteinizing hormone,
follicle-stimulating hormone and thyroid-stimulating hormone
(1). Histological features for
primary pituitary carcinomas are significant nuclear pleomorphism
and/or hyper-chromasia with increased proliferative activity,
cytological activity and mitosis (5). Overexpression of the tumour suppressor
oncoproteins p53 and Ki-67 is noted in pituitary carcinomas and
adenomas (8). Compared with
pituitary adenomas, pituitary carcinomas present with increased
apoptosis, cyclooxygenase-2 expression and hypoxia-inducible
factor-1α expression, and lower B-cell lymphoma 2 (anti-apoptotic
factor) and p27 KIP1 levels (9).
Treatment options include tumour resection, hormone
therapy, radiotherapy and chemotherapy. Surgical resection may not
prolong survival, but it is important for providing the immediate
relief of symptoms, particularly when the mass effect is a major
concern. Surgery also aids in the accurate establishment of the
pathological diagnosis. Nonetheless, early recurrence with rapid
local growth, even after initial pituitary tumour resection, is
common. Radiotherapy may be considered for additional local tumour
control (3).
Hormone therapy with dopamine agonists (for
PRL-producing tumours) and somatostatin analogs (for GH-producing
tumours) are used to control the biochemical secretions. The
chemotherapy commonly used for pituitary carcinomas is
cyclohexyl-chloroethyl-nitrosourea, combined with 5-fluorouracil
and/or temozolomide (3).
Pituitary carcinomas are generally associated with a
poor prognosis. The mean survival time for patients is two years;
however, the majority of patients succumb within one year of the
discovery of the pituitary carcinoma (1,9).
Since the majority of pituitary malignancies arise
from pre-existing benign pituitary lesions, the pathogenesis of the
undifferentiated pituitary carcinoma of this case report is quite
difficult to understand. In the post-treatment follow-up of the
hypopharyngeal tumour, computed tomography revealed that two months
prior to the diagnosis of pituitary cancer, the pituitary fossa
appeared to be completely normal. Thus, there is suspicion of a
link between irradiation and the pituitary cancer. Post-radiation
sarcomas are already known as rare and long-term complications of
radiotherapy (10); however, few
studies discuss the topic of radiation-induced non-sarcomatous
tumours (11,12).
In the present case, the radiation exposure of the
pituitary gland during the treatment for hypopharyngeal cancer was
relatively low. Moreover, there was only a three-month latency
period for the pituitary cancer. Considering the differing nature
of sarcomas and undifferentiated carcinomas, there be a yet unknown
correlation between irradiation and the development of pituitary
cancer in this patient. More studies are warranted to clarify this
association. In the meantime, physicians should be more alert, as
irradiation may cause more damage than previously expected.
References
|
1
|
Ragel BT and Couldwell WT: Pituitary
carcinoma: a review of the literature. Neurosurg Focus. 16:E72004.
View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Furth J, Buffett RF and Haran-Ghera N:
Pathogenesis and character of radiation-induced pituitary tumors.
Acta Unio Int Contra Cancrum. 16:138–142. 1960.PubMed/NCBI
|
|
3
|
Kaltsas GA, Nomikos P, Kontogeorgos G,
Buchfelder M and Grossman AB: Clinical review: Diagnosis and
management of pituitary carcinomas. J Clin Endocrinol Metab.
90:3089–3099. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Ezzat S, Asa SL, Couldwell WT, et al: The
prevalence of pituitary adenomas: a systematic review. Cancer.
101:613–619. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Pernicone PJSB: Invasive pituitary adenoma
and pituitary carcinoma. Diagnosis and Management of Pituitary
Tumors. Thapar K, Kovacs K, Scheithauer BW and Lloyd RV: Humana
Press; Totowa, NJ: pp. 369–386. 2001
|
|
6
|
Komninos J, Vlassopoulou V, Protopapa D,
et al: Tumors metastatic to the pituitary gland: case report and
literature review. J Clin Endocrinol Metab. 89:574–580. 2004.
View Article : Google Scholar
|
|
7
|
Lake MG, Krook LS and Cruz SV: Pituitary
adenomas: an overview. Am Fam Physician. 88:319–327.
2013.PubMed/NCBI
|
|
8
|
Scheithauer BW, Kurtkaya-Yapicier O,
Kovacs KT, Young WF Jr and Lloyd RV: Pituitary carcinoma: a
clinicopathological review. Neurosurgery. 56:1066–1074.
2005.PubMed/NCBI
|
|
9
|
Sav A, Rotondo F, Syro LV, Scheithauer BW
and Kovacs K: Biomarkers of pituitary neoplasms. Anticancer Res.
32:4639–4654. 2012.PubMed/NCBI
|
|
10
|
Cahan WG: Radiation-induced sarcoma - 50
years later. Cancer. 82:6–7. 1998.
|
|
11
|
Kurwale NS, Ahmad FU, Satyarthi G, Suri A
and Mahapatra AK: Can radiation induce pituitary tumors? Giant
prolactinoma after radiation exposure. J Clin Neurosci.
15:1287–1288. 2008. View Article : Google Scholar
|
|
12
|
Lin KC, Cheng TJ, Yung JM and Kuo JR:
Malignant astrocytoma following radiation for nasopharyngeal
carcinoma: case report and review of the literature. Acta Neurol
Taiwan. 16:27–32. 2007.PubMed/NCBI
|