Introduction
Prostate adenocarcinoma is the second most common
cause of cancer-related mortality in males, affecting up to 70% of
males over the age of 80 years (1).
In total, up to 10% of patients exhibit skull and spinal
metastasis, while intramedullary spinal cord metastases (ISCMs) are
rare and account for 4–8.5% of central nervous system metastases
(2). Only one previous study of
biopsy-proven ISCM due to prostate cancer has been reported
(3). The current study presents an
additional unique case of ISCM from prostate adenocarcinoma, in
which the symptoms of conus medullaris dysfunction from the
metastasis preceded the detection of the primary tumor. To the best
of our knowledge, this is the first case in which conus medullaris
dysfunction was the first symptom (4,5). This
scenario is even more rare. The tumor was radically resected,
followed by androgen blockade treatment. The patient’s neurological
deficit significantly improved, with no tumor recurrence during the
follow-up period. However, considering the rarity of ISCM, no
previous controlled study has compared surgery, radiotherapy and
androgen deprivation. The present study provides an overview of the
previous literature concerning ISCMs from prostate cancer and
discusses the treatment options.
Case report
The patient was a 74-year-old male who complained of
numbness and hypoesthesia in the lower limbs, together with back
pain. The patient also experienced a loss of strength in the lower
extremities. All these symptoms began four months prior to
admission. Three weeks following the onset of these early-stage
symptoms, the patient experienced difficulty in walking and a
decrease in sensation from T12 to S5. Furthermore, the patient
developed dysuria and worsening sphincter dysfunction. At the time
of referral to the Department of Neurosurgery (Renji Hospital,
Shanghai, China), the patient was no longer capable of walking
alone. The patient provided written informed consent.
Examination
On admission, the patient’s mental status, cranial
nerve, upper extremities and general physical examination were
normal. Neurological examination demonstrated that the legs were
weak with hypoalgesia on both sides from T12 downwards. The
Babinski reflex was not evoked on the patient’s feet.
Neuroimaging
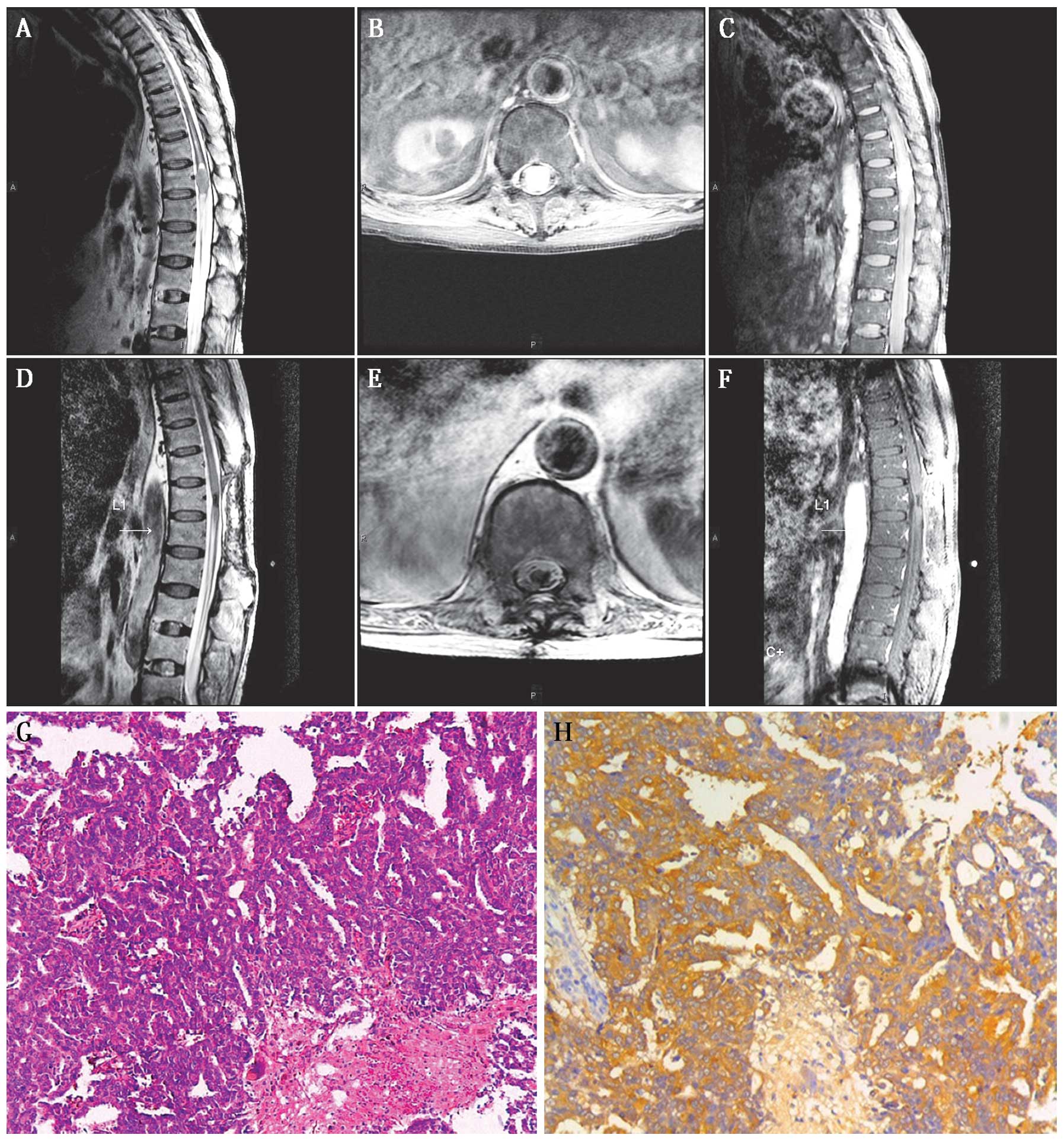
Magnetic resonance imaging (MRI) revealed a
spindle-shaped intramedullary lesion at the level of T12. A focal
expansion of the spinal cord was identified with some surrounding
edema. The lesion was ~15 mm in diameter and ~28 mm in the vertical
dimension (Fig. 1A). Following
administration of gadopentetate meglumine, the well-demarcated
lesion was enhanced (Fig. 1B and
C).
Surgery
The differential diagnosis included ependymoma,
astrocytoma or a metastasis from an additional primary tumor. Since
the patient’s neurological deficit continued to develop following
admission and the diagnosis was uncertain, a standard thoracic
laminectomy from T12 to L1 and an excisional biopsy were performed,
with somatosensory and motor-evoked potential monitoring. When the
dura was opened, an enlarged abnormal conus medullaris was
immediately identified covered by tortuous dilated blood vessels.
An intraoperative frozen biopsy demonstrated adenocarcinoma. The
abnormal tissue was radically resected without any damage to the
adjacent spinal cord tissues. When the conus medullaris appeared
adequately decompressed, an uneventful closure was performed.
Pathological observations
Microscopic examination of the surgical specimen
revealed sheets and nests of cells with abundant cytoplasm and
prominent nucleoli (Fig. 1G). The
immunohistochemical staining results were negative for
transcription factor-1, CK7, CK20, SPA, GFAP, CA19-9, Muc1, Muc4,
p53 and Vim; however, a positive reaction to prostatic acid
phosphatase was observed (Fig. 1H).
In combination with the microscopic characteristics, the pathology
was consistent with metastatic adenocarcinoma of the prostate.
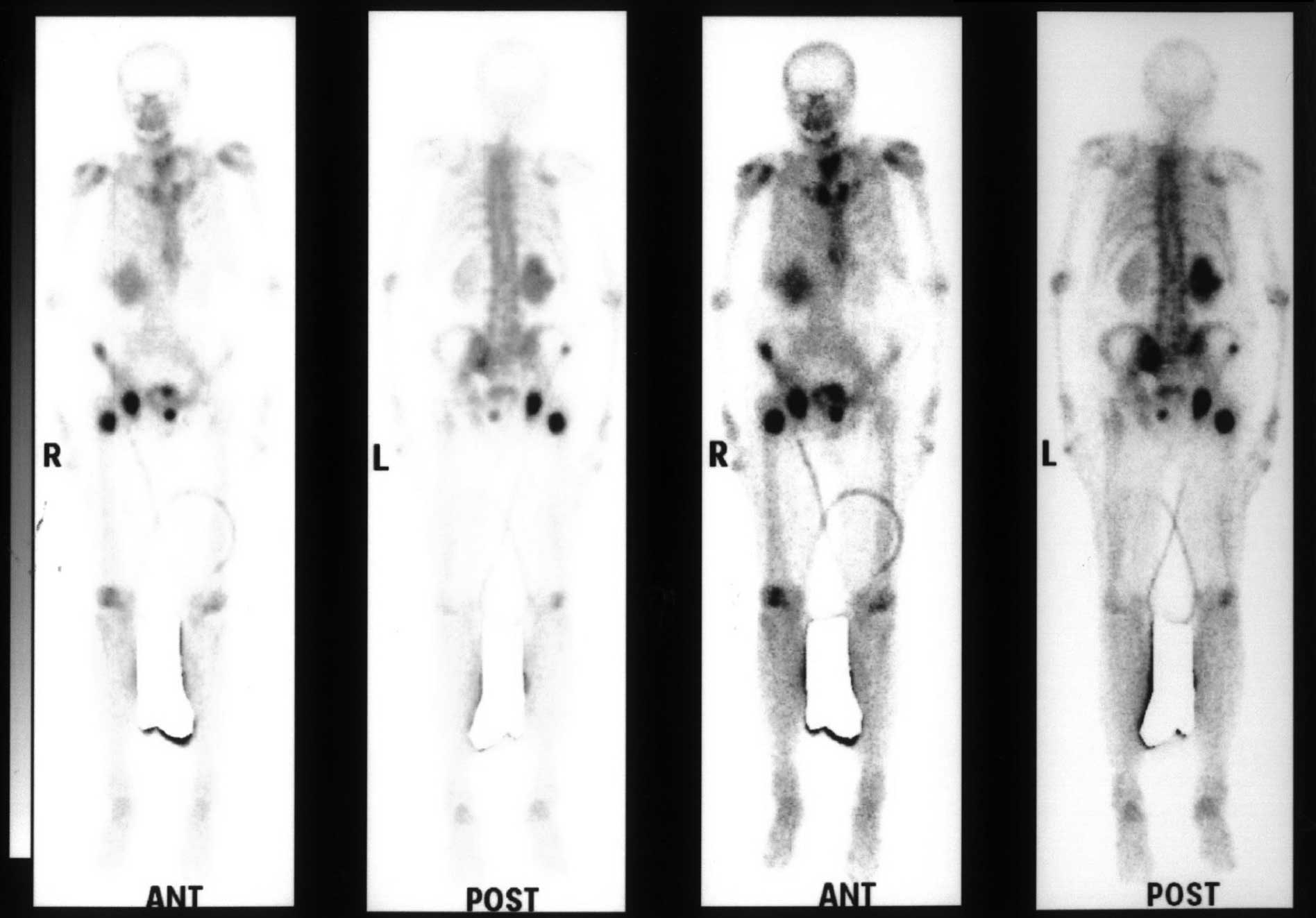
Furthermore, the patient accepted a single-photon emission computed
tomography scan, which showed multiple bone metastatic lesions
(Fig. 2).
Two weeks postoperatively
Postoperatively, the patient’s sensory disturbance
did not improve significantly, but the motor examination marginally
improved. In addition, the patient’s bowel and bladder function
remained poor; therefore, a catheter was inserted. While the tumor
was confirmed to be a metastasis of a prostate carcinoma,
radiotherapy was suggested, but the patient refused due to the high
cost. Subsequently, the patient received androgen blockade with
leuprolide, flutamide and bicalutamide without any surgery on the
prostate gland or primary tumor. No new neurological deficit was
identified when the patient was discharged two weeks following
surgery.
Six months postoperatively
During the follow-up, androgen deprivation was
continuously achieved with leuprolide, flutamide and bicalutamide.
The prostate-specific antigen levels of the patient were almost
normal, decreasing from an initial value of 22.25 to 0.47 μg/l. The
patient’s bowel and bladder function improved significantly and the
catheter was removed three months following surgery. Motor
examination showed that the neurological deficit had also improved.
A new MRI scan revealed that a cavity had formed (Fig. 1D–F) and, therefore, it was concluded
that the tumor had been radically resected during surgery with no
recurrence.
Discussion
Tumor spread occurs primarily hematogenously via the
arterial or venous system, mainly to the liver, lungs and bones.
Secondly, dissemination occurs to the subarachnoidal space via the
lymph vessels of the peripheral nerves. This route of spread is
extremely likely when the cord is affected by leptomeningeal
invasion (6). In ISCM patients,
vertebral and other epidural metastasis is common, while metastatic
intramedullary spinal cord tumors are rare. ISCM may be considered
an infrequent observation at an advanced stage of the disease,
usually accompanying the rapid progression of systemic cancer
(2). Previously, Grem et al
reported pain and weakness to be the most frequent symptoms
(7). The authors reviewed 55
patients and found that bowel and bladder dysfunction were unusual
early manifestations of intramedullary spinal cord metastasis,
possibly as the time period from the onset of the neurological
symptoms to the development of the full-blown neurological deficit
is short. The incidences of the various primary tumors were as
follows: Lung (small cell carcinoma in particular), 29–54%; breast,
11–14%; kidney, 6–9%; colorectal, 3–5%; melanoma, 6–9%; lymphoma,
4%; thyroid, 2%; and ovarian, 1%. In total, ~3% of cases are
categorized as secondary tumors to unknown primary tumors (2).
Adenocarcinoma of the prostate affects up to 70% of
males over 80 years of age and is the second most common cause of
cancer-related mortality in males (3). Meningeal carcinomatosis, brain
metastases and intradural extramedullary spinal lesions are
uncommon. Only one previous case of biopsy-proven ISCM caused by
adenocarcinoma of the prostate has been reported. However, the
majority of cases of prostate adenocarcinoma exhibit no marked
specific symptoms at the early stage. In the present case, it was
confirmed that the patient had suffered from the tumor prior to the
onset of conus medullaris dysfunction.
The median survival of patients with ISCM depends on
several conditions. It is influenced by the nature of the primary
cancer, the preoperative neurological status and the presence of
systemic and/or CNS metastases; however, the differences are mostly
without statistical significance (2). According to Schiff and O’Nill, the
median survival is four months for patients receiving radiotherapy
and two months for those not receiving radiotherapy (8). The authors’ observation is consistent
with that of Grem et al who found that >80% of patients
succumb to the disease within three months following the diagnosis
of ISCM (7).
Currently, the surgical approach is more precise and
less invasive and, thus, allows spinal cord tumor excision with an
acceptable morbidity rate (2). The
treatment of ISCM is mostly initiated to relieve pain and to
preserve or stabilize neurological function; however, it does not
extend the survival duration (5).
In total, ~80% of patients succumb to ISCM within six months;
therefore, a timely and effective microsurgery is feasible
(1). The majority of prostate
cancer tumor cells maintain androgen dependence. Hormone therapy is
the current primary treatment for metastatic prostate carcinoma,
which implies the lack of circulating testosterone to activate the
androgen receptor (AR) in tumor cells, and it may be accomplished
by a reduction in testosterone production or by AR blockade
(9). However, considering the
rarity of ISCM, no previous controlled study has compared surgery,
radiotherapy and androgen deprivation.
In a previous study analyzing a unique
adenocarcinoma in a prostate ISCM patient, the patient initially
received a partial prostatectomy and androgen blockade and accepted
decompression surgery for the ISCM. During the follow-up, the
patient was treated with CyberKnife radiosurgery and neurological
deficits remained (3). In the
current case, the patient was unaware of the severity of his
disease progression until the occurrence of dysuria and worsening
sphincter dysfunction. This is the first case in which conus
medullaris dysfunction was the first symptom onset. The patient
refused to accept the radiotherapy due to the high cost and,
therefore, only received curative resection of the metastatic tumor
and hormone therapy for the prostate adenocarcinoma. The patient
recovered well, and it appeared that radical surgery and effective
androgen blockade may also treat the prostate adenocarcinoma in
ICSM patients, particularly those with conus medullaris metastasis.
Therefore, providing patients with successful palliation and
improving their quality of life also requires multidisciplinary
strategic treatment planning.
Acknowledgements
The present study was sponsored by grants from the
Shanghai Rising-Star Program (no. 10QH1401700) supported by the
Shanghai Science and Technology Commission, and the ‘Shu Guang’
project supported by the Shanghai Municipal Education Commission
and the Shanghai Education Development Foundation, China (no.
09SG20).
References
|
1
|
Schijns O, Kurt E, Wessels P, Luijckx GJ
and Beuls EA: Intramedullary spinal cord metastasis as a first
manifestation of a renal cell carcinoma: report of a case and
review of the literature. Clin Neurol Neurosurg. 102:249–254. 2000.
View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Kalita O: Current insights into surgery
for intramedullary spinal cord metastases: a literature review. Int
J Surg Oncol. 2011:9895062011.PubMed/NCBI
|
|
3
|
Lieberson RE, Veeravagu A, Eckermann JM,
Doty JR, Jiang B, Andrews R and Chang SD: Intramedullary spinal
cord metastasis from prostate carcinoma: a case report. J Med Case
Rep. 6:1392012. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Asadi M, Rokni-Yazdi H, Salehinia F and
Allameh FS: Metastatic renal cell carcinoma initially presented
with an intramedullary spinal cord lesion: a case report. Cases J.
2:78052009. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Parikh S and Heron DE: Fractionated
radiosurgical management of intramedullary spinal cord metastasis:
A case report and review of the literature. Clin Neurol Neurosurg.
111:858–861. 2009. View Article : Google Scholar
|
|
6
|
Mut M, Schiff D and Shaffrey ME:
Metastasis to nervous system: spinal epidural and intramedullary
metastases. J Neurooncol. 75:43–56. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Grem JL, Burgess J and Trump DL: Clinical
features and natural history of intramedullary spinal cord
metastasis. Cancer. 56:2305–2314. 1985. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Schiff D and O’Neill BP: Intramedullary
spinal cord metastases: clinical features and treatment outcome.
Neurology. 47:9069–9112. 1996. View Article : Google Scholar
|
|
9
|
Arranz Arija JÁ, Cassinello Espinosa J,
Climent Durán MÁ and Rivero Herrero F; SEOM (Spanish Society of
Clinical Oncology). SEOM clinical guidelines for treatment of
prostate cancer. Clin Transl Oncol. 14:520–527. 2012.PubMed/NCBI
|