Introduction
Anal cancer is a rare tumor among gastrointestinal
tract neoplasms. Squamous cell carcinomas are the most common
subtype. The most common subtype is squamous cell carcinoma.
Basaloid squamous cell carcinoma is a rare and aggressive variant
of squamous cell carcinoma that normally arises in the upper
aerodigestive tract and less frequently in the lungs, anus, vagina
and uterine cervix (1).
Overall, ≤20% of patients present with disseminated
disease at the time of diagnosis. Brain metastasis is a rare
entity, with only a total of four cases have been previously
reported in the literature. To the best of our knowledge, this case
report presents the fifth case of anal carcinoma with brain
metastasis.
Case report
A 69-year-old male presented with a six-month
history of anorectal pain, tenesmus and an anal tumor. In addition,
the patient complained of back pain, fatigue and hyporexia. The
patient’s medical history included glaucoma and cataracts, and an
80 pack-year smoking history. A physical examination showed
hepatomegaly, a painful mass in the external anal sphincter and a
performance status of 1.
Colonoscopy found an ulcerated mass within 6 cm of
the anal verge. Pathological specimens were obtained during the
colonoscopy procedure and the histological report showed a basaloid
undifferentiated carcinoma. Staging computed tomography (CT) scans
of the chest, abdomen and pelvis exhibited mesorectal
lymphadenopathy and multiple pulmonary and liver metastases. Due to
the back pain, a bone scintigraphy was also performed and uptake
was revealed at the coccix, right sacral ala and pubis.
The patient was diagnosed with basaloid
undifferentiated carcinoma of the anal canal, stage IV (T3N2M1),
and underwent treatment in October 2011. The patient was treated
with cisplatin (75 mg/m2) and 5-fluorouracil (5FU; 750
mg/m2/day as a continuous infusion for five days). An
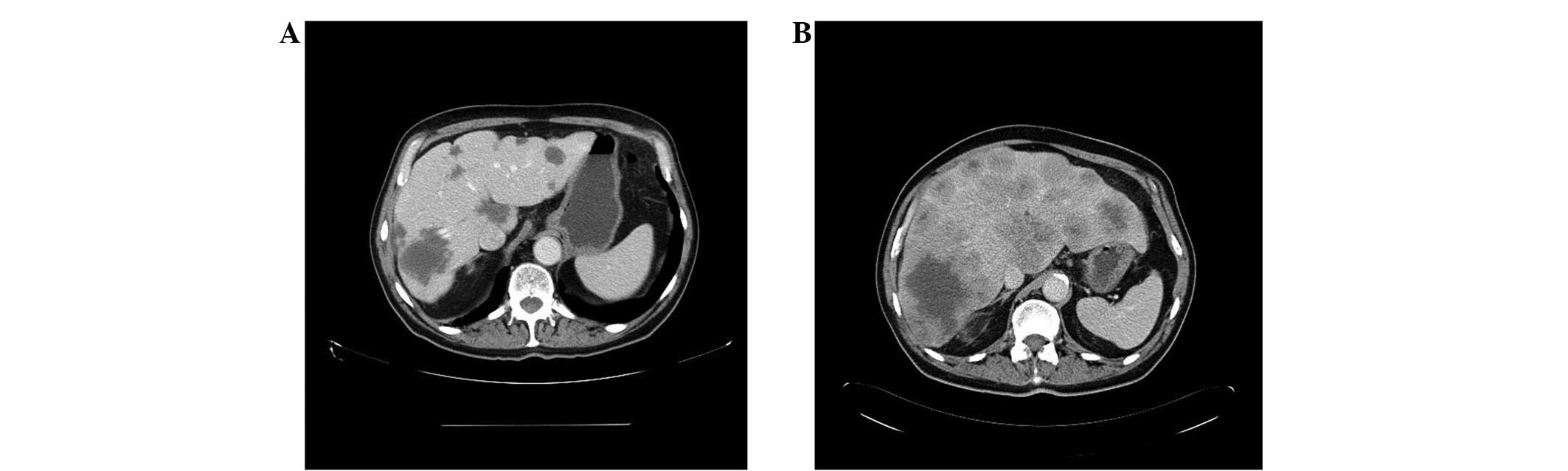
evaluation following the third and sixth cycle of treatment
recorded a partial response (Fig.
1). Toxicity included asthenia G2, nausea G1 and peripheral
neuropathy G1.
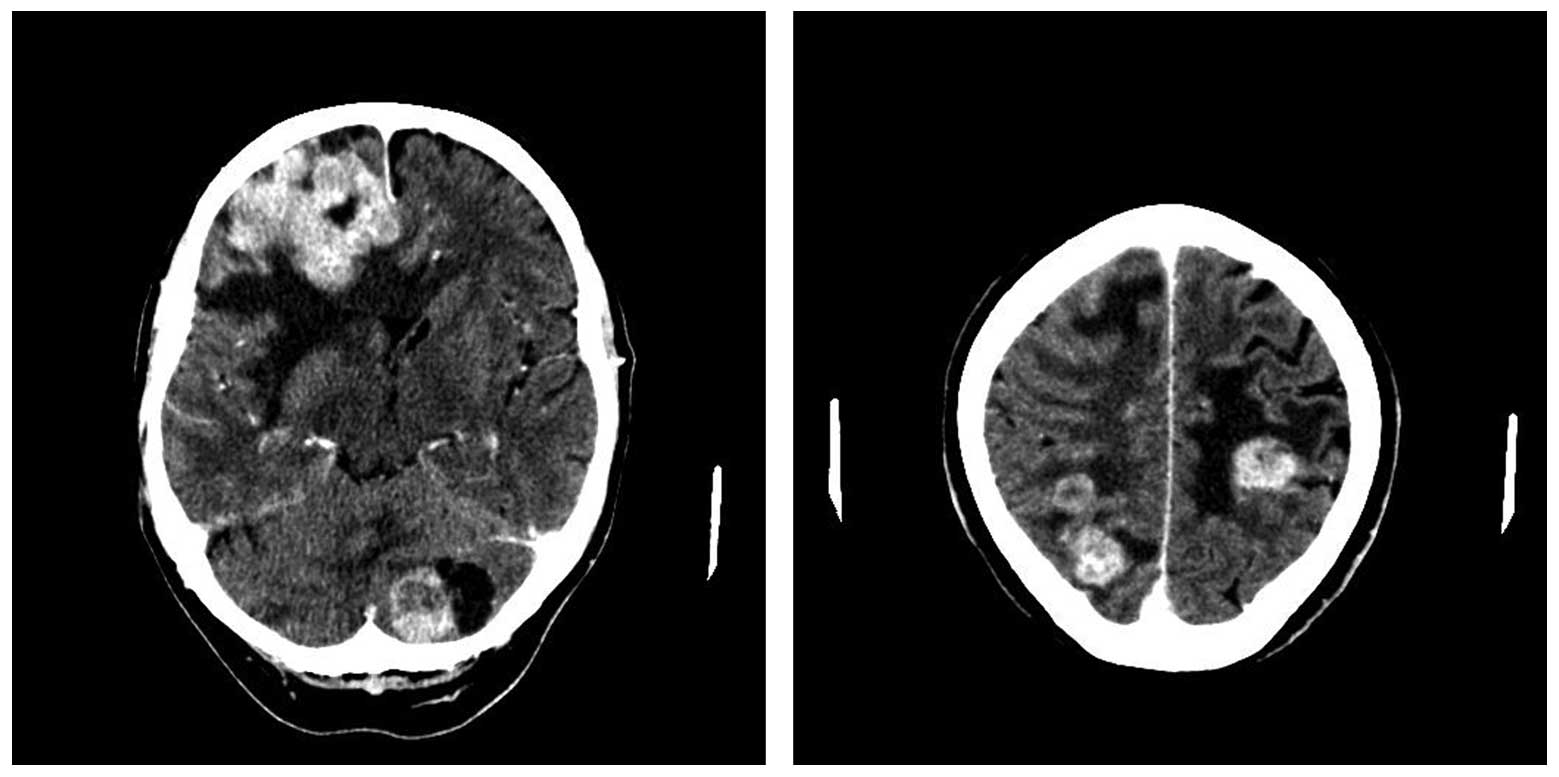
Subsequent to 14 months of follow-up after treatment
with chemotherapy, the patient developed neurological symptoms
consisting of loss of strength in the left arm that evolved to
self-limited episodes of myoclonic status, which became
generalized. Cranial CT scans found multiple lesions indicative of
metastases in the right parietal, left rolandic, cortical and
subcortical, cerebellar and frontal lobes, with tonsillar
herniation (Fig. 2). Steroid
therapy was initiated with prompt symptomatic improvement and
cranial radiotherapy was planned and delivered (30 Gy).
Despite treatment, the general condition of the
patient gradually deteriorated until they succumbed 12 weeks after
the diagnosis of brain metastasis.
Discussion
Anal cancer (including the anus, anal canal or
anorectum) accounts for 2.2% of all gastrointestinal malignancies
(2). The disease usually occurs in
the sixth decade of life. Although relatively rare, the incidence
of anal cancer is increasing due to its risk factors (3), such as anal-genital human
papillomavirus (HPV) infection, immunosuppression associated with
human immunodeficiency virus or transplantation and smoking
(4,5). HPV infection is associated with 97% of
anal cancers (6).
These tumors are divided into two categories, tumors
of the anal canal or anal margin, based on their anatomical
location. The majority of anal canal tumors are squamous cell
carcinomas (7). Although the tumors
have been traditionally divided into well-differentiated
keratinizing and non-keratinizing (cloacogenic/basaloid and
transitional) types, the two types have a similar natural history.
Therefore, no distinction has been determined in their management
(8). Other rarer types include
adenocarcinoma, anaplastic carcinoma, undifferentiated tumors and
melanomas (7).
Squamous cell carcinoma also predominates in the
anal margin subtype, which is usually well-differentiated and
keratinizing (9). Overall, squamous
carcinomas account for 75% of anal cancers (10).
Clinically presenting with rectal bleeding (45%) and
anorectal pain or urgency (30%) (10), 10–20% of patients exhibit
extrapelvic disseminated disease at the time of diagnosis. The most
important organ for metastases is the liver (12). The five-year survival rate at stage
IV is 20.9% in squamous cell carcinomas and 7.4% in non-squamous
cell carcinomas (8).
Cisplatin-based chemotherapy in combination with 5FU and paclitaxel
is the standard treatment of metastatic anal carcinoma (13), with radiotherapy provided for local
treatment (14). The presence of
epidermal growth factor receptor (EGFR) overexpression in anal
carcinoma indicates a role for anti-EGFR therapies, such as
cetuximab (15).
A total of four cases of anal cancer with brain
metastasis have been previously reported in the literature. The
first was identified in a review of 373 cases of anorectal
‘transitional cloacogenic carcinomas’ (now considered squamous cell
carcinomas) by Klotz et al (1967), however, no further data
on this case is available (16).
The following three cases were published in 1991, 2011 and 2012,
respectively (Table I).
 | Table IComparison of the only cases of brain
metastasis published in the literature to date. |
Table I
Comparison of the only cases of brain
metastasis published in the literature to date.
| First author/s
(ref) | Age, years | Gender | Histology | Stage at
diagnosis | Distant
metastasis | Initial
treatment | Months to cerebral
metastasis | Survival after brain
metastasis diagnosis, weeks | Brain metastasis
treatment |
|---|
| Klotz et al
(15) | NA | NA | Cloacogenic
(squamous) | IV | No | NA | NA | NA | NA |
| Davidson and Yong
(16) | 61 | Female | Basaloid
(squamous) | II | No | Surgery | 96 | NA | Surgery and RT |
| Rughani et al
(9) | 63 | Female | Squamous | IV | Liver | CT and RT | NA | 14 | Surgery |
| Gassman et al
(17) | 67 | Male | Squamous
undifferentiated | IV | Liver | CT, RT and
surgery | 6 | NA | RT |
| Present case | 69 | Male | Basaloid (squamous)
undifferentiated | IV | Liver, lung and
bone | CT | 14 | 12 | RT |
Davidson and Yong reported the case of a 61-year-old
female with a single brain lesion appearing eight years after
abdominoperineal amputation of non-metastatic anal carcinoma at
diagnosis. The patient was treated with surgery and adjuvant
radiotherapy with posterior recurrence of the primary tumor
(17).
Rughani et al (2011) reported the case of a
63-year-old patient with liver metastasis at diagnosis who received
chemoradiation treatment. Following treatment, the patient showed
prompt neurological symptoms and isolated brain metastasis was
identified. The patient underwent surgery and radiation therapy,
but succumbed 14 weeks later (10).
Finally, Austin Gassman et al recently
reported the case of a 67-year-old patient with a single liver
metastasis at diagnosis, who received neoadjuvant chemoradiation
therapy and subsequently underwent surgery for the primary tumor
and liver metastasis. The patient presented with blurred vision and
right ptosis three months after surgery. A tissue sample confirmed
brain metastasis. Radiotherapy was planned but was not performed as
the patient succumbed to the disease (18).
The present case had the peculiarity of being a
basaloid undifferentiated carcinoma, unlike the previous cases
which were the squamous type (although poorly differentiated). The
patient was diagnosed with metastatic disease similar to the
majority of the cases described previously. The present case had a
good response to the initial treatment with chemotherapy, achieving
a partial response maintained for 14 months. Due to the appearance
of neurological symptoms, a cranial CT scan was performed, which
revealed the first documented case of brain and cerebellar
metastasis for this condition. Despite receiving radiation therapy,
the patient clinically deteriorated until the patient succumbed 12
weeks following the diagnosis of brain metastasis.
Despite its rarity, brain metastasis must be
considered in any patient with anal cancer and neurological
symptoms. All five reported cases have been squamous carcinomas
with disseminated disease at diagnosis, with the exception of one
case. In addition, brain metastasis has been associated with a poor
prognosis. Radiation therapy may be administered with palliative
intent, alone or in combination with surgery in selected cases.
References
|
1
|
Vasudev P, Boutross-Tadross O and Radhi J:
Basaloid squamous cell carcinoma: two case reports. Cases J.
13:93512009. View Article : Google Scholar
|
|
2
|
Siegel R, Naishadham D and Jemal A: Cancer
statistics. Cancer J Clin. 62:10–29. 2012.
|
|
3
|
Johnson LG, Madeleine MM, Newcomer LM,
Schwartz SM and Dailing JR: Anal cancer incidence and survival: the
surveillance, epidemiology, and end results experience, 1973–2000.
Cancer. 101:281–288. 2004.PubMed/NCBI
|
|
4
|
Gervaz P, Calmy A, Durmishi Y, Allal AS
and Morel P: Squamous cell carcinoma of the anus - an opportunistic
cancer in HIV-positive male homosexuals. World J Gastroenterol.
17:2987–2991. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Shia J: An update on tumors of the anal
canal. Arch Pathol Lab Med. 134:1601–1611. 2010.PubMed/NCBI
|
|
6
|
Centers for Disease Control and Prevention
(CDC). Human papillomavirus-associated cancers - United States,
2004–2008. MMWR Morb Mortal Wkly Rep. 61:258–261. 2012.
|
|
7
|
Cummings BJ, Ajani JA and Swallow CJ:
Cancer of the anal region. Cancer: Principles & Practice of
Oncology. DeVita VT Jr, Lawrence TS and Rosenberg SA: 8th edition.
Lippincott Williams & Wilkins; Philadelphia, PA: pp. 1301–1314.
2008
|
|
8
|
Benson AB, Bekaii-Saab T, Chan E, Chen YJ,
Choti MA, Cooper HS, Dilawari RA, et al; National Comprehensive
Cancer Network. Anal Carcinoma Version 2. 2013, http://www.nccn.org/professionals/physician_gls/pdf/anal.pdf.
Accessed May 3, 2013
|
|
9
|
Olivier GC and Labow SB: Neoplasms of the
anus. Surg Clin North Am. 74:1475–1490. 1994.PubMed/NCBI
|
|
10
|
Rughani AI, Lin C, Tranmer BI and Jilson
JT: Anal cancer with cerebral metastasis: a case report. J
Neurooncol. 101:141–143. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Ryan DP, Compton CC and Mayer RJ:
Carcinoma of the anal canal. N Engl J Med. 342:792–800. 2000.
View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Cummings BJ: Metastatic anal cancer: the
search for cure. Onkologie. 29:5–6. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Faivre C, Rougier P, Ducreux M, Miltry E,
Lusinchi A, Lasser P, et al: 5-fluorouracile and cisplatinum
combination chemotherapy for metastatic squamous-cell anal cancer.
Bull Cancer. 86:861–865. 1999.(In French).
|
|
14
|
Benson AB III, Arnoletti JP, Bekaii-Saab
T, Chan E, Chen YJ, Choti MA, et al: Anal Carcinoma, Version
2.2012: featured updates to the NCCN guidelines. J Natl Compr Canc
Netw. 10:449–454. 2012.PubMed/NCBI
|
|
15
|
Garg M, Lee JY, Kachnic LA, Catalano PJ,
Henry DH, Cooley TP, et al; Eastern Cooperative Oncology Group
(ECOG); AIDS Malignancy Consortium (AMC). Phase II trials of
cetuximab (CX) plus cisplatin (CDDP), 5-fluorouracil (5-FU) and
radiation (RT) in immunocompetent (ECOG 3205) and HIV-positive
(AMC045) patients with squamous cell carcinoma (SCAC) of the anal
canal: Safety and preliminary efficacy results (updated after
absract submission). JAMA. 299:1914–1921. 2008.
|
|
16
|
Klotz RG Jr, Pamukcoglu T and Souilliard
DH: Transitional cloacogenic carcinoma of the anal canal.
Clinicopathologic study of three hundred seventy-three cases.
Cancer. 20:1727–1745. 1967. View Article : Google Scholar
|
|
17
|
Davidson NG and Yong PP: Brain metastasis
from basaloid carcinoma of the anal canal 8 years after
abdominoperineal resection. Eur J Surg Oncol. 17:227–230.
1991.PubMed/NCBI
|
|
18
|
Austin Gassman A, Fernando E, Holmes CJ,
Jacob C, Kapur U and Eberhardt JM: Development of cerebral
metastasis after medical and surgical treatment of anal squamous
cell carcinoma. Case Rep Oncol Med. 2012:9121782012.PubMed/NCBI
|