Introduction
Extraskeletal chondrosarcomas were first described
by Stout and Verner in 1953 (1);
however, it was not until 1972 that extraskeletal myxoid
chondrosarcoma (EMC) was histopathologically defined as its own
entity (2). EMC is provisionally
classified as a tumor of uncertain differentiation in the revised
version of the World Health Organization classification of tumors
of soft tissue and bone in 2002 (3). EMC is a relatively rare but
well-characterized tumor that accounts for <2% of all soft
tissue sarcomas (4). Approximately
80% of these tumors occur in the extremities, with 20% located in
the trunk. The lower extremity is the most common location of EMC
(4). The male to female ratio of
EMC is 2:1, with a peak occurrence in the fifth and sixth decades
(4).
This report presents two patients, one with EMC of
the buttock and the other with EMC of the knee. Both patients
provided written informed consent.
Case reports
Case 1
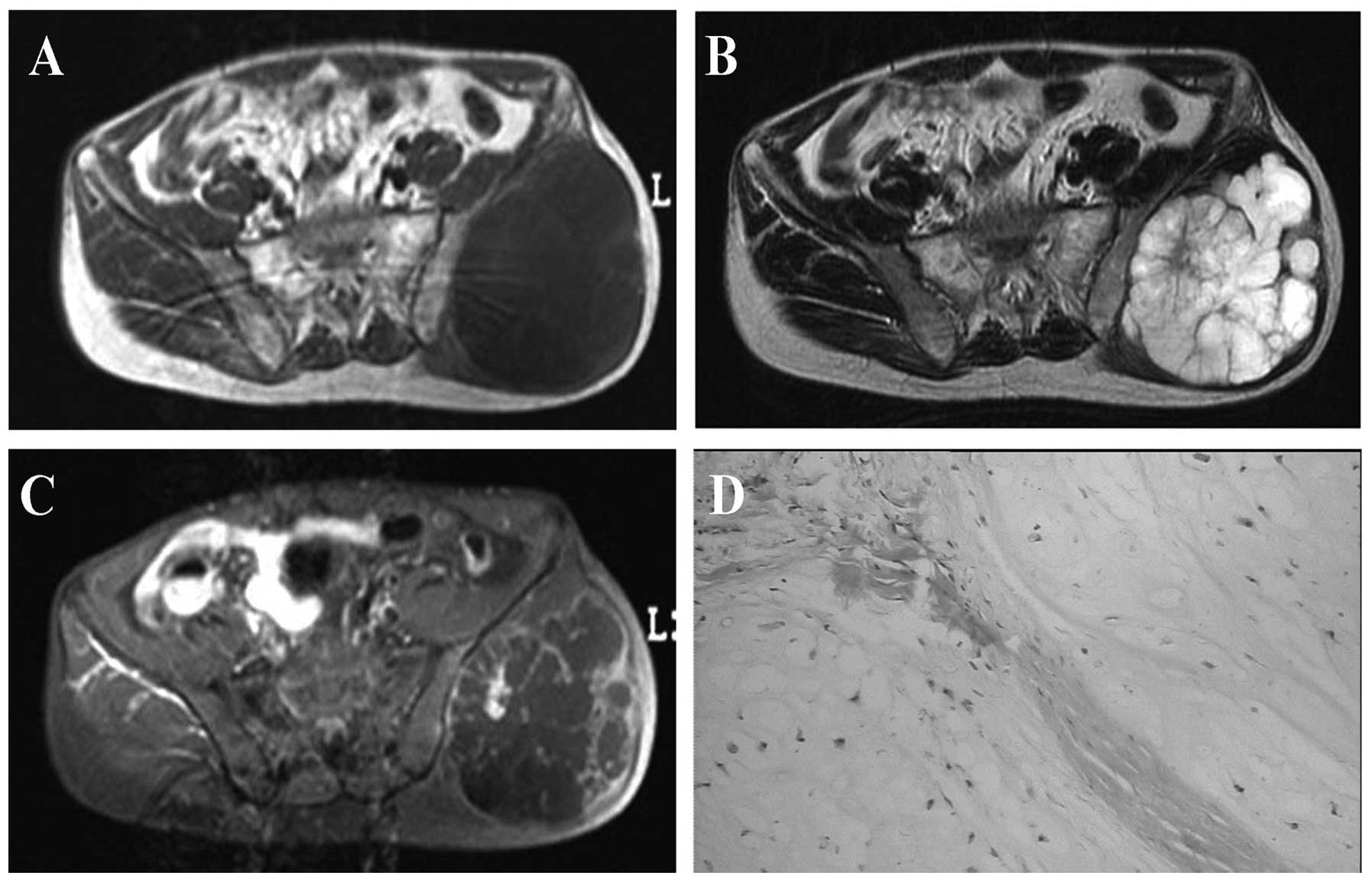
A 47-year-old man presented with a five-year history
of a painless lump in his left buttock. Six months prior to
presentation, the patient had noted that the mass had gradually
enlarged and become hard. Magnetic resonance imaging (MRI) revealed
an 8×6×6-cm sized lobular mass in the left buttock that had long T1
and T2 signal intensities. The MRI scan also revealed a uniform low
signal in the T1 weighted image (WI) (Fig. 1A) and a high signal in the T2WI,
with fat suppression and uneven signaling inside the mass and
radiated arrangement of low signaling separation in the middle of
the mass (Fig. 1B). An enhanced MRI
scan revealed an obvious and uneven enhanced mass with radiated
point bar enhancement in the middle of the mass in T1WI (Fig. 1C). In addition, the adjacent bone
showed normal signaling with mild edema of the surrounding soft
tissue. During surgery, a mass outside the left iliac bone plate
was identified. The mass comprised jelly-like tissue inside and
adhered to the surrounding sciatic nerve. The physician excised the
mass, which was located in the subcutaneous tissue and consisted of
chondroid tissue with lobes and nodular arrangement. A tissue
specimen was then sent to the pathologist for analysis. The tumor
was found to be composed of strands or cords of oval and spindle
cells embedded in abundant myxoid stroma (Fig. 1D). Pathological analysis of the
specimen concluded that the tumor was myxoid chondrosarcoma.
Case 2
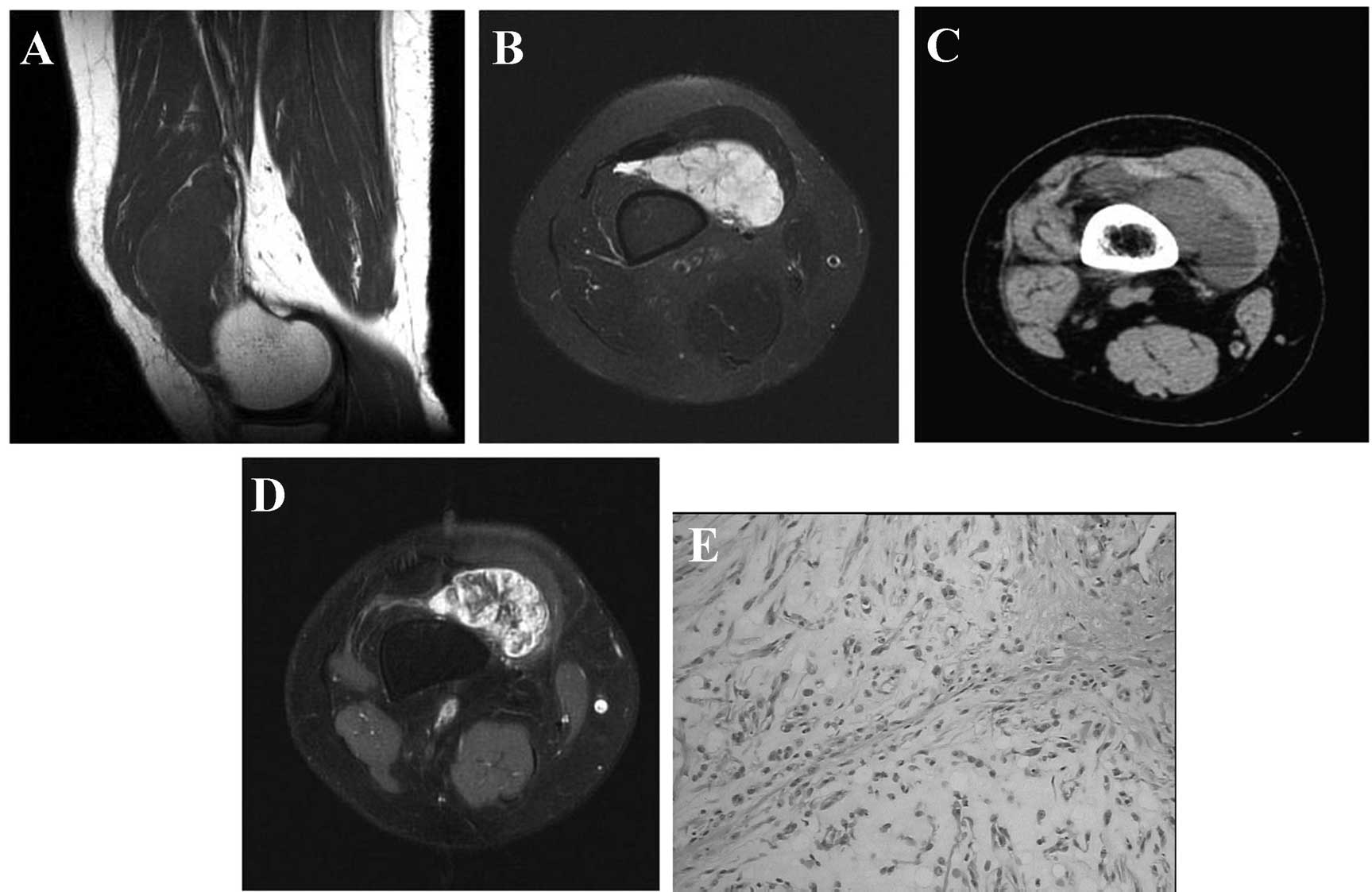
A 45-year-old woman presented with a painless lump
in her right knee for one week. Physical examination demonstrated
that the right lower extremities and knee were slightly swollen
with a palpable mass, but the patient had no difficulty in
mobilization. Computed tomography (CT) revealed an irregular-shaped
soft tissue mass measuring 8.0×6.6×3.3 cm in size located in the
right knee bursa, and the mass showed clear boundary and uniform
density (Fig. 2A). The adjacent
bone of the mass did not show obvious absorption and destruction.
MRI confirmed the presence of an irregular-shaped soft tissue mass
in right knee bursa with long T1 and T2 signaling, as well as a
uniformed low signal in T1WI (Fig.
2B) and a high signal with fat suppression in T2WI (Fig. 2C). An enhanced MRI scan revealed an
obvious uneven enhanced mass with radiated arrangement separation
enhanced like spokes in T1WI (Fig.
2D). During surgery, a mass was located in the deep surface of
the rectus femoris and vastus lateralis. The mass had the
appearance of pale yellow soft tissue and was brittle with a large
quantity of mucus. Histological examination identified that the
tumor was composed of clustered and trabecular-shaped cells in an
abundant myxoid matrix. The tumor cells had relatively uniform oval
nuclei with dense, evenly dispersed chromatin and a moderate amount
of eosinophilic cytoplasm that was often finely vacuolated
(Fig. 2E). Immunohistochemical
stains showed that the tumor cells were negative for smooth-muscle
actin (SMA), myogenin and CKpan, and positive for S-100 and
vimentin. Based on these findings, the patient was diagnosed with
EMC.
Discussion
EMC is a relatively rare neoplasm with no specific
findings in the clinic. Patients commonly present with non-specific
symptoms, including tenderness and the detection of a palpable mass
(3). The most common manifestation
of EMC is an enlarging soft tissue mass; some lesions are
accompanied by pain and tenderness, or may restrict the range of
motion. Long-term follow-up studies have shown that EMC is a slowly
growing tumor with a risk of local recurrence or distant metastasis
and disease-associated mortality (3). The lesions exhibit low density on CT,
low signal intensity on T1-weighted MRI scans and a high signal
intensity on T2-weighted MRI scans (6). Microscopically, the tumors are
characterized by a proliferation of ovoid and bipolar cells that
are enmeshed in a prominent myxoid matrix rich in chondroitin and
keratin sulfate (7,8). Immunohistochemically, the neoplastic
cells commonly stain with antibodies to vimentin and S-100 protein.
Certain studies have shown that they may also be positive for Leu-7
and epithelial membrane antigen. Uniformly, they are negative for
keratin, SMA and desmin (9,10).
This study describes two patients, one with EMC of
the buttock and one with EMC of the knee. EMC of the buttock has
rarely been reported; since its first description in 1972 (2), only a small number of cases have been
discussed. The two cases presented in this report demonstrated
large lobed masses and long T1 and T2 signals on MRI. An enhanced
MRI scan showed enhancement of the tumors. The tumors were found to
be composed of strands or cords of oval and spindle cells embedded
in abundant myxoid stroma.
The differential diagnosis of EMC is broad and
includes mucus liposarcomas and soft tissue myxomas. Mucus
liposarcomas often present as a large bump situated in the muscles,
with a clear boundary, multilocular high signaling in T2WI and
without radial low signal separation. Soft tissue myxomas belong to
the embryonic mesenchymal benign tumors. The appearance in MRI of
an intramuscular lesion with low T1 signal and high signal
intensity on fluid-sensitive sequences demonstrating a peripheral
rim of fat and edema is highly suggestive of a soft tissue myxoma
(11). The tumors present with a
clear boundary on CT scans, with uniform density and without
calcification. MRI often shows long T1 and T2 signaling, and no
obvious enhancement. In conclusion, when soft tissue masses exhibit
significantly long T1 and T2 signal intensities, lesions appear in
radial short T2 signal separation and an enhanced MRI scan reveals
enhancement of tumors, EMC should be considered as a possible
diagnosis.
References
|
1
|
Stout AP and Verner EW: Chondrosarcoma of
the extraskeletal soft tissues. Cancer. 6:581–590. 1953. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Enzinger FM and Shiraki M: Extraskeletal
myxoid chondrosarcoma: an analysis of 34 cases. Hum Pathol.
3:421–435. 1972. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Hisaoka M and Hashimoto H: Extraskeletal
myxoid chondrosarcoma: updated clinicopathological and molecular
genetic characteristics. Pathol Int. 55:453–463. 2005. View Article : Google Scholar
|
|
4
|
Smith MT, Farinacci CJ, Carpenter HA and
Bannayan GA: Extraskeletal myxoid chondrosarcoma: a
clinicopathological study. Cancer. 37:821–827. 1976. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Bhamra JS, Alorjani M, Skinner JA and
Saifuddin A: Intra-articular extraskeletal myxoid chondrosarcoma of
the ankle. Skeletal Radiol. 41:1017–1020. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Gebhardt MC, Parekh SG, Rosenberg AE and
Rosenthal DI: Extraskeletal myxoid chondrosarcoma of the knee.
Skeletal Radiol. 28:354–358. 1999. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Fletcher CD, Powell G and McKee PH:
Extraskeletal myxoid chondrosarcoma: a histochemical and
immunohistochemical study. Histopathology. 10:489–499. 1986.
View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Mackenzie DH: The unsuspected soft tissue
chondrosarcoma. Histopathology. 7:759–766. 1983. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Wick MR, Burgess JH and Manivel JC: A
reassessment of ‘chordoid sarcoma’. Ultrastructural and
immunohistochemical comparison with chordoma and skeletal myxoid
chondrosarcoma. Mod Pathol. 1:433–443. 1988.
|
|
10
|
Suzuki T, Kaneka H, Kojima K, Takatoh M
and Hasebe K: Extraskeletal myxoid chondrosarcoma characterized by
microtubular aggregates in the rough endoplasmic reticulum and
tubulin immunoreactivity. J Pathol. 156:51–57. 1988. View Article : Google Scholar
|
|
11
|
Walker EA, Fenton ME, Salesky JS and
Murphey MD: Magnetic resonance imaging of benign soft tissue
neoplasms in adults. Radiol Clin North Am. 49:1197–1217. 2011.
View Article : Google Scholar : PubMed/NCBI
|