Introduction
Inflammatory myofibroblastic tumor (IMT), also known
as an inflammatory pseudotumor, is an uncommon mesenchymal neoplasm
of intermediate malignant potential. IMT usually presents in
children and young adults and has been found to occur in numerous
locations, including the lungs, mesentery, omentum, soft tissues of
the head and neck, retroperitoneum, liver and urinary bladder
(1,2,3).
However, IMT of the digestive tract is rare and only a few cases
have previously been reported (2,3). The
current report presents one case of a 36-year-old female with an
IMT involving the colonic wall. The patient provided written
informed consent.
Case report
A 36-year-old female was hospitalized at the
Department of Infection (Huashan Hospital, Shanghai, China) due to
fever of unknown origin. The patient experienced an intermittent
fever of ≤38.5°C, which was preceded by feeling cold, however, this
was not accompanied by marked shivering or sweating; in addition,
the patient experienced slight right abdominal pain for one month.
Non-steroidal anti-inflammatory agents, such as indomethacin,
alleviated the fever. However, the body temperature of the patient
gradually increased again several hours later. The tuberculin skin
test was negative for Mycobacterium tuberculosis. The body
temperature remained abnormal following antibiotic medications,
including cephalosporin and penicillin, which were administered at
the First Affiliated Hospital of Nanchang University (Nanchang,
China) where the patient was initially admitted. The patient had no
history of serious illness, surgery or hospitalization.
On admission to the Huashan Hospital, no
abnormalities were detected on physical examination and a
laboratory evaluation revealed almost normal blood routine test
results (hemoglobin levels, 11.5 g/dl; white blood cell count,
8.57×109/litre; neutrophil count, 68%; and platelet
count, 358×109/litre). The erythrocyte sedimentation
rate and C-reactive protein levels were elevated to 120 mm/h and
159 mg/l, respectively. Electrolytes, urinalyses and renal function
tests were normal, however, liver function was abnormal (alanine
transaminase, 216 U/l; aspartate transaminase, 152 U/l;
γ-glutamyltransferase, 171 U/l; alkaline phosphatase, 281 U/l; and
lactate dehydrogenase, 314 U/l), as a result of long-term use of
antibiotics. In addition, the patient’s antistreptolysin O and
anti-Jo-1 antibodies were identified as positive. Serum markers for
hepatitis B and C, anti-dsDNA, antinuclear antibodies and
antineutrophil cytoplasmic antibodies were all negative. No
pathogens, including parasites, were observed in the stool
samples.
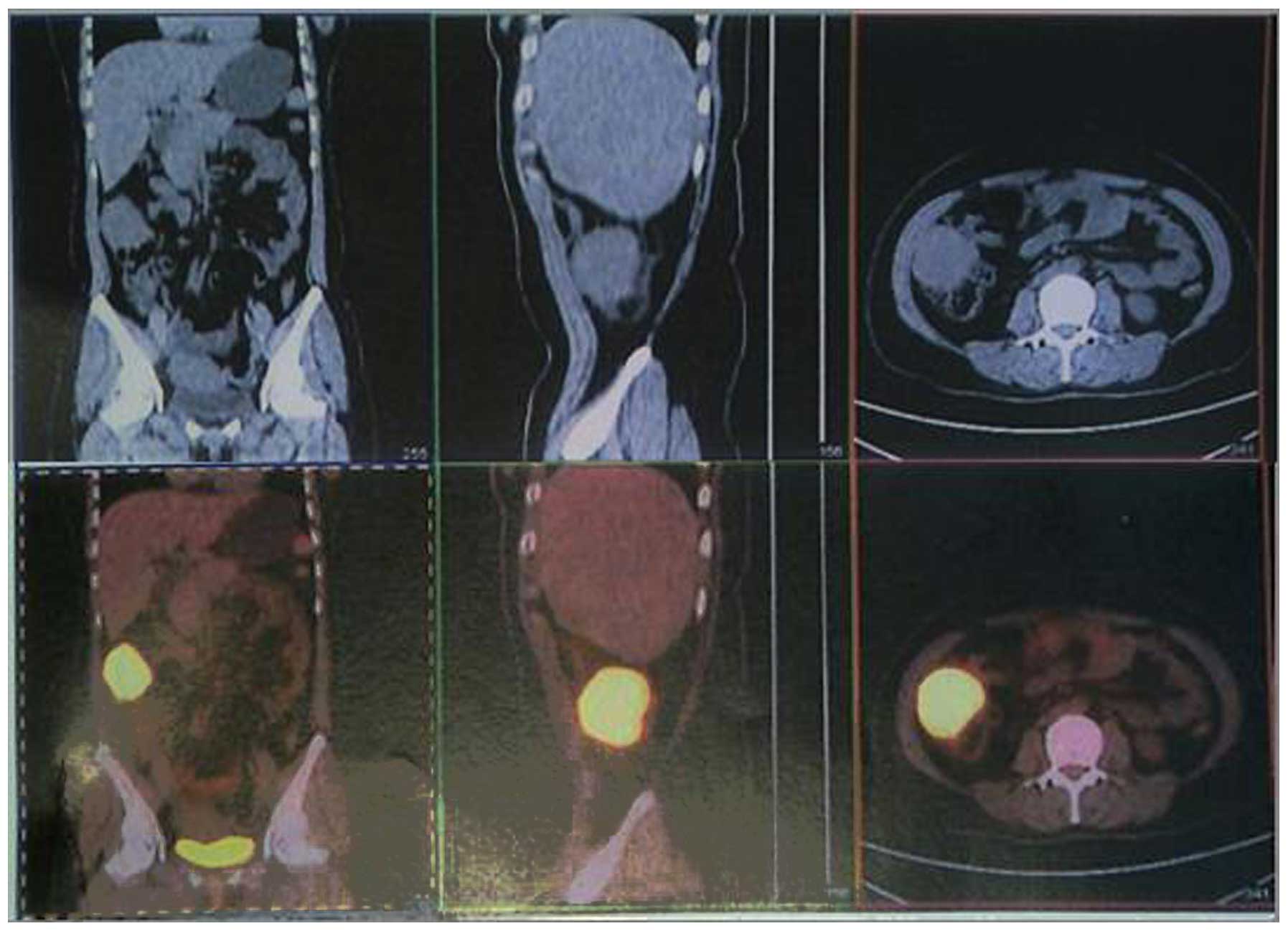
During hospitalization, the patient underwent
ultrasonography of the abdomen that showed a mass lesion with
abnormal echo in the right lower quadrant of the abdomen, which was
considered to be an inflammatory mass. This mass was confirmed by a
computed tomography (CT) scan, which localized the tumor to the
ascending colon and was considered to be a stromal tumor. In
addition, a positron emission tomography/CT scan showed an
exogenous tumor at the ascending colon (close to the hepatic
flexure), which was associated with the increased metabolism of
fluorodeoxyglucose (Fig. 1). The
radiologist diagnosed the tumor as a stromal tumor. A colonoscopy
was performed and no neoplasm was evident, however, there was a
small quantity of colon polyps.
The fever remained between 38.5 and 39°C up to and
including the day of surgery. The intraoperative examination
revealed an irregularly margined, round and rubbery mass, which
appeared to arise from the ascending colon (close to the hepatic
flexure). The mass was tightly adhered to the side of the
peritoneum, transverse colon and a section of the great omentum. A
right hemicolectomy was performed to include the region of the
tumor.
Gross examination of the primary tumor revealed an
ill-defined, smooth, glistening mass that infiltrated the colonic
wall (the intestinal mucosal surface was normal). The excised tumor
measured 6.5×4.5×4.0 cm, and the cut surface of the primary tumor
showed a white/gray lobulated mass and sections of the surface
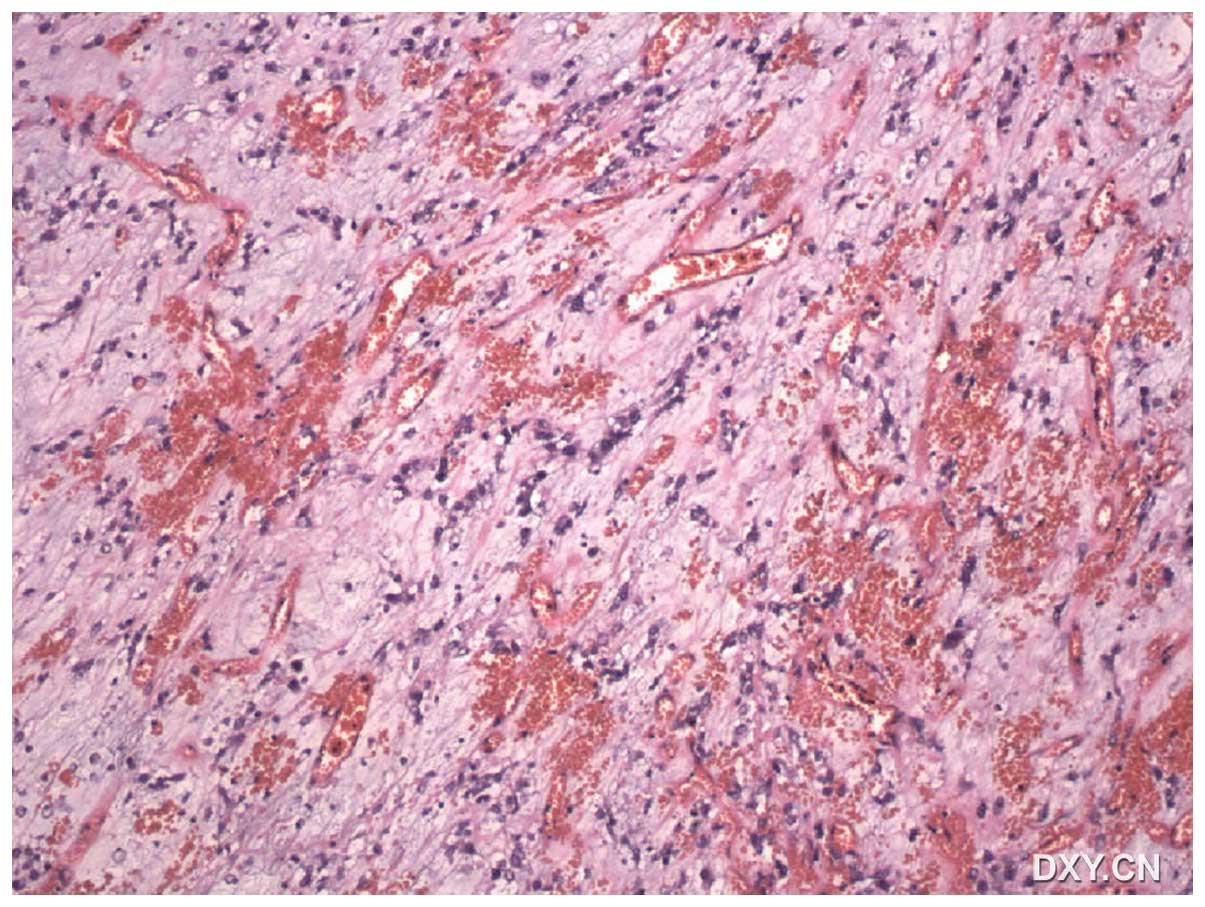
exhibited a cross-hatched appearance. Histologically, the tumor was
characterized by fibrosis and proliferation of the spindle cells.
In addition, polymorphous inflammatory infiltration of the plasma
cells, histiocytes and lymphocytes with fibroblasts were noted
(Fig. 2). The pattern of growth was
infiltrative, with the whole thickness of the colonic wall
infiltrated by the proliferating spindle cells.
Immunohistochemistry of the atypical tumor cells revealed positive
immunoreactivity for smooth muscle actin (SMA) and vimentin, and
focal immunoreactivity for cluster of differentiation (CD)34,
Ki-67, leukocyte common antigen (CD45), desmin and S-100; however,
staining for cytokeratin, CD117 and discovered on GIST (DOG)-1
protein was negative.
Furthermore, the gene test showed no mutations in
exons 9, 11, 13 or 17 of the c-KIT gene, or exons 12 or 18 of the
platelet-derived growth factor receptor A gene. The results of the
gene test combined with the negative immune reactivity of DOG-1 and
CD117 excluded the diagnosis of a gastrointestinal stromal tumor.
Leiomyoma and schwannoma were also excluded, due to the unclear
positive immunoreactivity for desmin and S-100.
The preoperative fever subsided and did not recur
until the patient was discharged. The patient was considered to be
healthy without evidence of recurrence during the one year
following surgery.
Discussion
IMT is a clinical and pathological disease entity
(1). It is an inflammatory lesion
with unknown etiology that originates from any site of the body
(2). The term IMT is used to denote
a histologically similar group of tumors, which are characterized
by spindle cell proliferation with a fibroinflammatory appearance.
IMTs have previously been reported under a variety of additional
descriptive terms, such as inflammatory fibroid polyp, inflammatory
pseudotumor, plasma cell granuloma and pseudosarcomatous
myofibroblastic proliferation (2,3).
Despite an apparently benign morphological nature, certain cases of
IMT have been reported to have a malignant clinical course,
including a locally aggressive growth and a tendency to recur
following complete resection (4).
Therefore, it is difficult to confirm an accurate diagnosis prior
to surgery (5).
Previously, Coffin et al (2) described the following three
histological patterns of IMT: i) Myxoid vascular pattern resembling
nodular fasciitis; ii) compact spindle cell pattern with a
fascicular or storiform cellular arrangement; and iii) hypocellular
collagenized pattern resembling a scar or desmoid fibromatosis. In
any case of IMT, a combination of all of these patterns may be
present or any one pattern may be predominant.
Immunohistologically, the spindle cells have been identified to be
reactive against antibodies to vimentin, SMA and muscle-specific
protein in the majority of cases (2), which is comparable to the observations
of the present study.
The majority of extrapulmonary IMTs, including
colonic IMTs, are successfully curable by surgical resection
without the development of recurrence (3,6). The
prognosis of an IMT of the digestive tract is usually good
(3), however, certain cases of IMT
that originate from other organs may show recurrence or even
metastasis following surgery (7–11). The
tendency for local recurrence appears to be associated with the
initial site of the IMT (3). For
this reason, numerous authors have recommended complete surgical
resection of the lesion as the first treatment of choice for IMTs
(3,9,12,13).
In conclusion, IMT is an extremely rare lesion that
mimics malignancy and is accompanied by various clinical
manifestations; however, they are often benign lesions and are
surgically curable. Therefore, an IMT must be considered as the
possible cause for an abdominal mass that is accompanied by various
clinical manifestations. Thus, all patients must undergo a careful
long-term follow-up due to the unknown risk of recurrence.
References
|
1
|
Batsakis JG, el-Naggar AK, Luna MA and
Goepfert H: ‘Inflammatory pseudotumor’: what is it? How does it
behave? Ann Otol Rhinol Laryngol. 104:329–331. 1995.
|
|
2
|
Coffin CM, Watterson J, Priest JR and
Dehner LP: Extrapulmonary inflammatory myofibroblastic tumor
(inflammatory pseudotumor). A clinicopathologic and
immunohistochemical study of 84 cases. Am J Surg Pathol.
19:859–872. 1995. View Article : Google Scholar
|
|
3
|
Coffin CM, Humphrey PA and Dehner LP:
Extrapulmonary inflammatory myofibroblastic tumor: a clinical and
pathological survey. Semin Diagn Pathol. 15:85–101. 1998.PubMed/NCBI
|
|
4
|
Biselli R, Ferlini C, Fattorossi A, et al:
Inflammatory myofibroblastic tumor (inflammatory pseudotumor): DNA
flow cytometric analysis of nine pediatric cases. Cancer.
77:778–784. 1996. View Article : Google Scholar
|
|
5
|
Dehner LP: The enigmatic inflammatory
pseudotumours: the current state of our understanding, or
misunderstanding. J Pathol. 192:277–279. 2000. View Article : Google Scholar
|
|
6
|
Ntloko S, Gounden A, Naidoo M, et al:
Intestinal inflammatory myofibroblastic tumour. S Afr J Surg.
49:190–193. 2011.PubMed/NCBI
|
|
7
|
Salceda J, Tayar C, Laurent A, et al:
Inflammatory pseudotumor of the liver: a case of recurrence after
resection. Acta Gastroenterol Latinoam. 43:48–52. 2013.(In
Spanish).
|
|
8
|
Zhao HD, Wu T, Wang JQ, et al: Primary
inflammatory myofibroblastic tumor of the breast with rapid
recurrence and metastasis: A case report. Oncol Lett. 5:97–100.
2013.PubMed/NCBI
|
|
9
|
Kim HB, Maller E, Redd D, et al:
Orthotopic liver transplantation for inflammatory myofibroblastic
tumor of the liver hilum. J Pediatr Surg. 31:840–842. 1996.
View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Andersen ND, DiBernardo LR, Linardic CM,
et al: Recurrent inflammatory myofibroblastic tumor of the heart.
Circulation. 125:2379–2381. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Kato S, Kondo K, Teramoto T, et al: A case
report of inflammatory pseudotumor of the lung: rapid recurrence
appearing as multiple lung nodules. Ann Thorac Cardiovasc Surg.
8:224–227. 2002.
|
|
12
|
Kovach SJ, Fischer AC, Katzman PJ, et al:
Inflammatory myofibroblastic tumors. J Surg Oncol. 94:385–391.
2006. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Sanders BM, West KW, Gingalewski C, et al:
Inflammatory pseudotumor of the alimentary tract: clinical and
surgical experience. J Pediatr Surg. 36:169–173. 2001. View Article : Google Scholar : PubMed/NCBI
|