Introduction
Chondrosarcoma is a rare disease, with an estimated
incidence of 1 in 200,000 per year (1), and occurring predominantly in the
extremities. Approximately one-third of chondrosarcomas occur in
the spine (2). Conventional
radiation therapy and chemotherapy have not been proven to be
effective in chondrosarcoma treatment (3,4), and
surgical resection remains the standard method (5–7).
Chondrosarcomas grow slowly and rarely metastasize, and they have
an excellent prognosis following en bloc resection (8). For the present patient, performing en
bloc resection was impossible, as the tumor infringed on important
vascular and nervous tissue. The current study presents a case of
cervical spinal low-grade chondrosarcoma in which the installation
of a unilateral fixation system provided cervical spinal stability
following an intralesional resection of the low-grade
chondrosarcoma. Written informed consent was obtained from the
patient for participation in this study.
Case report
A 29-year-old female was admitted to the Department
of Orthopedic Surgery (First Affiliated Hospital and Orthopedic
Institute, Soochow University, Suzhou, Jiangsu, China) presenting
with complaints of increasing pain at the back of the neck, with a
mass on the cervical spine and right upper extremity weakness for
the previous 2 months. The patient initially presented to the
hospital 3 years prior to this with soreness in the right side of
the neck lasting for 12 months. The diagnosis from an incisional
biopsy was of a low-grade chondrosarcoma of the cervical spine
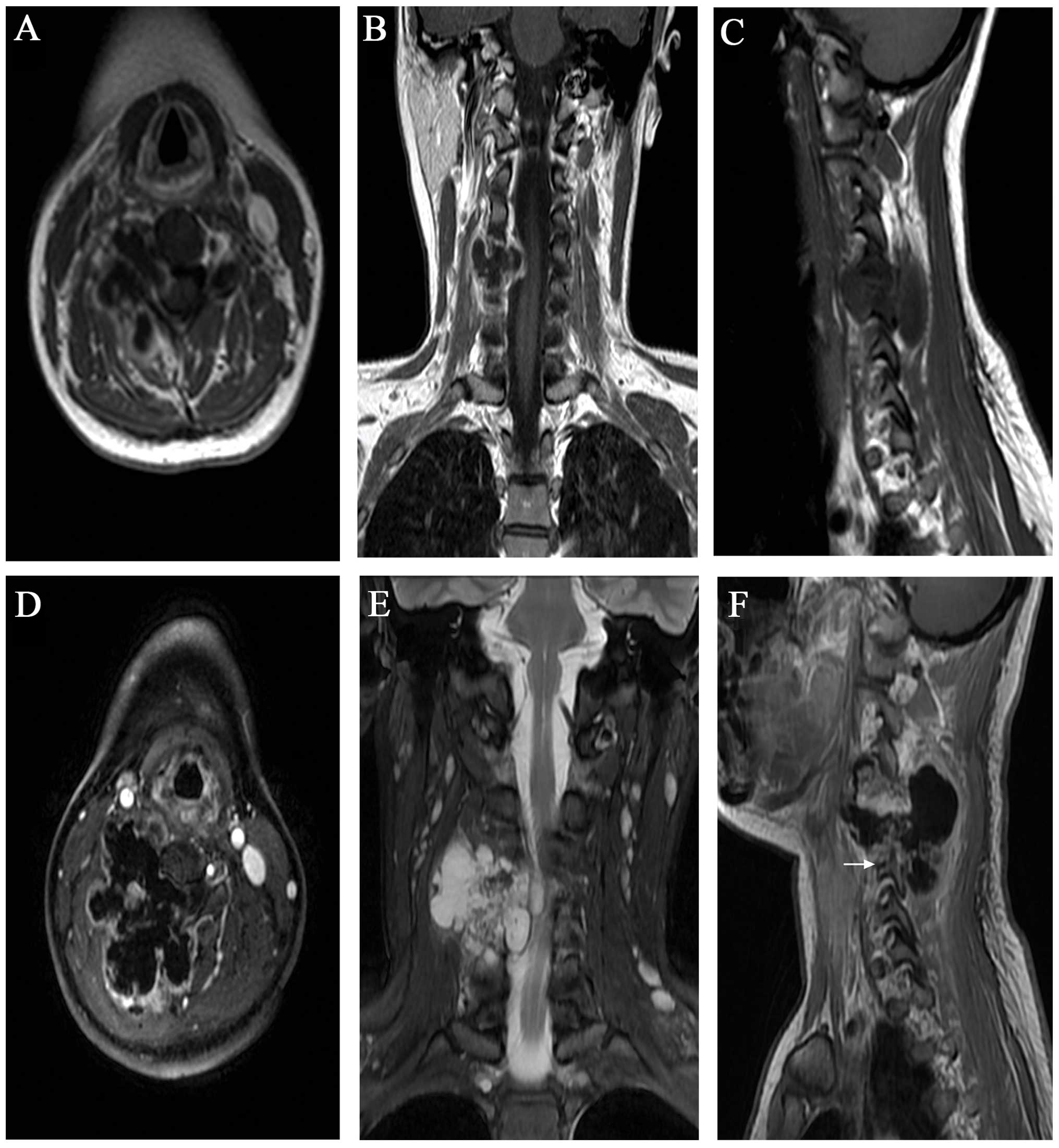
(Fig. 1A–C).
A physical examination showed that there was
weakness in the upper right extremity and hypermyotonia in the
lower extremities. Upon admission, plain radiography, computed
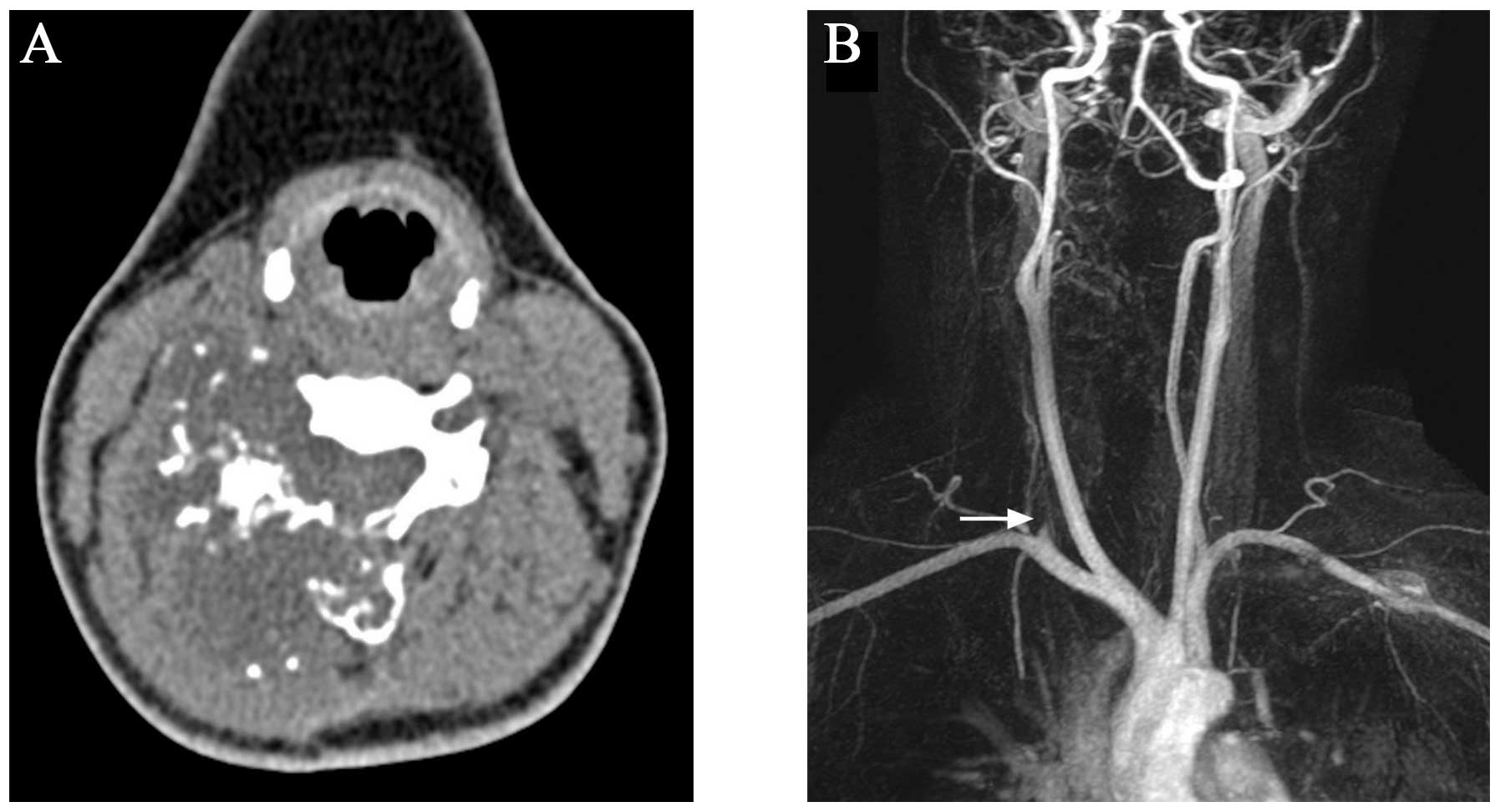
tomography (Figs. 2 and 3) and magnetic resonance imaging (Fig. 1D–F) demonstrated an expansive mass
lesion. Computed tomography scans of the chest, abdomen and pelvis
identified no other lesions. Angiography (Fig. 3B) was performed for the lesions that
were close to the vertebral artery to evaluate the displacement and
involvement of the vessels.
Embolizations were performed through digital
subtraction arteriography prior to the surgery. In the present
case, the mass had become involved with the spinal canal and had
wrapped around the vertebral artery and adhered to the root of
C4/C5 (Enneking stage IB and Weinstein-Boriani-Biagini stage
8–12/A–D). Therefore, en bloc resection with a tumor-free margin
could not be achieved. The patient received posterior surgery only,
involving piecemeal removal of the tumors, until tumor-free margins
were obtained. The bilateral arcus vertebrae and the right
articulationes zygapophysiales of C4/C5 were removed and part of
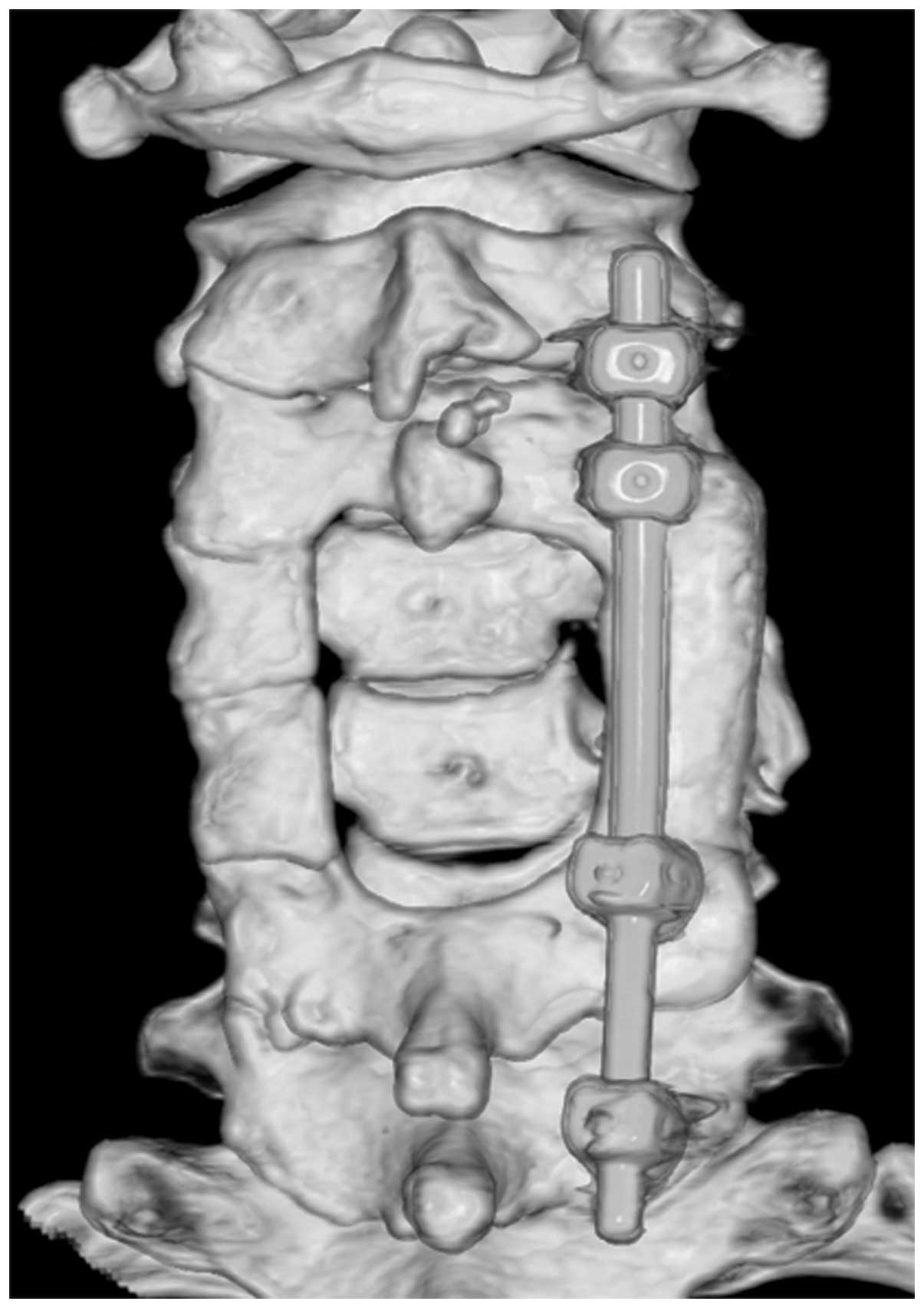
the spinous process of C3 was excised. A fixation system of screws
and rods was installed (Fig. 4) and
the axis rods were bent to match the cervical curvature. Bone
harvested form the posterior superior iliac spine was inserted as a
bone graft at the site of the lesion. Post-surgery, the patient
underwent radiotherapy (five days a week at a dose of 48 Gy for
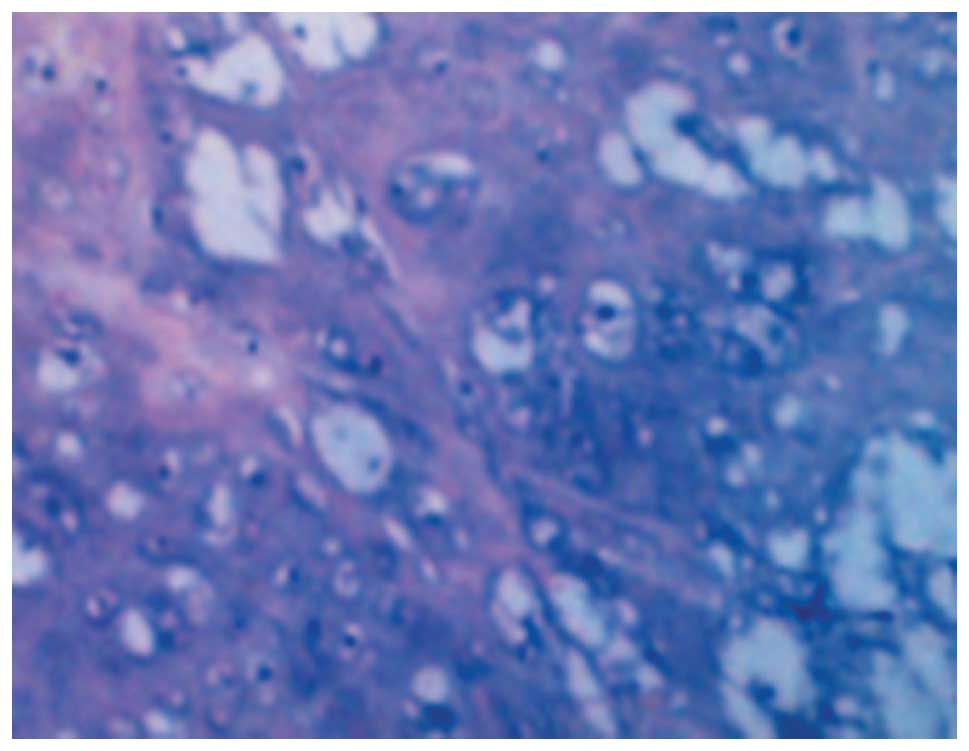
five weeks), and histopathological examination diagnosed a
low-grade chondrosarcoma (Fig. 5).
The post-operative neurological symptoms improved and therefore the
patient was discharged 10 days after the surgery. In the 2 years
following the surgery the patient had no neurological deficiency
symptoms and only a mildly uncomfortable left cervical spine
(Fig. 6).
Discussion
Pain is the most common symptom of chondrosarcoma,
and another is a palpable mass. Neurological deficits have also
been reported in half of all affected patients (9). The pain is often insidious in nature
and can be present for weeks to years (10). Low-grade chondrosarcomas grow slowly
and rarely metastasize (8,11). In the 3 years previous to the
present study, the patient did not receive surgery, chemotherapy or
radiotherapy. During the 3 years, the tumor grew by expansion to
compress the spinal cord and nerve roots and destroy the adjacent
normal tissues, including the right side of the articulationes
zygapophysiales, lamina and spinous process, without
metastasizing.
In general, with the current treatment strategies,
including local adjuvant therapy, the local recurrence rate is low
for low-grade chondrosarcoma, and there is a decrease in morbidity,
but recurrence can occur 10 years post-surgery (8). Recurrence of chondrosarcoma is usually
within 3–5 years post-surgery. If a subtotal excision resection is
performed and not en bloc resection, then the recurrence occurs
sooner (5,12). Low-grade chondrosarcoma can be
safely treated by an extended intralesional excision in the
extremity; the long-term clinical results of this method are
promising and there is satisfactory local control (5,8,13,14).
Riedel et al (13) reported
that there has been a trend of moving away from the use of wide
resection in select low-grade tumors, as a combination of a low
metastatic potential and a low local recurrence rate has been noted
for the intralesional surgery of low-grade chondrosarcoma. No
difference in the overall survival rate between the intralesional
curettage group and the wide resection group in patients with
conventional low-grade chondrosarcoma of the long bones has been
reported (15).
However, patients with lesions in the axial skeleton
have the worse prognosis when treated with intralesional resection
(5–7,11,16).
The results from these studies may be in correlation with the
complex spinal anatomy, which leads to difficulty in the thorough
excision of tumors and inadvertent intraoperative contamination
(5,17). For treatment of spinal
chondrosarcoma, surgery is critical; it should aim to preserve and
possibly improve the functionality of the spine, and to relieve
pain and control local tumor recurrence, which in turn promises a
longer survival rate (18).
En bloc resection with wide or close margins remains
the best oncological management of the spine (3,5–8,16).
A long-term survival rate has only been observed for low-grade
spinal chondrosarcoma in patients treated with repeated
intralesional excisions of the recurrent disease, combined with
radiation therapy (19). Thus, an
en bloc resection is the current recommendation for numerous
primary tumors of the thoracic, lumbar and sacral spine (17). Owing to its proximity to vital
neurovascular structures and combined with the complex spinal
anatomy, chondrosarcoma of the spine poses difficulties with regard
to the surgical procedures performed (7), and the majority of these lesions
cannot be excised in an ideal en bloc manner. If en bloc resection
is recommended for a patient, the high rate of surgical morbidity
and potential functional impairment must be weighed against
intentional tumor transgressions for functional sparing and the
consequences of tumor-margin violation (16). Virkus et al (20) demonstrated that the potential loss
of function must be seriously considered, as it has not been
definitively shown that local recurrence has an effect on the
overall patient survival rate. In the present patient, performing
an en bloc resection was impossible since the tumor was wrapped
around the right vertebral artery and was adherent to the nerve
root, therefore, an intralesional tumor resection was
performed.
The goal of this surgical procedure was adequate
neurological recovery. When laminectomy is required for spinal cord
compression, the possibility of future spinal instability must be
assessed at an early stage (21).
It has been reported that lateral mass screw fixation is a safe and
effective technique for stabilization (22). Chen et al (23) demonstrated that unilateral fixation
is good enough to maintain the stability of the device-spine
construct through an in vitro biomechanical study. The
clinical outcome and lumbar fusion rate in the unilateral pedicle
screw fixation were almost identical with those in the bilateral
method, as reported by Suk et al (24). In comparison to the bilateral
variable screw placement model, Goel et al (25) concluded that the unilateral system
was more likely to reduce the stress shielding of the vertebral
bodies and was less rigid. In the present patient, the disc was
intact without degeneration and the left articulationes
zygapophysiales was undamaged. We hypothesized that unilateral
lateral mass fixation was sufficient to reconstruct the stability
of the spine.
In accordance with the requirements of the patient,
the unilateral fixation was performed. Xue et al (26) reported that the unilateral pedicle
screw instrumented transforaminal lumbar interbody fusion neither
decreased the fusion rate nor increased the complication rate. The
present patient felt only mild discomfort in the left cervical
spine and has so far been disease-free for 2 years
post-surgery.
Unilateral fixation can provide spinal stability,
although the mechanical characteristics of the local change are
unknown, which may cause patients to feel uncomfortable. If
unilateral cervical fixation can provide enough stability, it may
present as a possible treatment option for unilateral cervical
spine injury caused by trauma. A clinical study is required to
determine the biomechanical characteristics of unilateral fixation.
As the patient follow-up time of this condition is not long enough,
the long-term effect remains to be observed.
For curative intentions, doses of >60 Gy are
required to achieve local control (8). Harwood et al (27) indicated the necessity of delivering
a dose of >50 Gy in order to have an impact on chondrosarcoma.
Great care must be taken in planning the volume applied to tumors
arising in the sacrum, vertebrae or ribs close to the vertebral
colon. For tumors that have spread into the spinal canal, a dose of
48 Gy should be chosen.
In conclusion, chondrosarcoma is generally a
low-grade, slow-growing tumor, which rarely metastasizes. Low-grade
chondrosarcoma can be safely treated with intralesional curettage
without increasing the risk for local recurrence or metastatic
disease in the extremities. Pre-operative planning for surgical
tumor removal and spine stabilization is mandatory. Although
unilateral lateral mass fixation can provide spinal stability,
determination of the biomechanical characteristics is required in
future studies.
References
|
1
|
Giuffrida AY, Burgueno JE, Koniaris LG, et
al: Chondrosarcoma in the United States (1973 to 2003): an analysis
of 2890 cases from the SEER database. J Bone Joint Surg Am.
91:1063–1072. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Sakayama K, Kawatani Y, Kidani T, Sugawara
Y, Miyazaki T, Fujibuchi T and Yamamoto H: Dumbbell-shaped
chondrosarcoma that primarily developed in the cervical spine: a
case report. J Orthop Sci. 9:166–170. 2004. View Article : Google Scholar
|
|
3
|
Katonis P, Alpantaki K, Michail K,
Lianoudakis S, Christoforakis Z, Tzanakakis G and Karantanas A:
Spinal chondrosarcoma: a review. Sarcoma. 2011:3789572011.
View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Lee FY, Mankin HJ, Fondren G, Gebhardt MC,
Springfield DS, Rosenberg AE and Jennings LC: Chondrosarcoma of
bone: an assessment of outcome. J Bone Joint Surg Am. 81:326–338.
1999.PubMed/NCBI
|
|
5
|
Boriani S, De Iure F, Bandiera S,
Campanacci L, et al: Chondrosarcoma of the mobile spine: report on
22 cases. Spine (Phila Pa 1976). 25:804–812. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Schoenfeld AJ, Hornicek FJ, Pedlow FX, et
al: Chondrosarcoma of the mobile spine: a review of 21 cases
treated at a single center. Spine (Phila Pa 1976). 37:119–126.
2012. View Article : Google Scholar
|
|
7
|
Yang X, Wu Z, Xiao J, et al:
Chondrosarcomas of the cervical and cervicothoracic spine: surgical
management and long-term clinical outcome. J Spinal Disord Tech.
25:1–9. 2012. View Article : Google Scholar
|
|
8
|
Gelderblom H, Hogendoorn PC, Dijkstra SD,
et al: The clinical approach towards chondrosarcoma. Oncologist.
13:320–329. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Quiriny M and Gebhart M: Chondrosarcoma of
the spine: a report of three cases and literature review. Acta
Orthop Belg. 74:885–890. 2008.PubMed/NCBI
|
|
10
|
Stuckey RM and Marco RA: Chondrosarcoma of
the mobile spine and sacrum. Sarcoma. 2011:2742812011. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Bergh P, Gunterberg B, Meis-Kindblom JM
and Kindblom LG: Prognostic factors and outcome of pelvic, sacral,
and spinal chondrosarcomas: a center-based study of 69 cases.
Cancer. 91:1201–1212. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
York JE, Berk RH, Fuller GN, Rao JS,
Abi-Said D, Wildrick DM and Gokaslan ZL: Chondrosarcoma of the
spine: 1954 to 1997. J Neurosurg. 90(1 Suppl): 73–78.
1999.PubMed/NCBI
|
|
13
|
Riedel RF, Larrier N, Dodd L, Kirsch D,
Martinez S and Brigman BE: The clinical management of
chondrosarcoma. Curr Treat Options Oncol. 10:94–106. 2009.
View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Hickey M, Farrokhyar F, Deheshi B,
Turcotte R and Ghert M: A systematic review and meta-analysis of
intralesional versus wide resection for intramedullary grade I
chondrosarcoma of the extremities. Ann Surg Oncol. 18:1705–1709.
2011. View Article : Google Scholar
|
|
15
|
Leerapun T, Hugate RR, Inwards CY, Scully
SP and Sim FH: Surgical management of conventional grade I
chondrosarcoma of long bones. Clin Orthop Relat Res. 463:166–172.
2007.PubMed/NCBI
|
|
16
|
Boriani S, Saravanja D, Yamada Y, et al:
Challenges of local recurrence and cure in low grade malignant
tumors of the spine. Spine (Phila Pa 1976). 34(22 Suppl): S48–S57.
2009. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Matsumoto Y, Takahashi Y, Harimaya K, et
al: Dedifferentiated chondrosarcoma of the cervical spine: a case
report. World J Surg Oncol. 11:322013. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Rao G, Suki D, Chakrabarti I, Feiz-Erfan
I, Mody MG, et al: Surgical management of primary and metastatic
sarcoma of the mobile spine. J Neurosurg Spine. 9:120–128. 2008.
View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Ozaki T, Lindner N, Hillmann A, et al:
Influence of intralesional surgery on treatment outcome of
chondrosarcoma. Cancer. 77:1292–1297. 1996. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Virkus WW, Marshall D, Enneking WF and
Scarborough MT: The effect of contaminated surgical margins
revisited. Clin Orthop Relat Res. 397:89–94. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Camins MB, Duncan AW, Smith J and Marcove
RC: Chondrosarcoma of the spine. Spine (Phila Pa 1976). 3:202–209.
1978. View Article : Google Scholar
|
|
22
|
Sekhon LH: Posterior cervical lateral mass
screw fixation: analysis of 1026 consecutive screws in 143
patients. J Spinal Disord Tech. 18:297–303. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Chen HH, Cheung HH, Wang WK, Li A and Li
KC: Biomechanical analysis of unilateral fixation with interbody
cages. Spine (Phila Pa 1976). 30:E92–E96. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Suk KS, Lee HM, Kim NH and Ha JW:
Unilateral versus bilateral pedicle screw fixation in lumbar spinal
fusion. Spine (Phila Pa 1976). 25:1843–1847. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Goel VK, Lim TH, Gwon J, et al: Effects of
rigidity of an internal fixation device. A comprehensive
biomechanical investigation. Spine (Phila Pa 1976). 16(3 Suppl):
S155–S161. 1991. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Xue H, Tu Y and Cai M: Comparison of
unilateral versus bilateral instrumented transforaminal lumbar
interbody fusion in degenerative lumbar diseases. Spine J.
12:209–215. 2012. View Article : Google Scholar
|
|
27
|
Harwood AR, Krajbich JI and Fornasier VL:
Radiotherapy of chondrosarcoma of bone. Cancer. 45:2769–2777. 1980.
View Article : Google Scholar : PubMed/NCBI
|