Introduction
For almost 20 years lung cancer has been the most
frequent malignancy worldwide, and it remains the most common cause
of cancer mortality (1,2). A large amount of evidence supports the
use of chemotherapy as a first-line therapy in advanced non-small
cell lung cancer (NSCLC) patients with a good performance status
(PS). This is founded on a landmark meta-analysis that demonstrated
the reduced risks of mortality and an increased one-year survival
rate following chemotherapy (3).
The current standard first-line therapy consists of platinum
combinations of two cytotoxic drugs with or without a
molecular-targeted agent (4,5).
The optimal duration of first-line chemotherapy for
patients with stage IV NSCLC has yet to be established. Socinski
et al (6) demonstrated that
continuing treatment with carboplatin (CBDCA) and paclitaxel beyond
four cycles produced no overall benefit in survival time, response
rates or quality of life for patients with advanced NSCLC. However,
the data are limited. According to the 2011 focused update of the
2009 American Society of Clinical Oncology (ASCO) clinical practice
guideline (7), first-line cytotoxic
chemotherapy should be discontinued when disease progression has
been detected or following four cycles in patients whose disease is
stable but is not responding to treatment. For the patients with
stable disease (SD), or for those who show a response following
four cycles of treatment, immediate treatment with an alternative,
single-agent chemotherapy, including pemetrexed, docetaxel or
erlotinib, may be administered. Following a fixed course of
treatment, a break from cytotoxic chemotherapy is also acceptable,
however, second-line chemotherapy is initiated upon disease
progression.
Despite the development of various first-line
therapies with a fixed course of treatment, the outcomes remain
poor. Two varying types of chemotherapy for the continuation of
treatment soon after stopping the platinum-based doublet regimens
have been extensively investigated. One is continuation maintenance
therapy, which involves continuing an agent that was part of the
initial induction treatment regimen (8–10),
while the other is switch maintenance therapy that involves
initiating another agent prior to disease progression (10–15).
The approximate median progression-free survival (PFS) time with
these therapeutic approaches ranged between 3 and 5 months
following maintenance therapy initiation, and between 6 and 7
months following induction therapy initiation, although patients
showing progressive disease (PD) with the first-induction therapy
were excluded (8–15).
One of the major variations between first-line
platinum doublet combinations and maintenance therapies is
feasibility. Continuation of a first-line platinum doublet regimen
may be difficult, even when the regimen is effective, due to
toxicity. Feasible first-line platinum doublet combinations could
be continued beyond standard cycle numbers and may exert favorable
effects if cumulative toxicities do not occur or can be managed
without deterioration of the PS. It is, however, extremely
difficult to perform a prospective study on continuous
multiple-cycle first-line treatments under the present
circumstances. However, the cycle number of first-line treatment
was not strictly determined until 2003 (16). The present study retrospectively
analyzed the efficacy and safety of continuous multiple-cycle
first-line treatment with CBDCA and docetaxel in advanced NSCLC
patients whose treatment had been initiated during the period
between July 1999 and February 2003.
Materials and methods
Patient selection
Between July 1999 and February 2003, NSCLC patients
who met the established criteria were treated with docetaxel plus
CBDCA at Saiseikai Central Hospital (Tokyo, Japan), according to
the selected treatment schedule. In total, a case series of 21
patients (17 males and 4 females) with inoperable stage IIIB and IV
NSCLC without prior chemotherapy were evaluated. The medical data
collected up to July 2004 was assessed. The primary outcome was
overall survival (OS) time, and the secondary outcomes included
PFS, response rate (RR) and adverse events. The retrospective
protocol was approved by the institutional review boards of the
Tokai University School of Medicine (Isehara, Japan) and the
Saiseikai Central Hospital (Tokyo, Japan).
The selection criteria for the patients were as
follows: Histologically or cytologically proven NSCLC; an Eastern
Cooperative Oncology Group PS of 0, 1 or 2; an age of ≥18 years;
measurable lesions as assessed by computed tomography (CT);
adequate bone marrow reserves, defined as a white blood cell (WBC)
count of ≥3,500/μl, a neutrophil count of ≥2,000/μl, a platelet
count of ≥100,000/μl and hemoglobin levels that were ≥10 g/dl; and
adequate liver function, defined as bilirubin levels of <2.0
mg/dl and/or aspartate transaminase (AST), alanine transaminase
(ALT) and γ-glutamyltransferase levels at more than three times the
upper limit of normal. Patients with impaired renal function were
included if the measured creatinine clearance was >40 ml/min.
Patients with ischemic heart diseases and diabetes mellitus were
included if their conditions were medically controlled, and those
who had central nervous system metastasis were also included. None
of the patients had undergone previous radiation therapy or major
surgery. Patients with malignant pleural and/or pericardial
effusions were also included. Patients with stage IIIB disease who
could be treated with curative radiotherapy were excluded.
Treatment schedule
Prior to starting chemotherapy, all the patients
underwent a physical examination, a complete blood count, blood and
urine chemistry, a chest X-ray, a chest CT scan, an abdominal echo
and/or CT scan, a head CT and/or MRI, a bone scan and
electrocardiography. The creatinine clearance was measured, and
complete blood cell counts, differential counts and routine blood
chemistry measurements were performed at least twice weekly during
the first cycle. On the day of the nadir following the initiation
of chemotherapy, the minimum WBC and neutrophil and platelet counts
were determined. The patients were hospitalized during all the
chemotherapy courses and evaluated by physical examination,
complete blood count, blood chemistry and a chest X-ray. The
responses were assessed every two cycles by a chest X-ray and/or a
CT scan, and metastasis was also evaluated.
All the patients received the following treatment
protocol: 60 mg/m2 docetaxel as a 3-h infusion in 500 ml
of 5% glucose or 0.9% saline, followed by 300 mg/m2
CBDCA as a 2-h infusion in 500 ml of 5% glucose or 0.9% saline
solution on day 1. Antiemetic treatment with 5-hydroxytryptamine-3
antagonists was provided prior to the administration of
chemotherapy. Steroids were not administered as premedication. The
treatment was repeated every three to four weeks, provided that the
patients had sufficiently recovered from any toxicities. The
patients were treated with the same regimen as many times as
possible unless there was evidence of PD, unacceptable toxicity or
they refused further treatment. Once PD occurred following the
initiation of the first-line treatment, second-line treatment began
if the patient wanted to continue. The patients with a brain
metastasis received either γ-knife radiosurgery or whole-brain
radiotherapy. The patients with symptomatic bone metastasis and
invasion were also treated with radiotherapy.
Recombinant human granulocyte colony-stimulating
factor (G-CSF) was not administered prophylactically in the first
cycle. G-CSF was administered at a dose of 1 μg/kg when the
neutrophil counts were <500/mm3, the febrile
neutrophil counts were <1,000/mm3 or the leukocyte
counts were <2,000/mm3. The patients who experienced
grade 4 neutropenia received prophylactic G-CSF administration and
the CBDCA dose was reduced by 25% in subsequent courses. The
docetaxel dose was reduced by another 25% to ameliorate the
neutropenia, as necessary. If the measured creatinine clearance was
between 40 and 50 ml/min, the CBDCA dose was reduced by 25%.
Response and toxicity evaluation
The responses were assessed using Response
Evaluation Criteria in Solid Tumors (version 1.0) (17). The confirmation of a complete
response (CR) or partial response (PR) was required at least 4
weeks subsequent to the initial documentation. SD was defined as
disease control (absence of progression) when it was maintained for
at least 6 weeks. Toxicity was graded according to the National
Cancer Institute’s Common Toxicity Criteria for Adverse Events,
version 3.0 (18).
Statistical analysis
PFS time was defined as the time that elapsed
between the first day of the first-line therapy and the date of PD
or mortality. The OS time was defined as the elapsed time between
the first day of the first-line therapy and the date of mortality.
The PFS and OS time differences between the groups were analyzed
using the Kaplan-Meier method and compared using the log-rank test.
Differences were considered to indicate a statistical significance
when P<0.05.
Results
The patient characteristics are listed in Table I. Unspecified NSCLC included
poorly-differentiated and non-specified carcinomas. All the
patients had a PS of 0–2. The measured creatinine clearances were
40–50, 51–60, 61–80, 81–90 and ≥91 ml/min in three (14.3%), four
(19.0%), four (19.0%), five (23.8%) and five (23.8%) patients,
respectively. The median area under the plasma concentration vs.
time curve (AUC) as calculated by employing Calvert’s formula, with
the measured creatinine clearance as the glomerular filtration
rate, was 4.4 mg/ml × min (range, 2.8–6.1 mg/ml × min). The
calculated AUC (mg/ml × min) values were 2.5–3.0, 3.1–4.0, 4.1–4.5,
4.6–5.0, 5.1–6.0 and ≥6.1 in two (9.5%), four (19.0%), five
(23.8%), five (23.8%), four (19.0%) and one (4.8%) patient,
respectively. The vast majority of patients presented with
adenocarcinoma and stage IV disease. All the patients were
assessable for toxicity and response.
 | Table IPatient characteristics. |
Table I
Patient characteristics.
| Characteristics | Value (%) |
|---|
| Total patients,
n | 21 (100) |
| Gender, n |
| Male | 17 (81.0) |
| Female | 4 (19.0) |
| Age, years |
| Median | 65 |
| Range | 46–77 |
| ECOG PS, n |
| 0 | 10 (47.6) |
| 1 | 4 (19.0) |
| 2 | 7 (33.3) |
| Creatinine clearance
in ml/min, n |
| 40–50 | 3 (14.3) |
| 51–60 | 4 (19.0) |
| 61–80 | 4 (19.0) |
| 81–90 | 5 (23.8) |
| ≥91 | 5 (23.8) |
| AUCa in mg/ml × min, n |
| 2.5–3.0 | 2 (9.5) |
| 3.1–4.0 | 4 (19.0) |
| 4.1–4.5 | 5 (23.8) |
| 4.6–5.0 | 5 (23.8) |
| 5.1–6.0 | 4 (19.0) |
| ≥6.1 | 1 (4.8) |
| Histology, n |
| Adenocarcinoma | 14 (66.7) |
| Squamous cell
carcinoma | 3 (14.3) |
| Large-cell
carcinoma | 2 (9.5) |
| Unspecified
NSCLC | 2 (9.5) |
| Clinical stage,
n |
| IIIB | 5 (23.8) |
| IV | 16 (76.2) |
| No. of organs with
metastases, n |
| 0 (stage IIIB) | 5 (23.8) |
| 1 | 3 (14.3) |
| 2 | 6 (28.6) |
| ≥3 | 7 (33.3) |
Fourteen patients achieved a PR (Table II). The overall RR was 66.7% [95%
confidence interval (CI), 43.0–85.4]. In total, five patients
(23.8%) had SD and two (9.5%) had PD. The patients with
adenocarcinoma had an RR of 64.3% (95% CI, 35.1–87.2), and those
with non-adenocarcinoma had an RR of 71.4% (95% CI, 29.0–96.3). The
median number of cycles per patient was four (range, 2–12 cycles),
and four patients received ≥10 cycles and achieved long survival
durations; 823 days (11 cycles), 625 days (10 cycles), 708 days (12
cycles) and 496 days (10 cycles).
 | Table IIResponses according to patient
characteristics. |
Table II
Responses according to patient
characteristics.
| | Response, n | | |
|---|
| |
| | |
|---|
| Characteristics | n | CR | PR | SD | PD | CR+PR, | % 95% CI |
|---|
| Histological
subtypes, Ca |
| Adeno | 14 | 0 | 9 | 4 | 1 | 64.3 | 35.1–87.2 |
| Non-adeno | 7 | 0 | 5 | 1 | 1 | 71.4 | 29.0–96.3 |
| Squamous cell | 3 | 0 | 3 | 0 | 0 | | |
| Large
cell/unspecified | 4 | 0 | 2 | 1 | 1 | | |
| Overall | 21 | 0 | 14 | 5 | 2 | 66.7 | 43.0–85.4 |
| No. of chemotherapy
cycles |
| 2 | 5 | 0 | 3 | 0 | 2 | | |
| 3 | 3 | 0 | 0 | 3 | 0 | | |
| 4 | 5 | 0 | 4 | 1 | 0 | | |
| 6 | 1 | 0 | 1 | 0 | 0 | | |
| 7 | 3 | 0 | 3 | 0 | 0 | | |
| ≥10 | 4 | 0 | 3 | 1 | 0 | | |
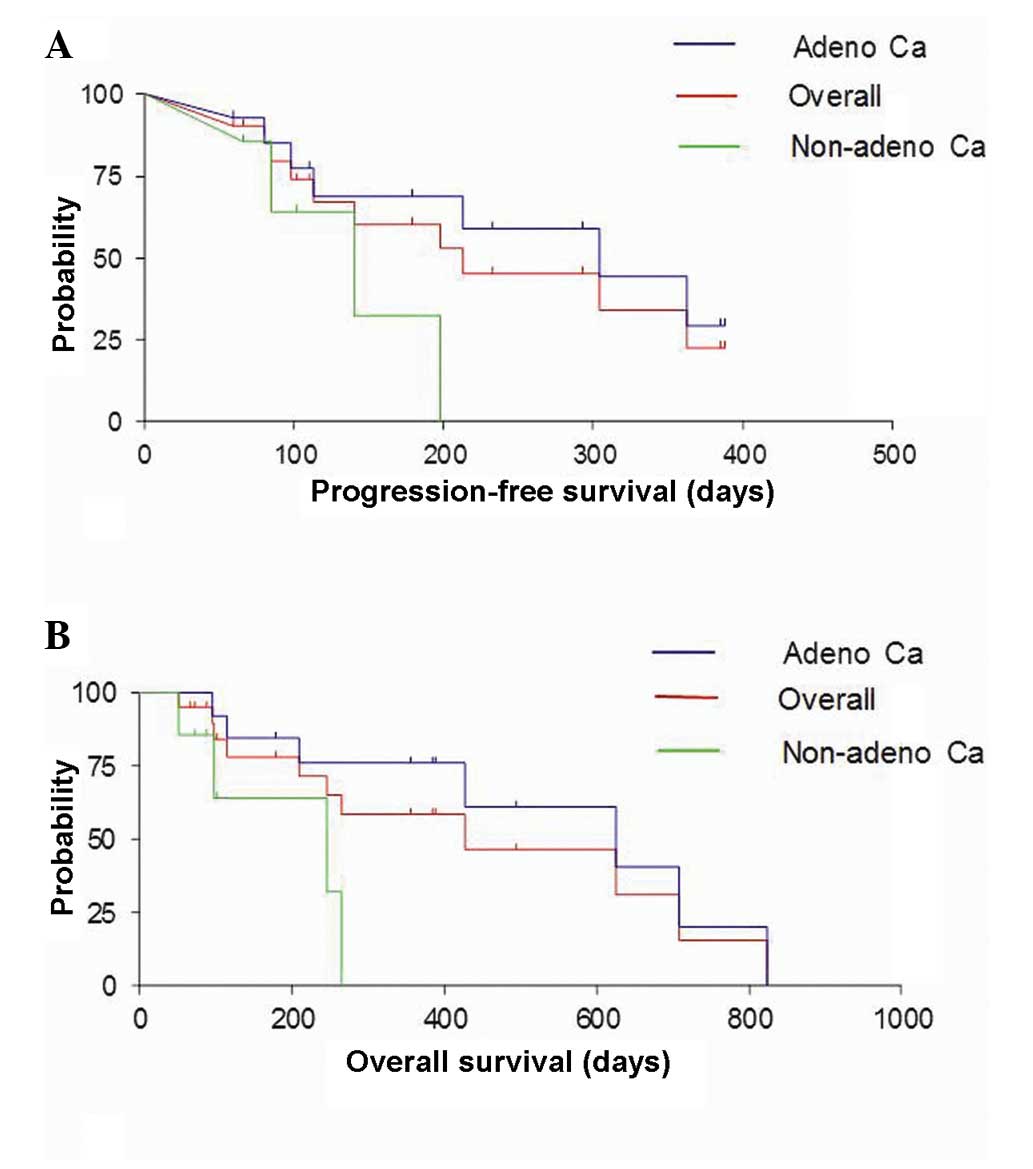
The median OS time (Fig.
1) was 400 days (range, 52–1,047 days). For the adenocarcinoma
patients the overall median survival time was 490 days (range,
95–1,047 days) and for the non-adenocarcinoma patients it was 192
days (range, 52–297 days). The log-rank test demonstrated a
significant survival difference between the adenocarcinoma and
non-adenocarcinoma patients (P=0.0012). The one-year survival rate
was 47.6% (95% CI, 25.7–70.2) and the two-year survival rate was
9.5% (95% CI, 1.2–30.4). Among the adenocarcinoma patients, the
one-year survival rate was 71.4% (95% CI, 41.9–91.6) and the
two-year survival rate was 14.3% (95% CI, 1.8–42.8). The one-year
survival rate was, however, 0% (95% CI, 0–41.0) among the
non-adenocarcinoma patients. The median PFS time (Fig. 1) for all the NSCLC patients was 176
days (range, 31–388 days), while the median PFS time was 210 days
(range, 42–388 days) for the adenocarcinoma patients and 108 days
(range, 31–198 days) for the non-adenocarcinoma patients.
The actual and relative dose intensities of CBDCA
are shown in Table III. The cycle
number and the total number of G-CSF injections for each patient
are also shown. Dose reduction was necessary in six patients.
Neutropenia was the only toxicity for which dose reduction was
required (Table IV). No patient
experienced a dose reduction for any reason other than grade 4
neutropenia. Grade 3/4 neutropenia was observed in 17 patients
(81.0%), grade 3/4 leukocytopenia in 14 (66.7%), grade 3
thrombocytopenia in three (14.3%) and grade 3 anemia in one patient
(4.8%). Neither grade 4 thrombocytopenia nor grade 4 anemia
occurred. Febrile neutropenia was observed in four patients. All
these patients were successfully managed with G-CSF and
broad-spectrum antibiotics. The patients with neutropenia recovered
with G-CSF administration, however, one patient with a perirectal
abscess deteriorated while neutropenic. This infection was
successfully treated with broad-spectrum antibiotics. No
thrombopenic episodes were complicated by hemorrhage. Alopecia was
almost universal (95.2%), and grade 1/2 nausea was observed in 10
patients (47.6%), whereas grade 1/2 vomiting was observed in three
(14.3%). Grade 1/2 diarrhea occurred in four patients (19.0%) and a
grade 1 allergic reaction in one (4.8%). Neuropathy, i.e.,
paresthesia with a loss of vibration sensation, occurred in only
one patient. None of the patients developed pneumonitis or
interstitial pneumonia. Grade 1/2 elevations of hepatic enzymes
were observed in four (AST), four (ALT) and two (alkaline
phosphatase) patients and these levels normalized without
medication. None of the patients showed nephrotoxicity and there
were no treatment-related mortalities.
 | Table IIIActual and relative CBDCA doses. |
Table III
Actual and relative CBDCA doses.
| CBDCA dose,
mg/body | Cycle no. | G-CSFa vials |
Dose
intensity of CBDCA, cycles |
|---|
|
|---|
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | >10 |
|---|
| 300 | 4 | 0 | 1 | 1 | 1 | 1 | | | | | | | |
| 360 | 7 | 0 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | | | | |
| 400 | 2 | 16 | 1 | 1 | | | | | | | | | |
| 400 | 3 | 11 | 1 | 1 | 1 | | | | | | | | |
| 400 | 4 | 12 | 1 | 1 | 1 | 1 | | | | | | | |
| 420 | 2 | 7 | 1 | 0.75 | | | | | | | | | |
| 420 | 3 | 0 | 1 | 1 | 1 | | | | | | | | |
| 450 | 4 | 12 | 1 | 1 | 1 | 1 | | | | | | | |
| 450 | 7 | 8 | 1 | 1 | 1 | 1 | 0.75 | 0.75 | 0.75 | | | | |
| 450 | 10 | 39 | 1 | 1 | 0.75 | 0.75 | 0.75 | 0.75 | 0.75 | 0.75 | 0.75 | 0.75 | |
| 450 | 7 | 12 | 1 | 1 | 1 | 0.75 | 0.75 | 0.75 | 0.75 | | | | |
| 450 | 10 | 21 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | |
| 450 | 11 | 32 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 |
| 450 | 12 | 53 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 0.75 | 0.75 |
| 460 | 6 | 34 | 1 | 0.75 | 0.75 | 0.75 | 0.75 | 0.75 | | | | | |
| 480 | 2 | 14 | 1 | 1 | | | | | | | | | |
| 500 | 2 | 9 | 1 | 1 | | | | | | | | | |
| 500 | 2 | 0 | 1 | 1 | | | | | | | | | |
| 500 | 4 | 6 | 1 | 1 | 1 | 1 | | | | | | | |
| 550 | 3 | 0 | 1 | 1 | 1 | | | | | | | | |
| 585 | 4 | 7 | 1 | 1 | 1 | 1 | | | | | | | |
 | Table IVToxicity in patients with National
Cancer Institute’s Common Toxicity Criteria for Adverse Events
(most severe, any course). |
Table IV
Toxicity in patients with National
Cancer Institute’s Common Toxicity Criteria for Adverse Events
(most severe, any course).
| Toxicity | Grade | Total, n (%) | ≥Grade 3, n
(%) |
|---|
|
|---|
| 1 | 2 | 3 | 4 |
|---|
| Neutropenia | 0 | 2 | 7 | 10 | 19 (90.5) | 17 (81.0) |
| Leukocytopenia | 2 | 2 | 11 | 3 | 18 (85.7) | 14 (66.7) |
| Febrile
neutropenia | 0 | 0 | 4 | 0 | 4 (19.0) | 4 (19.0) |
|
Thrombocytopenia | 4 | 1 | 3 | 0 | 8 (38.1) | 3 (14.3) |
| Infection | 0 | 0 | 1 | 0 | 1 (4.8) | 1 (4.8) |
| Anemia | 6 | 7 | 1 | 0 | 14 (66.7) | 1 (4.8) |
| Alopecia | 9 | 11 | 0 | 0 | 20 (95.2) | 0 (0.0) |
| Nausea | 8 | 2 | 0 | 0 | 10 (47.6) | 0 (0.0) |
| Vomiting | 2 | 1 | 0 | 0 | 3 (14.3) | 0 (0.0) |
| Diarrhea | 2 | 2 | 0 | 0 | 4 (19.0) | 0 (0.0) |
| Ileus | 0 | 0 | 0 | 0 | 0 (0.0) | 0 (0.0) |
| Allergic
reaction | 1 | 0 | 0 | 0 | 1 (4.8) | 0 (0.0) |
| Neuropathy | 1 | 0 | 0 | 0 | 1 (4.8) | 0 (0.0) |
| Pneumonitis | 0 | 0 | 0 | 0 | 0 (0.0) | 0 (0.0) |
| AST | 1 | 3 | 0 | 0 | 4 (19.0) | 0 (0.0) |
| ALT | 1 | 3 | 0 | 0 | 4 (19.0) | 0 (0.0) |
| Alkaline
phosphatase | 1 | 1 | 0 | 0 | 2 (9.5) | 0 (0.0) |
| Bilirubin | 0 | 0 | 0 | 0 | 0 (0.0) | 0 (0.0) |
| Liver failure | 0 | 0 | 0 | 0 | 0 (0.0) | 0 (0.0) |
Discussion
The present study retrospectively analyzed the
continuation of first-line treatment with docetaxel and CBDCA in
advanced NSCLC patients. The continuation of this first-line
treatment for disease control was possible, as the only cumulative
toxicity was neutropenia. The median number of cycles was, however,
four (range, 2–12 cycles), the same as the ASCO recommendations
(7). This continuous combination
therapy may have encouraging activity for the treatment of stage IV
adenocarcinoma, although not for stage IV non-adenocarcinoma,
including the poorly-differentiated type. In the treatment of the
adenocarcinoma patients of the present study, the RR of 64.3%, the
median PFS time of 210 days, the median survival time of 490 days
and the one-year survival rate of 71.4% were encouraging. Among the
adenocarcinoma patients who received ≥10 cycles, long-term survival
durations were achieved. Despite tumor persistence, neither tumor
regrowth nor progression occurred until the terminal stage in these
patients. The feasibility of the CBDCA-based combination with
docetaxel makes multiple administrations possible without serious
side-effects, including nausea/vomiting and nephrotoxicity, which
often develop in patients receiving CDDP-based combinations, or the
cumulative muscle pain and neurotoxicity observed in those who
receive paclitaxel.
Regarding the cycle number for first-line treatment,
a few studies have confirmed the non-inferiority, in terms of the
OS time, of three to four cycles compared with six cycles of
chemotherapy (19,20). However, a study by Soon et al
(21) reported that extending
chemotherapy beyond a standard number of cycles significantly
improved the PFS time in a meta-analysis of 13
randomized-controlled trials involving >3,000 patients. A cycle
number exceeding six could be administered in certain patients,
particularly those with adenocarcinoma, according to individual PS
and the side-effects of this protocol. The profiles of toxicities
occurring in the first cycle were almost the same as those in the
subsequent cycles. Toxicities, which had not been observed in the
first several cycles, were not cumulative.
Limitations of the present retrospective results,
obtained in clinical settings, include the small number of patients
and the lack of epidermal growth factor receptor mutation status
and echinoderm microtubule-associated protein-like 4 anaplastic
lymphoma kinase fusion gene status. However, determination of these
genetic features was not possible between 1999 and 2003. With this
treatment protocol, as performed at Saiseikai Central Hospital
(Tokyo, Japan) prior to 2003, the CBDCA dose was determined based
on the body surface area (BSA), rather than by the AUC, and the
CBDCA dose was 300 mg/m2, which is the dose approved by
the Japanese Ministry of Health, Labour and Welfare. Therefore,
Calvert’s formula was used to calculate the corresponding AUC,
employing the measured creatinine clearance. The mean calculated
AUC was 4.4 mg/ml × min, which was low compared with the TAX 326
study, a phase III study of docetaxel combined with a platinum
agent (22). In the TAX 326 study,
the AUC was 6 mg/ml × min for CBDCA, and the docetaxel dose was 75
mg/m2.
Neutropenia was a serious issue, and numerous G-CSF
administrations were necessary in patients receiving this
continuation therapy of docetaxel and CBDCA. No other toxicities
were serious. Despite the relatively low administered doses of
docetaxel and CBDCA, 17 patients (81.0%) experienced grade 3/4
neutropenia. These patients were successfully managed with G-CSF
and a dose reduction. No grade 3/4 toxicities, other than
myelosuppression, were observed. Alopecia was almost universal, but
not serious. Nausea, vomiting and diarrhea were moderate, but
manageable. There were no serious allergic reactions. Neuropathy,
which often occurs with paclitaxel administration, was rare and
mild. Due to these tolerable toxicity profiles and as hydration was
not necessary, patients with renal impairment (creatinine
clearance, 40–50 ml/min) were successfully treated with this
regimen.
Continuous first-line chemotherapy with docetaxel
(60 mg/m2) and CBDCA (300 mg/m2), as
determined by BSA rather than AUC, may be effective in advanced
NSCLC patients with adenocarcinoma. In the present study, the doses
of docetaxel and CBDCA were set relatively low, compared with the
majority of previously reported studies, and administered as many
times as possible. The rate of neutropenia was high however,
possibly making prophylactic G-CSF administration necessary.
Further investigations of the optimal cycle numbers are
warranted.
References
|
1
|
Ferlay J, Shin HR, Bray F, Forman D,
Mathers C and Parkin DM: GLOBOCAN 2012: Estimated cancer incidence,
mortality and prevalence worldwide. 2012, http://globocan.iarc.fr/Pages/fact_sheets_population.aspx.
Accessed February 20, 2014
|
|
2
|
Parkin DM, Bray F, Ferlay J and Pisani P:
Global cancer statistics, 2002. CA Cancer J Clin. 55:74–108. 2005.
View Article : Google Scholar
|
|
3
|
No authors listed. Chemotherapy in
non-small cell lung cancer: a meta-analysis using updated data on
individual patients from 52 randomised clinical trials. Non-small
Cell Lung Cancer Collaborative Group. BMJ. 311:899–909. 1995.
View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Azzoli CG, Baker S Jr, Temin S, Pao W,
Aliff T, Brahmer J, Johnson DH, Laskin JL, Masters G, Milton D,
Nordquist L, Pfister DG, Piantadosi S, Schiller JH, Smith R, Smith
TJ, Strawn JR, Trent D and Giaccone G; American Society of Clinical
Oncology. American Society of Clinical Oncology clinical practice
guideline update on chemotherapy for stage IV non-small-cell lung
cancer. J Clin Oncol. 27:6251–6266. 2009. View Article : Google Scholar
|
|
5
|
National Comprehensive Cancer Network.
Clinical practice guidelines in oncology: non-small cell lung
cancer, version 2. 2012, http://www.nccn.org/professionals/physician_gls/pdf/nscl.pdf.
Accessed August 10, 2013
|
|
6
|
Socinski MA, Schell MJ, Peterman A, Bakri
K, Yates S, Gitten R, Unger P, Lee J, Lee JH, Tynan M, Moore M and
Kies MS: Phase III trial comparing a defined duration of therapy
versus continuous therapy followed by second-line therapy in
advanced-stage IIIB/IV non-small-cell lung cancer. J Clin Oncol.
20:1335–1343. 2002. View Article : Google Scholar
|
|
7
|
Azzoli CG, Temin S, Aliff T, Baker S Jr,
Brahmer J, Johnson DH, Laskin JL, Masters G, Milton D, Nordquist L,
Pao W, Pfister DG, Piantadosi S, Schiller JH, Smith R, Smith TJ,
Strawn JR, Trent D and Giaccone G; American Society of Clinical
Oncology. 2011 focused update of 2009 American Society of Clinical
Oncology clinical practice guideline update on chemotherapy for
stage IV non-small-cell lung cancer. J Clin Oncol. 29:3825–3831.
2011. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Brodowicz T, Krzakowski M, Zwitter M,
Tzekova V, Ramlau R, Ghilezan N, Ciuleanu T, Cucevic B, Gyurkovits
K, Ulsperger E, Jassem J, Grgic M, Saip P, Szilasi M, Wiltschke C,
Wagnerova M, Oskina N, Soldatenkova V, Zielinski C and Wenczl M;
Central European Cooperative Oncology Group CECOG. Cisplatin and
gemcitabine first-line chemotherapy followed by maintenance
gemcitabine or best supportive care in advanced non-small cell lung
cancer: a phase III trial. Lung Cancer. 52:155–163. 2006.
View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Paz-Ares L, de Marinis F, Dediu M, Thomas
M, Pujol JL, Bidoli P, Molinier O, Sahoo TP, Laack E, Reck M,
Corral J, Melemed S, John W, Chouaki N, Zimmermann AH,
Visseren-Grul C and Gridelli C: Maintenance therapy with pemetrexed
plus best supportive care versus placebo plus best supportive care
after induction therapy with pemetrexed plus cisplatin for advanced
non-squamous non-small-cell lung cancer (PARAMOUNT): a
double-blind, phase 3, randomized controlled trial. Lancet Oncol.
13:247–255. 2012.
|
|
10
|
Pérol M, Chouaid C, Pérol D, Barlési F,
Gervais R, Westeel V, Crequit J, Léna H, Vergnenègre A, Zalcman G,
Monnet I, Le Caer H, Fournel P, Falchero L, Poudenx M, Vaylet F,
Ségura-Ferlay C, Devouassoux-Shisheboran M, Taron M and Milleron B:
Randomized, phase III study of gemcitabine or erlotinib maintenance
therapy versus observation, with predefined second-line treatment,
after cisplatin-gemcitabine induction chemotherapy in advanced
non-small-cell lung cancer. J Clin Oncol. 30:3516–3524. 2012.
|
|
11
|
Fidias PM, Dakhil SR, Lyss AP, Loesch DM,
Waterhouse DM, Bromund JL, Chen R, Hristova-Kazmierski M, Treat J,
Obasaju CK, Marciniak M, Gill J and Schiller JH: Phase III study of
immediate compared with delayed docetaxel after front-line therapy
with gemcitabine plus carboplatin in advanced non-small-cell lung
cancer. J Clin Oncol. 27:591–598. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Ciuleanu T, Brodowicz T, Zielinski C, Kim
JH, Krzakowski M, Laack E, Wu YL, Bover I, Begbie S, Tzekova V,
Cucevic B, Pereira JR, Yang SH, Madhavan J, Sugarman KP, Peterson
P, John WJ, Krejcy K and Belani CP: Maintenance pemetrexed plus
best supportive care versus placebo plus best supportive care for
non-small-cell lung cancer: a randomized, double-blind, phase 3
study. Lancet. 374:1432–1440. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Cappuzzo F, Ciuleanu T, Stelmakh L,
Cicenas S, Szczésna A, Juhász E, Esteban E, Molinier O, Brugger W,
Melezínek I, Klingelschmitt G, Klughammer B and Giaccone G; SATURN
investigators. Erlotinib as maintenance treatment in advanced
non-small-cell lung cancer: a multicentre, randomised,
placebo-controlled phase 3 study. Lancet Oncol. 11:521–529. 2010.
View Article : Google Scholar
|
|
14
|
Takeda K, Hida T, Sato T, Ando M, Seto T,
Satouchi M, Ichinose Y, Katakami N, Yamamoto N, Kudoh S, Sasaki J,
Matsui K, Takayama K, Kashii T, Iwamoto Y, Sawa T, Okamoto I,
Kurata T, Nakagawa K and Fukuoka M: Randomized phase III trial of
platinum-doublet chemotherapy followed by gefitinib compared with
continued platinum-doublet chemotherapy in Japanese patients with
advanced non-small-cell lung cancer: results of a west Japan
thoracic oncology group trial (WJTOG0203). J Clin Oncol.
28:753–760. 2010.
|
|
15
|
Zhang L, Ma S, Song X, Han B, Cheng Y,
Huang C, Yang S, Liu X, Liu Y, Lu S, Wang J, Zhang S, Zhou C, Zhang
X, Hayashi N and Wang M; INFORM investigators. Gefitinib versus
placebo as maintenance therapy in patients with locally advanced or
metastatic non-small-cell lung cancer (INFORM; C-TONG 0804): a
multicentre, double-blind randomized phase 3 trial. Lancet Oncol.
13:466–475. 2012. View Article : Google Scholar
|
|
16
|
Pfister DG, Johnson DH, Azzoli CG, Sause
W, Smith TJ, Baker S Jr, Olak J, Stover D, Strawn JR, Turrisi AT
and Somerfield MR; American Society of Clinical Oncology. American
Society of Clinical Oncology treatment of unresectable
non-small-cell lung cancer guideline: update 2003. J Clin Oncol.
22:330–353. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Therasse P, Arbuck SG, Eisenhauer EA,
Wanders J, Kaplan RS, Rubinstein L, Verweij J, Van Glabbeke M, van
Oosterom AT, Christian MC and Gwyther SG: New guidelines to
evaluate the response to treatment in solid tumors. European
Organization for Research and Treatment of Cancer, National Cancer
Institute of the United States, National Cancer Institute of
Canada. J Natl Cancer Inst. 92:205–216. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Cancer Therapy Evaluation Program. Common
Terminology Criteria for Adverse Events (CTCAE) Version 30. DCTD,
NCI, NIH, DHHS; 2006, http://ctep.cancer.gov/protocolDevelopment/electronic_applications/docs/ctcaev3.pdf.
Accessed August 10, 2013
|
|
19
|
von Plessen C, Bergman B, Andresen O,
Bremnes RM, Sundstrom S, Gilleryd M, Stephens R, Vilsvik J, Aasebo
U and Sorenson S: Palliative chemotherapy beyond three courses
conveys no survival or consistent quality-of-life benefits in
advanced non-small-cell lung cancer. Br J Cancer. 95:966–973.
2006.PubMed/NCBI
|
|
20
|
Park JO, Kim SW, Ahn JS, Suh C, Lee JS,
Jang JS, Cho EK, Yang SH, Choi JH, Heo DS, Park SY, Shin SW, Ahn
MJ, Lee JS, Yun YH, Lee JW and Park K: Phase III trial of two
versus four additional cycles in patients who are nonprogressive
after two cycles of platinum-based chemotherapy in non small-cell
lung cancer. J Clin Oncol. 25:5233–5239. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Soon YY, Stockler MR, Askie LM and Boyer
MJ: Duration of chemotherapy for advanced non-small-cell lung
cancer: a systematic review and meta-analysis of randomized trials.
J Clin Oncol. 27:3277–3283. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Fossella F, Pereira JR, von Pawel J,
Pluzanska A, Gorbounova V, Kaukel E, Mattson KV, Ramlau R, Szczesna
A, Fidias P, Millward M and Belani CP: Randomized, multinational,
phase III study of docetaxel plus platinum combinations versus
vinorelbine plus cisplatin for advanced non-small-cell lung cancer:
the TAX 326 study group. J Clin Oncol. 21:3016–3024. 2003.
View Article : Google Scholar : PubMed/NCBI
|