Introduction
Epithelial-myoepithelial carcinoma (EMC) is a rare
neoplasm, first described in 1972 by Donath et al (1). EMC accounts for ~1% of epithelial
salivary gland tumors, with the majority of cases of EMC arising in
the parotid gland (2).
Histologically, EMC is characterized by two types of cells arranged
in well-defined tubules; epithelial cells in the inner layer and
myoepithelial cells in the outer layer. EMC is always found
clinically, and is occasionally identified by the patient or doctor
as it commonly presents as a painless and slow growing neoplasm. In
addition, the majority of patients have no complaints at the early
stage. EMC is recognized to be a low-grade malignant tumor with a
low metastasis rate and the primary treatment of EMC is to surgical
excision (3). However, EMC arising
in the hypopharynx has not previously been reported. The current
study presents the first case in a 48-year-old male who exhibited
no other symptoms with the exception of dysphagia for six months.
The 2-cm-diameter mass was predominantly located in the left
posterior wall of the hypopharynx, and the mass was histologically
and immunohistochemically confirmed as EMC. The current study
describes the treatment and outcomes of EMC in the hypopharynx and
may provide useful information for future studies. Patient provided
written informed consent.
Case report
Case summary
A 48-year-old male was referred to the Digestive
System Department due to a 6-month history of dysphagia in
February, 2011. A video-fiber gastroscopy revealed a 2-cm-diameter
mass in the left posterior wall of the hypopharynx. False vocal
folds, vocal folds and piriform fossa were normal, as were the
other portions of the upper aero-digestive tract. A biopsy showed a
minor salivary glands tumor. Computed tomography (CT) of the neck
revealed a contrast-enhanced mass in the hypopharynx. The patient
underwent partial hypopharyngectomy with a left-side neck
dissection under general anesthesia. The partial neck dissection
revealed 20 lymph nodes that were negative for metastases. The
present patient has shown no sign of recurrence or metastasis
during the 27 months of follow-up.
Pathological findings
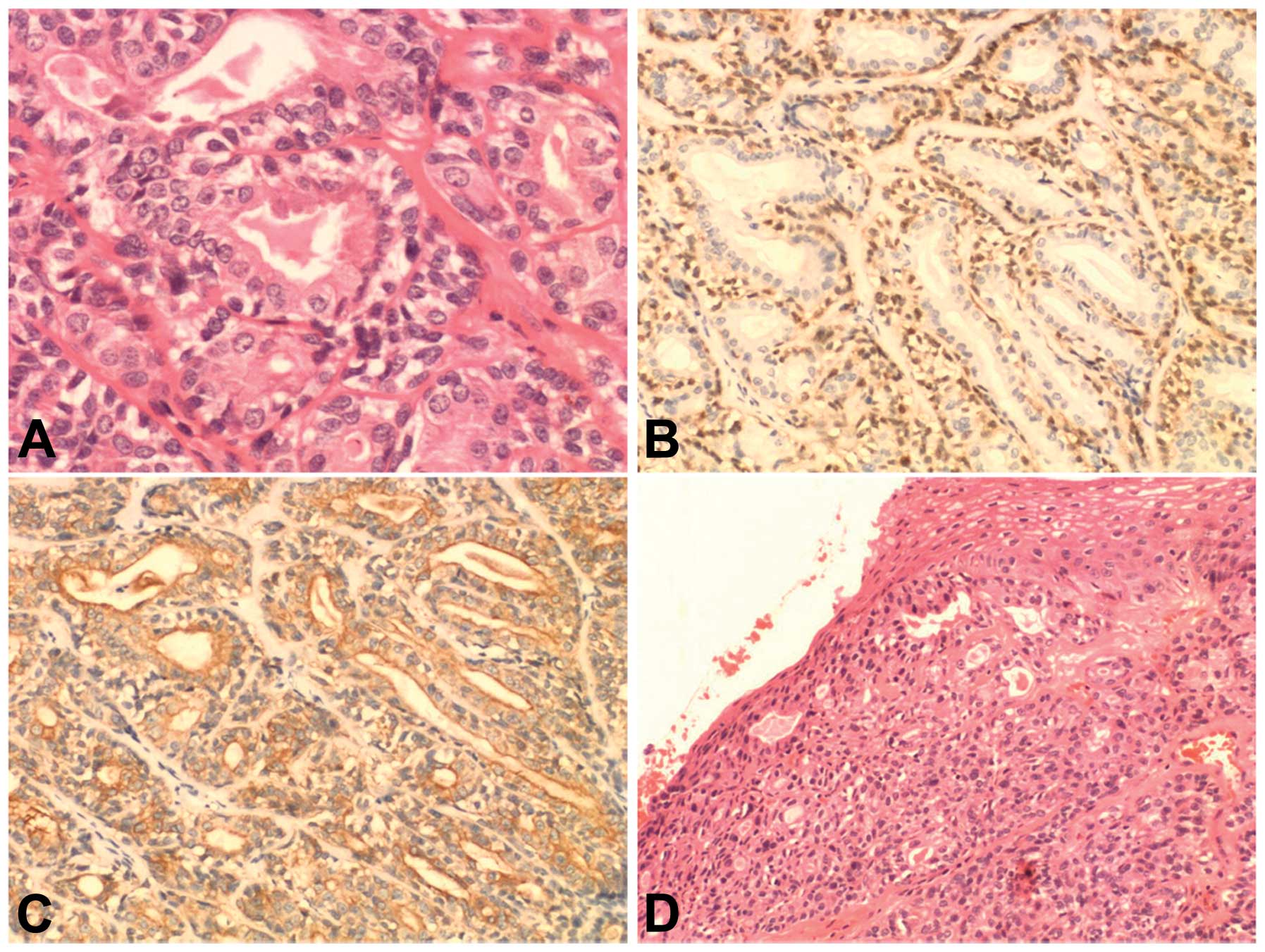
Microscopically, the tumor cells were arranged in
duct-like structures with an inner layer of ductal cells and an
outer layer of clear cells (Fig.
1A). Immunohistochemically, the outer layer of clear cells
stained positive for calponin, p63 protein, glial fibrillary acidic
protein, S-100 protein and smooth muscle actin, which is consistent
with a myoepithelial phenotype (Fig.
1B). The inner layer stained positive for cytokeratin and
cytokeratin-7, which is consistent with an epithelial phenotype
(Fig. 1C). The tumor cells were
partially involved in the overlying pharyngeal epithelium, and
induced necrosis and exfoliation (Fig.
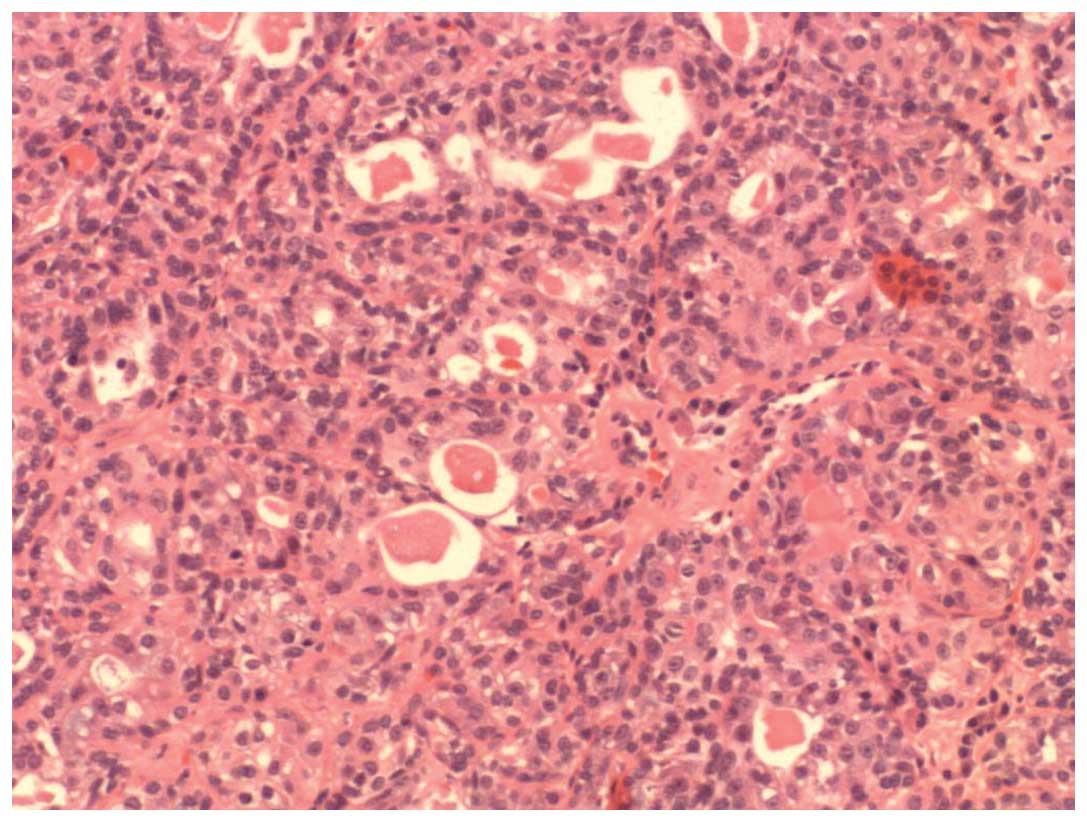
1D). These features were consistent with EMC. In the minor
region, the tumor was composed of variable sized ducts and nests,
and the tumor cells were monomorphic in appearance, round to oval
and had a moderate amount of eosinophilic to clear cytoplasm
(Fig. 2).
Discussion
EMC is a rare neoplasm and the majority of cases
occur in the parotid gland, while a few arise in the nasal cavity,
paranasal sinus, nasopharynx, subglottic region, trachea, bronchus,
lung, lacrimal gland, submandibular gland, tongue base, palate and
liver (3). The majority of patients
are females in their fifth to eighth decades (4). To the best of our knowledge, this is
the first case of EMC occurring in the hypopharynx. The patient was
male and had a 6-month history of dysphagia, without any pain or
hoarseness.
The diagnosis of EMC is based on conventional light
microscopy and immunohistochemical testing. Histologically, the EMC
tumor is determined by well-characterized tubules of two cell
types. These are an outer mantle of larger myoepithelial cells with
a clear cytoplasm that stains positive for calponin, p63 protein,
glial fibrillary acidic protein, S-100 protein and smooth muscle
actin, that are surrounding an inner lining of eosinophilic
cuboidal epithelial cells stained positive for cytokeratin,
cytokeratin-7 and epithelial membrane antigen (3,5). By
contrast, in the present case, certain areas of the specimens only
consisted of variable sized ducts and nests, the tumor cells were
monomorphic in appearance, round to oval and had a moderate amount
of eosinophilic to clear cytoplasm, without the characteristic
bilayered tubules, but similar to the characteristics of
polymorphous low-grade adenocarcinoma. Initially it was believed
that the diagnosis was a hybrid carcinoma composed of EMC and
polymorphous low-grade adenocarcinoma. Therefore, this may cause
diagnostic difficulty and confusion with other neoplasms if there
were no characteristic bilayered tubules in the sampled
specimens.
EMC is believed to be a low-grade malignancy tumor
(6), and the first choice of
treatment for EMC in the salivary glands is wide-surgical excision
with a clear margin (7). Fonseca
and Soares (3) reported that the
recurrence rate of EMC is between 35 and 40%, and that the
metastatic rate is between 8.1 and 25%. In the present study, the
patient underwent partial hypopharyngectomy with a left-side neck
dissection under general anesthesia. The partial neck dissection
revealed 20 lymph nodes that were negative for metastases, and the
patient has shown no sign of recurrence or metastasis during the 27
months of follow-up, however, close and prolonged follow-up is
required to evalate the prognosis of EMC in the hypopharynx. A
study by Cho et al (8)
showed that the mean interval between diagnosis and recurrence was
5 years (range, 1–19 years) and that the mean interval between
diagnosis and metastasis was 15 years (range, 4–20 years).
In conclusion, the present study reports the first
case of an EMC in the hypopharynx. The patient has shown no sign of
recurrence or metastasis during the 27 months since the partial
hypopharyngectomy. The results of the current study may aid in the
prognosis of EMC.
References
|
1
|
Donath K, Seifert G and Schmiz R:
Diagnosis and ultrastructure of the tubular carcinoma of salivary
gland ducts. Epithelial-myoepithelial carcinoma of the intercalated
ducts. Virchows Arch A Pathol Pathol Anat. 356:16–31. 1972.(In
German).
|
|
2
|
Ellis GL and Auclair PL: Malignant
epithelial tumors. Atlas of Tumor Pathology. 3rd edition. AFIP;
Washington: pp. 337–343. 1996
|
|
3
|
Fonseca I and Soares J:
Epithelial-myoepithelial carcinoma. World Health Organization
Classification of Head and Neck Tumours. Barnes L, Eveson JW,
Reichart P, et al: 1st edition. IARC Press; Lyon: pp. 225–226.
2005
|
|
4
|
Seethala RR, Barnes EL and Hunt JL:
Epithelial-myoepithelial carcinoma: a review of the
clinicopathologic spectrum and immunophenotypic characteristics in
61 tumors of the salivary glands and upper aerodigestive tract. Am
J Surg Pathol. 31:44–57. 2007. View Article : Google Scholar
|
|
5
|
Cheuk W and Chan JK: Advances in salivary
gland pathology. Histopathology. 51:1–20. 2007. View Article : Google Scholar
|
|
6
|
Senis-Segarra L, Sahuquillo-Arce E, Davo
R, et al: Salivary gland epithelial-myoepithelial carcinoma:
behaviour, diagnosis and treatment. Med Oral. 7:391–395. 2002.(In
Spanish).
|
|
7
|
Witterick IJ, Noyek AM, Chapnik JS, et al:
Observation of the natural history of a parotid
epithelialmyoepithelial carcinoma of intercalated ducts. J
Otolaryngol. 22:176–179. 1993.PubMed/NCBI
|
|
8
|
Cho KJ, el-Naggar AK, Ordonez NG, et al:
Epithelial-myoepithelial carcinoma of the salivary glands. A
clinicopathologic, DNA flow cytometric, and immunohistochemical
study of Ki-67 and HER-2/neu oncogene. Am J Clin Pathol.
103:432–437. 1995.
|