Introduction
Breast cancer is the second most common type of
cancer worldwide and undoubtedly the most common type of malignant
disease in females. Despite the application of the American Joint
Committee on Cancer tumor-node-metastasis system for staging and
prognosis, ≤30% of node-negative patients ultimately develop
recurrent disease (1). This may
occur as a result of occult metastatic cells that are undetectable
by current methods, which have spread via a lymphatic or
hematogenous route. Therefore, it is of great clinical value to
detect disseminated tumor cells using effective markers to
supplement the staging method, prediction of metastasis and
prognosis in breast cancer.
As breast cancer is highly heterogeneous and tumor
cells continue to evolve genetically in response to host pressures,
no single marker has been identified to be consistently and
specifically expressed by all of the breast cancer cells. The
positive detection rate of circulating cancer cells in breast
cancer patients was only 43.9% when the single marker gene,
cytokeratin 19, was employed (2).
Therefore, a combination of multiple markers may be required to
improve the sensitivity and specificity for the detection of
circulating cancer cells. In addition, the number of circulating
cancer cells is so small that they cannot be detected by
conventional diagnostic methods, including imaging studies and
assays for serum marker detection. However, it has been reported
that the nest reverse transcription (RT)-polymerase chain reaction
(PCR) is extremely sensitive and capable of detecting one breast
cancer cell in 107 cells, which is equivalent to four
cells per 10 ml blood (3). However,
such a technically demanding and time-consuming method is less
suitable for clinical application.
In the present study, a simple and rapid nested PCR
technique for the detection of circulating cancer cells in breast
cancer patients is described; the method was based on designing two
pairs of primers with marked differences in their annealing
temperatures. In addition, a panel of markers was identified for
the detection of circulating cancer cells in breast cancer patients
by in silico analysis of the National Cancer
Institute-Cancer Genome Anatomy Project database (http://cgap.nci.hih.gov/) (4). This rapid method was used to
investigate clinical specimens obtained from breast cancer patients
using the novel panel of marker genes. The panel of three marker
genes was demonstrated to result in a significant improvement in
the positive detection rate, which indicated that the positive
expression of these markers correlates with the metastasis in, and
prognosis of, breast cancer patients.
Patients and methods
Patients and samples
The present study was conducted using a total of 142
blood samples obtained from breast cancer patients, who were
histopathologically and clinically diagnosed at the Affiliated
Hospital of Chengde Medical College Cancer Center (Chengde, China)
between November 2009 and December 2013. All patients provided
written informed consent and the study was approved by the Ethics
Review Committee of Chengde Medical College (Chengde, China). The
patient age ranged from 21 to 82 years, with a mean age of 52
years. A total of 60 healthy female volunteers were also enrolled
(median age, 49 years; range, 22–76 years). None of the patients
received anti-hormonal treatment, chemotherapy, or radiotherapy
prior to surgery. All data, including age, pathological type, tumor
size, distant metastasis, clinical stage, estrogen receptor (ER),
progesterone receptor (PgR), human epidermal growth factor receptor
2 and recurrence, were obtained from the clinical and pathological
records.
Peripheral blood samples were obtained from
superficial veins on the opposite side to the breast cancer by
standard transcutaneous needle venipuncture and placed into a
citrate sodium-containing tube. Two tubes were used to collect the
blood, with 1 ml in the first tube and 5 ml in the second tube. The
blood in the first tube was discarded as it may have been
contaminated with epithelial cells picked up by the needle as it
pierced the skin. However, the blood in the second tube was loaded
on to a Ficoll-Hypaque layer (Gibco BRL, Carlsbad, CA, USA), and
following density gradient centrifugation (Centrifuge HK-2C,
Shenzhen Homk Telecommunication Technology Co., Ltd., Shenzhen,
China) at 2,000 × g for 30 min at room temperature, the peripheral
blood mononuclear cells (PBMCs) were collected. The PBMCs were
washed twice using a sterile phosphate buffer solution. The cell
pellets were subsequently snap frozen and stored at −80°C until RNA
extraction.
Identification of candidate marker
genes
A large database of information regarding expressed
sequence tags has been generated using cancer cell lines and is
maintained on the cDNA Digital Gene Expression Displayer (developed
by the National Cancer Institute-Cancer Genome Anatomy Project).
This was used in the present study to identify the genes that were
differentially expressed between breast cancer cells and
leukocytes. The Digital Gene Expression Displayer program
identified differentially expressed genes among 30,460 sequences in
four breast cancer cDNA libraries and 21,036 sequences in five
leukocyte cDNA libraries with the P filter set at 0.01. The
differentially expressed genes were ranked by sequence odds ratio
and the genes with the highest sequence odds ratios were selected
as candidate marker genes for the RT-PCR assay.
RNA preparation and cDNA synthesis
Total RNA was extracted using TRIzol reagent
(Invitrogen Life Technologies, Carlsbad, CA, USA) according to the
manufacturer’s instructions, treated with DNase I (Promega
Corporation, Madison, WI, USA) and quantitated using ultraviolet
spectrophotometry (UV2000; LabTech, Beijing, China). Subsequently,
cDNA was synthesized from 2 μg total RNA using advantage reverse
transcriptase (Clontech Laboratories, Inc., Mountain View, CA,
USA). The integrity of the patients’ RNA samples and the fidelity
of the cDNA synthesis were verified by a test amplification of
GAPDH in a standard PCR reaction.
Novel rapid nested RT-PCR assay
To detect the small number of cancer cells in the
blood circulation, a novel, highly sensitive and rapid nested PCR
technique was developed. Two pairs of primers with marked
differences in their annealing temperatures (72 and 60°C for the
outer and inner primers, respectively) were designed; the primer
sequences are listed in Table I.
The rapid nested PCR was performed using 2.5 μl of 10-fold diluted
cDNA with a PCR mixture containing 0.2 μmol/l outer primers
(100-fold dilution), 20 μmol/l inner primers, 0.2 mM
deoxynucleotide triphosphate, 50 mM Tris-HCl, 10 mM KCl, 5 mM
(NH4)2SO4, 2 mM MgCl2
and 0.75 units of Taq polymerase, in a total volume of 25
μl. The PCR conditions used were as follows: 95°C for 5 min; 30
cycles at 95°C for 20 sec and 72°C for 1 min; 20 cycles at 95°C for
10 sec, 60°C for 20 sec and 72°C for 10 sec; and a final extension
at 72°C for 7 min.
 | Table IPrimer sequences used in the
polymerase chain reaction for detecting the three marker genes. |
Table I
Primer sequences used in the
polymerase chain reaction for detecting the three marker genes.
| Gene | Primer sequence | Annealing
temperature, °C | Product, bp |
|---|
| FAM83A | | | 318 |
| Outer | | 72 | |
| Forward |
5′-CGCCACTGTGTACTTCCAGACCGTCAAGC-3′ | | |
| Reverse |
5′-CCTCGGCGGTTCTGCTCATGCTCCACTC-3′ | | |
| Inner | | 60 | |
| Forward |
5′-GTGGGGTGTTCGTTTGTG-3′ | | |
| Reverse |
5′-GCTTGGAGGAGGCGTAG-3′ | | |
| NPY1R | | | 372 |
| Outer | | 72 | |
| Forward |
5′-GCGTTCCAAAATGTAACACTTGATGCGTACA-3′ | | |
| Reverse |
5′-CATCTGTGTGCATCGTGGACATGGCTATTGT-3′ | | |
| Inner | | 60 | |
| Forward |
5′-CACTCTTCTCTTGGTGCTG-3′ | | |
| Reverse |
5′-GTTTTTGTTCAGGAACCCA-3′ | | |
| KRT19 | | | 393 |
| Outer | | 72 | |
| Forward |
5′-AAGCTAACCATGCAGAACCTCAACGACCGC-3′ | | |
| Reverse |
5′-TTTTATTGGCAGGTCAGGAGAAGAGCC-3′ | | |
| Inner | | 60 | |
| Forward |
5′-CAGCCACTACTACACGACC-3′ | | |
| Reverse |
5′-ACCTCATATTGGCTTCGCA-3′ | | |
| GAPDH | | 60 | 452 |
| Forward |
5′-ACCACAGTCCATGCCATC-3′ | | |
| Reverse |
5′-TCCACCACCCTGTTGCTGTA-3′ | | |
To evaluate the novel rapid nested PCR technique,
the traditional nested PCR was also performed using 1 μl of 20-fold
diluted cDNA with a PCR mixture containing 20 μmol/l outer primers,
0.2 mM deoxynucleotide triphosphate, 50 mM Tris-HCl, 10 mM KCl, 5
mM (NH4)2SO4, 2 mM
MgCl2 and 0.75 units of Taq polymerase in a total
volume of 25 μl. The PCR conditions used were as follows: 30 Cycles
at 95°C for 20 sec and 72°C for 50 sec; and a final extension at
72°C for 7 min. Next, 2 μl of the first PCR product (1:100) was
used as a template for the following round of PCR and the
conditions were as follows: 30 Cycles at 95°C for 20 sec, 60°C for
20 sec and 72°C for 20 sec; and a final extension at 72°C for 7
min.
The positive and negative controls were included in
each run and all precautions to prevent cross-contamination were
observed. Visualization of the target bands was performed using a
1.0% agarose gel with ethidium bromide staining to determine the
expression of the mRNA transcripts.
Follow-up
A follow-up study of the 142 breast cancer patients
was conducted by telephone interview, between November 2009 and
December 2013 with additional verification of their clinical
records. Chest X-rays and mammographs were examined biannually, and
liver ultrasounds and bone scans were examined annually.
Statistical analysis
Statistical analyses were conducted using SPSS 17.0
statistical package (SPSS, Inc., Chicago, IL, USA) and the
χ2 test was performed to determine the correlation
between the marker expression status and clinicopathological
features. The survival distributions were investigated using
Kaplan-Meier methods and the log-rank test was used to assess the
statistical significance of differences in overall survival between
the different groups. P<0.05 was considered to indicate a
statistically significant difference.
Results
Marker genes for detecting circulating
breast cancer cells
The in silico Digital Gene Expression
Displayer program search of the National Cancer Institute-Cancer
Genome Anatomy Project database yielded 23 overexpressed genes with
a sequence odds ratio of >16 between the breast cancer and
leukocyte cDNA libraries. The nested PCR was used to further verify
the candidate genes in the peripheral blood samples of the 43
breast cancer patients and 20 healthy control subjects, whereby
three marker genes, including FAM83A (NM_032899.4), NPY1R
(NM_000909.5) and KRT19 (NM_002276), were identified as the novel
panel of markers. Of the 43 breast cancer patients, 14 patients
exhibited NPY1R expression and 16 patients expressed FAM83A,
however, these two marker genes were undetectable in the peripheral
blood of the 20 healthy control subjects. Furthermore, the marker
gene, KRT19, showed positive expression in 21 breast cancer patient
samples, however, only one patient expressed the gene in the
healthy control group.
Evaluation of the rapid nested PCR
assay
Using the novel rapid and traditional nested PCR
techniques to detect the circulating cancer cells of 43 breast
cancer patients, the same 16 samples exhibited FAM83A expression in
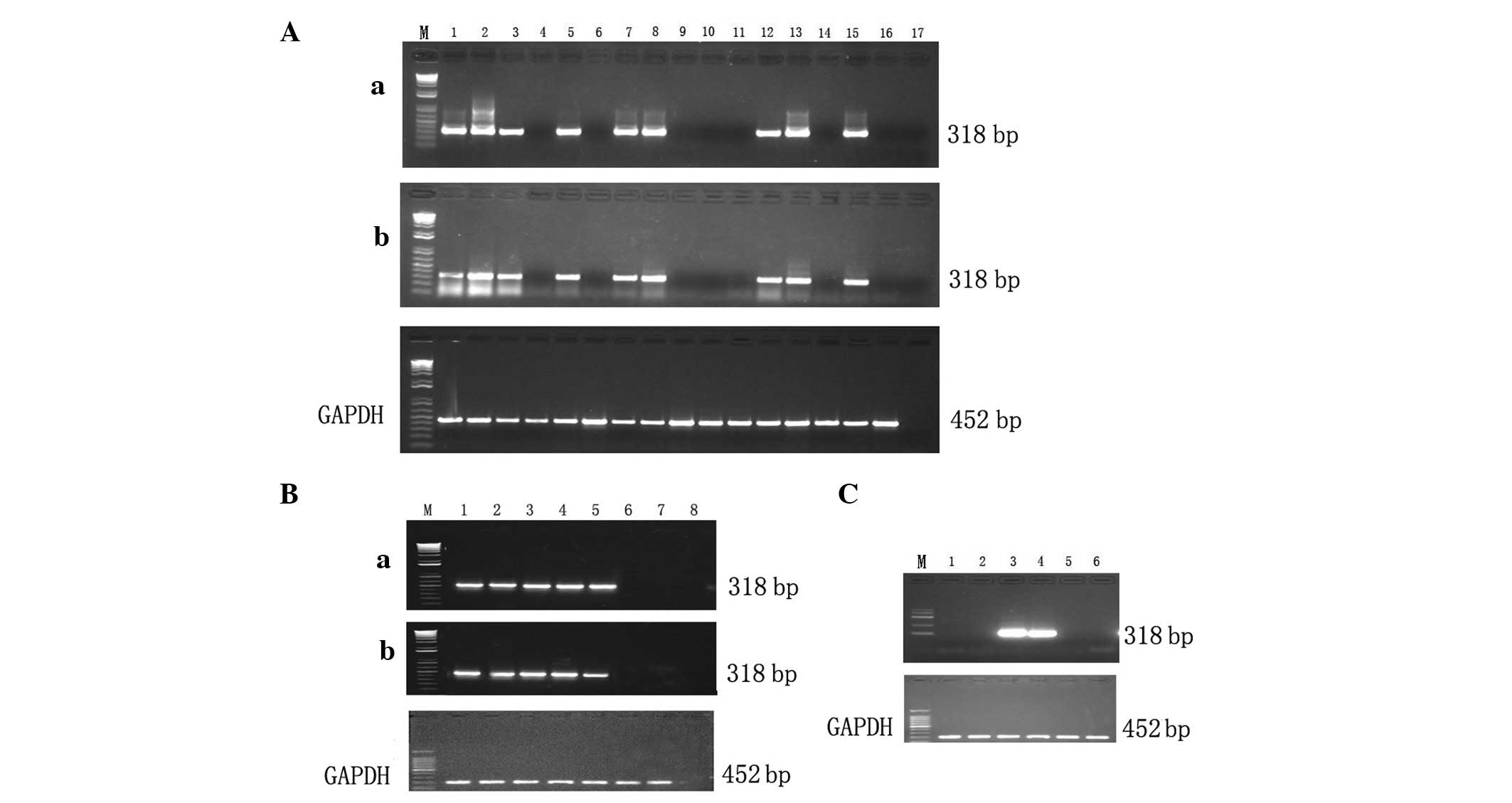
the two assays (Fig. 1A). The
relative sensitivity was determined by a 10-fold serial dilution of
the breast cancer MCF-7 cell line using PBMCs obtained from the
healthy donors. The breast cancer MCF-7 cell line was detected at a
dilution of 10−6 using the rapid nested PCR and the
traditional nested PCR techniques, indicating that the two assays
exhibit the same sensitivity (Fig.
1B). The target bands were produced with outer and inner
primers, while no target bands were amplified using only outer or
inner primers (Fig. 1C). The
amplification times were 65 and 89 min for the rapid and
traditional nested PCR assays, respectively, shortening the total
duration to 24 min.
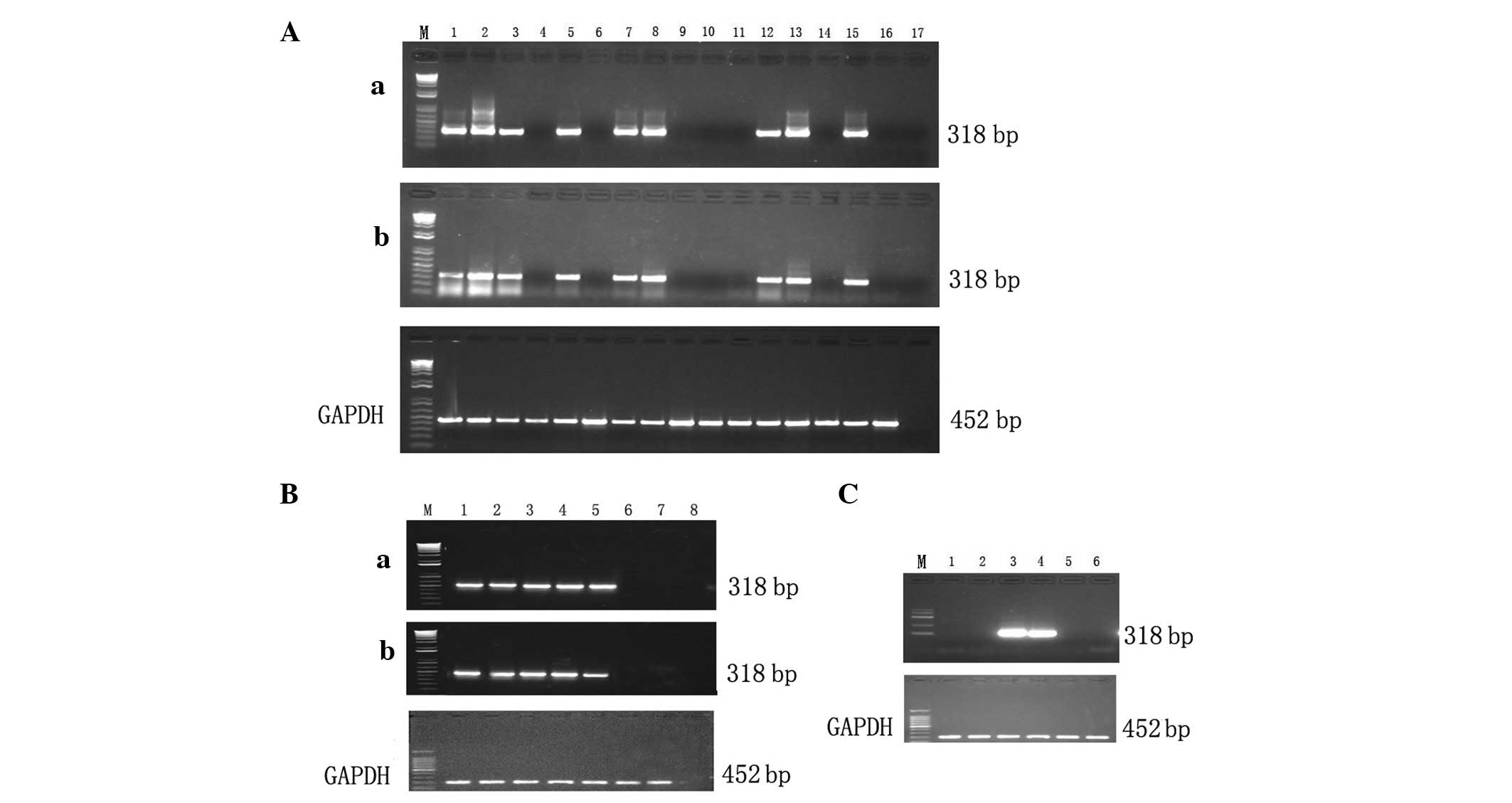 | Figure 1Evaluation of the rapid nested
polymerase chain reaction (PCR). (A) The same detection rate was
achieved using the (a) novel rapid and the (b) traditional nested
PCR assays. Lanes 1–15, breast cancer patients; lane 16, healthy
donor; and lane 17, negative control. (B) Sensitivity of the (a)
novel rapid and the (b) traditional nested PCR assays. Lanes 1–7,
10-fold serial dilution of MCF-7 using peripheral blood mononuclear
cells obtained from healthy donors (Lane 1, 102; lane, 2
103; lane 3, 104; lane 4, 105;
lane 5, 106; lane 6, 107; and lane 7,
108 cells); and lane 8, negative control. (C)
Amplification using outer and inner primers. Lanes 1 and 2, outer
primers only; lanes 3 and 4, outer and inner primers; and lanes 5
and 6, inner primers only. |
Enhancement of positive detection rate
with multiple markers
The three candidate markers, FAM83A, NPY1R and
KRT19, were investigated further in a large cohort consisting of
142 breast cancer patients and 60 healthy controls, using the novel
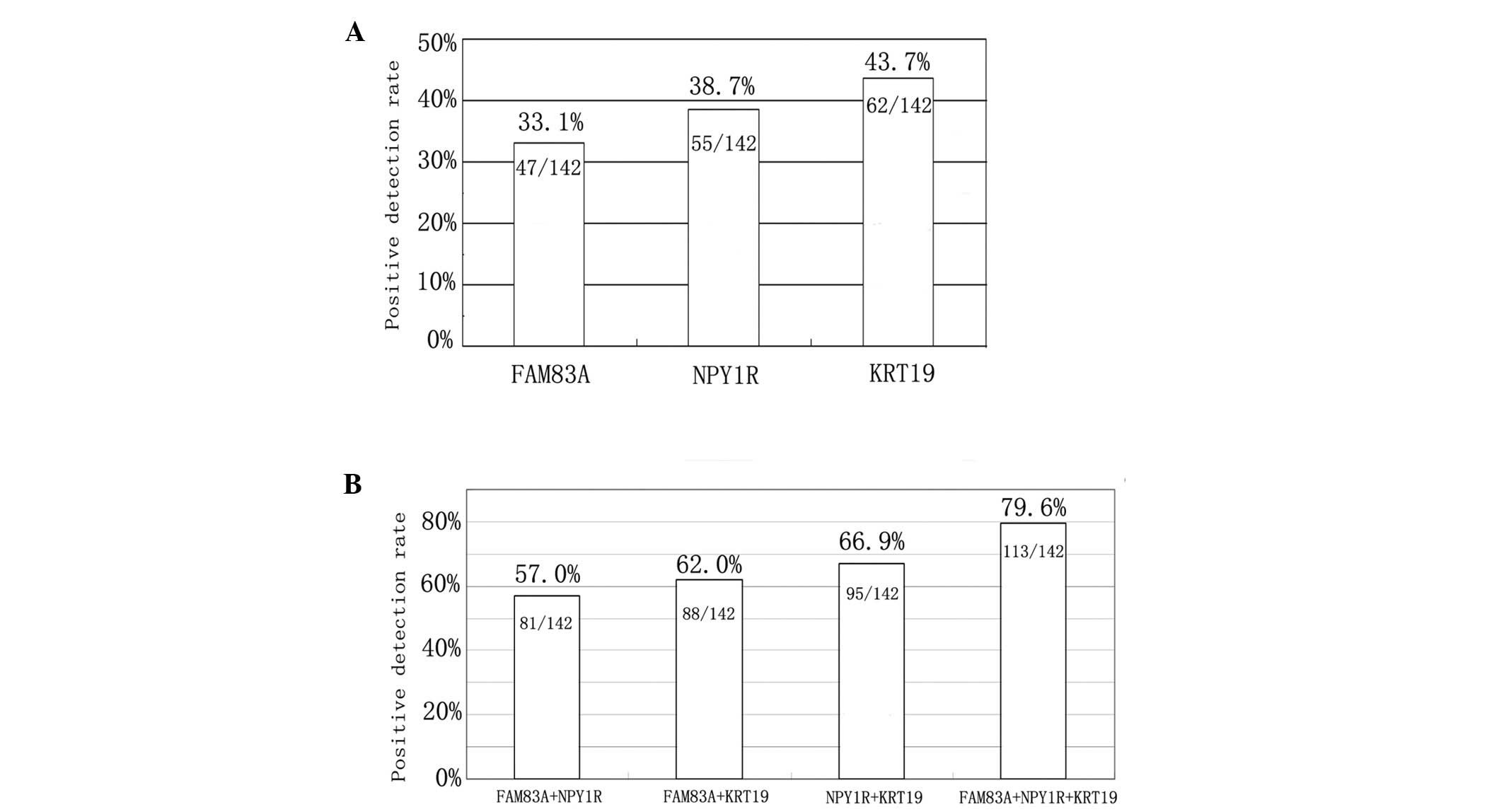
rapid nested PCR assay. As shown in Fig. 2A, the positive detection rate of
circulating cancer cells in breast cancer patients was 33.1
(47/142), 38.7 (55/142) and 43.7% (62/142) for the FAM83A, NPY1R
and KRT19 genes, respectively. The FAM83A and NPY1R transcripts
were undetectable in the PBMC samples of the 60 healthy controls,
whereas the KRT19 marker was detected in three of the healthy
samples. The fraction of positives among all of the patients are
indicated in Fig. 2 and ≤79.6%
(113/142) of the breast cancer patient blood samples were found to
be positive for at least one of the markers. The novel panel of the
three gene markers, FAM83A, NPY1R and KRT19, was found to be
significantly superior to the individual markers or any combination
of two markers. These results identified that using multiple
markers improves the positive detection rate (Fig. 2B).
Tumor marker detection and patient
characteristics
The statistical analysis was performed to determine
the correlation between marker expression frequency and
clinicopathological variables. With regard to the clinical stage,
the detection rate of FAM83A and NPY1R, as well as the panel of
markers, was significantly higher in patients with stage III or IV
breast cancer when compared with stage I or II patients
(P<0.05). The detection rate of the three marker genes, or at
least one of the three markers, was found to correlate with the
occurrence of distant metastasis (P<0.05), which indicated the
benefit of the panel as a predictive peripheral blood marker for
metastasis in breast cancer. In addition, the expression rate of
NPY1R was significantly higher in ER−, PgR− or
HER2/neu-positive patients when compared with ER−, PgR− or
HER2/neu-negative patients (P<0.05). However, no
statistically significant correlation was identified between marker
detection and tumor size, pathology type or patient age (P>0.05;
Table II).
 | Table IICharacteristics and tumor marker
expression in the circulating cancer cells of breast cancer
patients. |
Table II
Characteristics and tumor marker
expression in the circulating cancer cells of breast cancer
patients.
| Characteristic | n | FAM83A, n (%) | NPY1R, n (%) | KRT19, n (%) | Positive ratea, n (%) |
|---|
| Age, years |
| <50 | 56 | 17 (30.4) | 21 (37.5) | 25 (44.6) | 46 (82.1) |
| ≥50 | 86 | 30 (34.9) | 34 (39.5) | 37 (43.0) | 67 (77.9) |
| Pathology |
| Invasive ductal
carcinoma | 98 | 33 (33.7) | 38 (38.8) | 43 (43.9) | 78 (79.6) |
| Simple cancer | 7 | 2 (28.6) | 3 (42.9) | 3 (42.9) | 6 (85.7) |
| Eczematous
cancer | 5 | 2 (40.0) | 2 (40.0) | 2 (40.0) | 4 (80.0) |
| Medullary
carcinoma | 19 | 6 (31.6) | 7 (36.8) | 8 (42.1) | 15 (78.9) |
| Invasive lobular
carcinoma | 13 | 4 (30.8) | 5 (38.5) | 6 (46.2) | 10 (76.9) |
| Tumor size, cm |
| ≤2 | 75 | 25 (33.3) | 29 (38.7) | 32 (42.7) | 59 (78.7) |
| >2 | 67 | 22 (32.8) | 26 (38.8) | 30 (44.8) | 54 (80.6) |
| Clinical stage |
| I, II | 89 | 22 (24.7) | 27 (30.3) | 36 (40.4) | 64 (71.9) |
| III, IV | 53 | 25 (47.2)b | 28 (52.8)b | 26 (49.1) | 49 (92.5)b |
| Distant
metastases |
| No | 121 | 36 (29.8) | 42 (34.7) | 48 (39.7) | 93 (76.9) |
| Yes | 21 | 11 (52.4)b | 13 (61.9)b | 14 (66.7)b | 20 (95.2)b |
| Estrogen receptor
status |
| Positive | 101 | 34 (33.7) | 44 (43.6)b | 45 (44.6) | 82 (81.2) |
| Negative | 41 | 13 (31.7) | 11 (26.8) | 17 (41.5) | 31 (75.6) |
| Progesterone
receptor status |
| Positive | 89 | 30 (33.7) | 40 (44.9)b | 41 (46.1) | 71 (79.8) |
| Negative | 53 | 17 (32.1) | 15 (28.3) | 21 (39.6) | 42 (79.2) |
| HER-2/neu
receptor status |
| Positive | 50 | 19 (38.0) | 25 (50.0)b | 23 (46.0) | 40 (80.0) |
| Negative | 92 | 28 (30.4) | 30 (32.6) | 39 (42.4) | 73 (79.3) |
Correlation between tumor marker gene
detection and disease progression
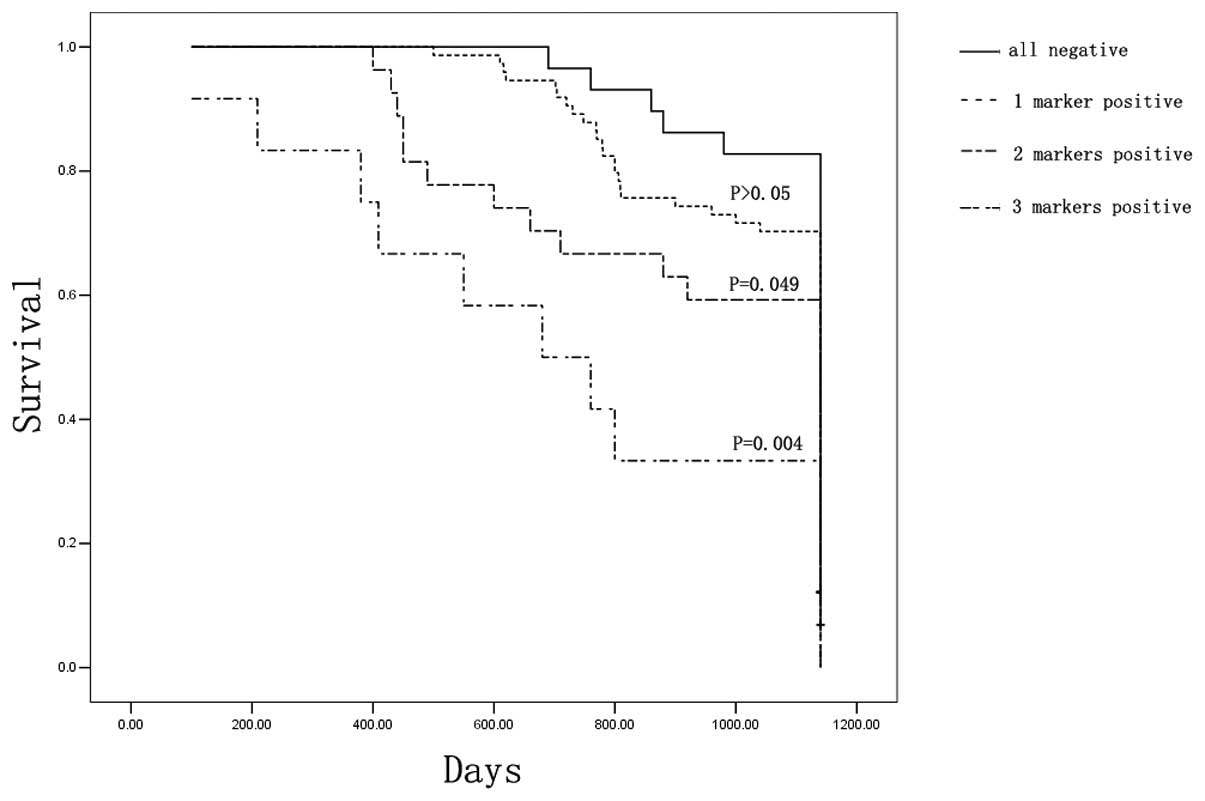
To investigate the correlation between the detection
of circulating cancer cells and the clinical outcome of breast
cancer patients, a follow-up study was performed for 38 months in
142 patients following surgical removal of the tumor mass. The
survival rate was 82.8% (24/29) for the all-negative patients
(those that exhibited no tumor markers), 70.3% (52/74) for patients
that were positive for a single tumor marker, 59.3% (16/27) for
patients that were positive for two tumor markers and 33.3% (4/12)
for patients that were positive for three tumor markers. In
addition, the Kaplan-Meier analysis and log-rank test indicated no
difference in the overall survival rate between the all-negative
and single-positive marker patients (P>0.05). However, patients
that were positive for more than one tumor marker exhibited a
significant overall disadvantage when compared with the
all-negative patients (P<0.05; Fig.
3).
Discussion
The detection of circulating cancer cells is a
promising and powerful tool for cancer diagnosis and disease
monitoring (5). However, due to the
heterogeneous expression of individual markers in tumor lesions
within individual patients or among patients, the predictive power
of a single marker is relatively limited. In the present study,
in sillico analysis was performed to identify a panel of
marker genes for the detection of breast cancer cells dispersed in
the circulation. Based on the experimental results of the current
study, the National Cancer Institute-Cancer Genome Anatomy Project
database and Digital Gene Expression Displayer program were
considered to be useful tools for establishing the genes that were
expressed between the two pools of samples. However, this is only
reliable when a sufficient quantity of expressed sequence tag
libraries for the tissue of interest are archived in the database
(6).
The differentially expressed genes can be further
developed into marker genes for diagnostic or prognostic purpose by
experimental verification procedures such as RT-PCR. The favorable
marker must exhibit a high level of expression in breast cancer
tissues, however, no or low expression in healthy PBMCs. In
addition, the current study identified a novel panel of marker
genes (FAM83A, NPY1R and KRT19) for the detection of cancer cells
in the peripheral blood of breast cancer patients. KRT19 is a
characteristic marker of epithelial cells (7), whereas FAM83A is a novel biomarker for
detection of the peripheral blood, which was identified as a
tumor-specific gene in our previous study (8). Furthermore, the FAM83A mRNA transcript
was expressed in 21 of 40 lung cancer samples (52.5%), 24 of 50
breast cancer samples (48.0%), four of 12 colon cancer samples
(33.3%) and three of 10 gastric cancer tissues (30.0%), however,
was not detected in the 16 healthy tissues. The overall positive
rate of FAM83 gene expression in the peripheral blood was 34.3%
(24/70) (8).
NPY1R was the first NPY receptor subtype to be
cloned and characterized. Previous studies revealed that normal
breast tissue expresses the Y2R subtype, whereas 85% of human
breast carcinoma express NPY1R (9).
It has been proposed that an interaction between estrogen, and NPY
and its receptors illustrates the concerted action of estrogen and
progesterone on increasing NPY levels, which results in an
associated increase in the release of luteinizing hormone (10). In the current study, the expression
of the marker gene, NPY1R, in peripheral blood was found to
correlate with the expression of ER and PgR, whereby the expression
rate of NPY1R was significantly higher in the ER− and PgR-positive
group compared with that in the ER− and PgR-negative group.
Furthermore, the results indicated that estrogen is important in
the upregulation of NPY1R, which in turn regulates estrogen-induced
cell proliferation in breast cancer cells (11).
The number of circulating cancer cells is so
marginal that they cannot be detected using conventional diagnostic
methods. Various techniques have been developed to enrich certain
types of cells from the blood and to characterize these cells using
nested RT-PCR assays, which is extremely sensitive and capable of
detecting one breast cancer cell in 107 cells; however,
this two-step, time-consuming method is less suitable for clinical
application. To overcome this problem, the current study developed
a simple and rapid nested PCR assay, which is less time-consuming
and, therefore, more readily applicable to the clinical
investigation of relatively large sample numbers in clinical
practice. Firstly, two pairs of primers were designed, that had
marked differences in their annealing temperatures, (72 and 60°C
for outer and inner primers, respectively). The two steps of the
nested PCR reaction were performed in one tube. The first step
consisted of heating the reaction to 95°C, causing the denaturation
of the DNA template. Next, the reaction temperature was lowered to
72°C to allow annealing of the outer primers to the single-stranded
DNA template. Following 30 cycles of amplification, a 100-fold
dilution of the outer primers (0.2 μmol) was depleted to achieve a
large amount of product in the tube, which was denatured upon
reheating the reaction to 95°C. The reaction temperature was
lowered to 60°C to allow the annealing of the inner primers to the
single-stranded product template. It was verified that the target
bands were produced with the outer and inner primers; however, none
of the target bands were amplified with only the outer or inner
primers.
The duration of the reaction using the improved
method was ~1 hr; the volume of the PCR mix was 25 μl and the PCR
reagents were added using a one-step method. The amplification
results indicated that the PCR factors used were effective and that
the enzymatic activity of the Taq DNA polymerase had been
preserved. The specificity and sensitivity of the amplification
were the same as those of the traditional method, and the cost of
the test was reduced proportionally due to the decreased use of
reagents.
In conclusion, the current study developed a novel
rapid nested PCR assay to detect circulating cancer cells in the
blood of breast cancer patients using a novel panel of marker
genes, FAM83A, NPY1R and KRT19. This assay may present a useful
tool for the prediction of cancer metastasis in breast cancer
patients and for the evaluation of their prognosis.
Acknowledgements
The current study was supported by grants from the
Hebei Provincial Population and Family Planning Commission (grant
no. 2009-B21) and the Hebei Provincial Bureau of Health (grant no.
20090579).
References
|
1
|
Gardner B and Feldman J: Are positive
axillary nodes in breast cancer markers for incurable disease? Ann
Surg. 218:270–278. 1993. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Zhao S, Yang H, Zhang M, et al:
Circulating tumor cells (CTCs) detected by triple-marker EpCAM,
CK19, and hMAM RT-PCR and their relation to clinical outcome in
metastatic breast cancer patients. Cell Biochem Biophys.
65:263–273. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Reinholz MM, Nibbe A, Jonart LM, et al:
Evaluation of a panel of tumor markers for molecular detection of
circulating cancer cells in women with suspected breast cancer.
Clin Cancer Res. 11:3722–3732. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Margossian A, Diaz J and Corvalan A: In
silico analysis of breast cancer transcriptome libraries
distinguish tumor subclasses. Cancer Res. 69(Suppl 3): S11652009.
View Article : Google Scholar
|
|
5
|
Rahbari NN, Bork U, Motschall E, et al:
Molecular detection of tumor cells in regional lymph nodes is
associated with disease recurrence and poor survival in
node-negative colorectal cancer: a systematic review and
meta-analysis. J Clin Oncol. 30:60–70. 2012. View Article : Google Scholar
|
|
6
|
Kavak E, Unlü M, Nistér M and Koman A:
Meta-analysis of cancer gene expression signatures reveals new
cancer genes, SAGE tags and tumor associated regions of
co-regulation. Nucleic Acids Res. 38:7008–7021. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Liu L, Liao GQ, He P, et al: Detection of
circulating cancer cells in lung cancer patients with a panel of
marker genes. Biochem Biophys Res Commun. 372:756–760. 2008.
View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Li Y, Dong X, Yin Y, et al: BJ-TSA-9, a
novel human tumor-specific gene, has potential as a biomarker of
lung cancer. Neoplasia. 7:1073–1080. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Reubi JC, Gugger M, Waser B and Schaer JC:
Y(1)-mediated effect of neuropeptide Y in cancer: breast carcinomas
as targets. Cancer Res. 61:4636–4641. 2001.PubMed/NCBI
|
|
10
|
Sheriff S, Ali M, Yahya A, et al:
Neuropeptide Y Y5 receptor promotes cell growth through
extracellular signal-regulated kinase signaling and cyclic AMP
inhibition in a human breast cancer cell line. Mol Cancer Res.
8:604–614. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Amlal H, Faroqui S, Balasubramaniam A and
Sheriff S: Estrogen up-regulates neuropeptide Y Y1 receptor
expression in a human breast cancer cell line. Cancer Res.
66:3706–3714. 2006. View Article : Google Scholar : PubMed/NCBI
|