Introduction
Intraosseous epithelioid vascular tumors are
generally classified as epithelioid hemangiomas (EHs), epithelioid
hemangioendotheliomas (EHEs) or epithelioid angiosarcomas (EAs)
(1–4). In addition, all of these tumor types
may express the epithelial marker, cytokeratin, in addition to
endothelial markers and vimentin (5). EA is a rare high-grade sarcoma of
intraosseous vascular endothelial origin and is a rare variant of
angiosarcoma. EA is characterized by rapidly proliferating, large
polygonal epithelioid malignant cells with marked cellular
pleomorphisms (6). As a result, the
clinical/radiological presentation and cellular morphology of EA
may be confused with multiple myeloma or metastatic carcinoma
(5,7). Furthermore, focal areas of
vasoformation and positivity for endothelial markers may lead to a
misdiagnosis of other vascular bone tumors. EA has been found in
the soft tissue, skin, adrenal gland, thyroid gland, vagina,
uterus, breasts, lungs and gallbladder, but rarely in the bone
(7–10). Thus, the presentation of EA in the
spine is particularly rare. Consequently, the current study
presents a case of a 76-year-old male with EA of the fourth lumbar
(L4) vertebra. Patient provided written informed consent and the
study was approved by the ethics committee of Wenzhou Medical
University (Zhejiang, China).
Case report
Presentation and examination
In December 2013, a 76-year-old male presented to
the Department of Orthopedics, The First Affiliated Hospital of
Wenzhou Medical University (Wenzhou, China) with progressive pain
over the mid-lumbar spine and a dull, aching and constant pain over
the left side of the lumbar of five months. Subsequently, a root
pain corresponding to the L4 dermatome was identified, which was
aggravated by walking. A physical examination revealed the muscle
strength and sensation to be weak in the left lower limb, and
tenderness and percussion pain were present over the L4 vertebra.
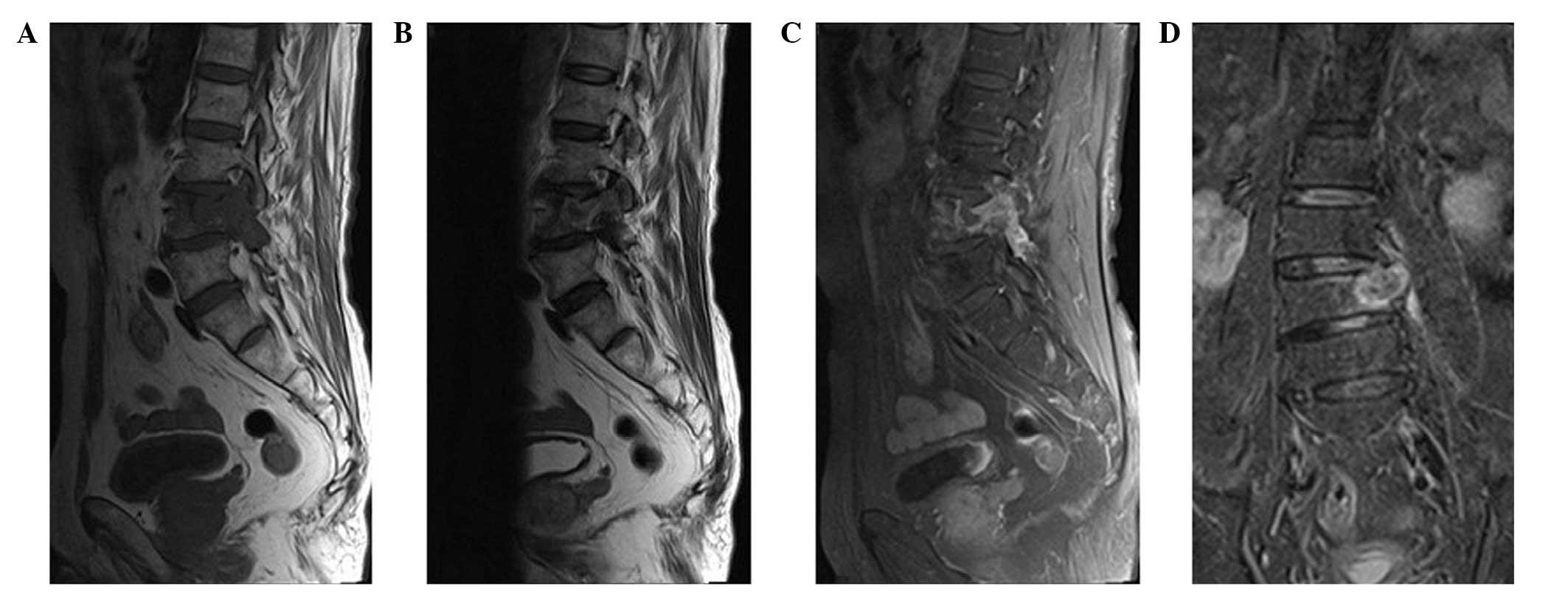
Magnetic resonance imaging (MRI) also detected a destructive soft
tissue lesion occupying the L4 vertebral region, accompanied by
moderate compression of the adjacent spinal cord which involved the
pedicle and lamina. A knuckle deformity of the L4 vertebra was also
observed, as well as cystic lesions present on T1-weighted images,
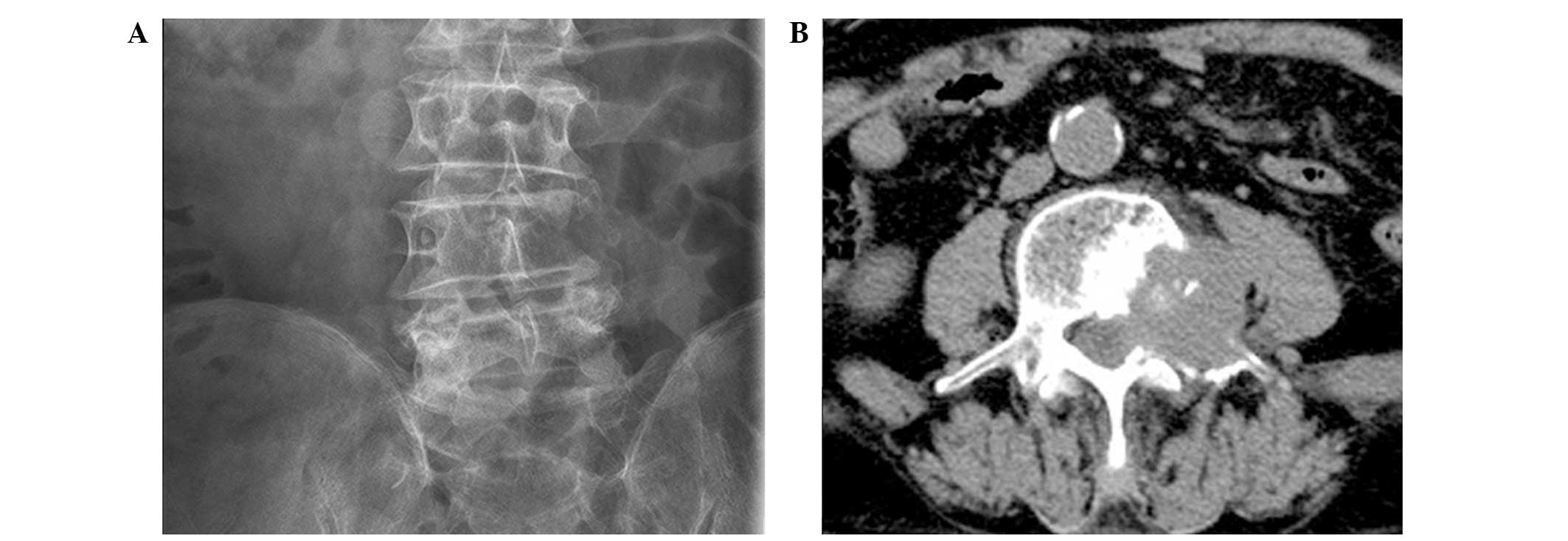
which exhibited high intensities on T2-weighted images (Fig. 1). Computed tomography (CT) scans
revealed the presence of an osteolytic lesion with ill-defined
margins, which extended into the proximal soft tissue (Fig. 2). In addition, erosion of the cortex
of the L4 was observed.
Treatment
To decompress the spinal cord, a laminectomy of the
L4 vertebra was performed. The lesion involved was 5 cm in length
and 4 cm wide, and included the cystic and necrotic areas. The
tumor was also poorly defined, had eroded the cortex and extended
into adjacent soft tissue in an infiltrative pattern. A biopsy from
the L4 vertebra revealed sections of softened bone, as well as
areas of hemorrhage, necrosis and blood spaces; a phenotype
distinctive of a red, hemorrhagic and friable tumor. In addition, a
biopsy of the lesion was obtained.
Histological examination
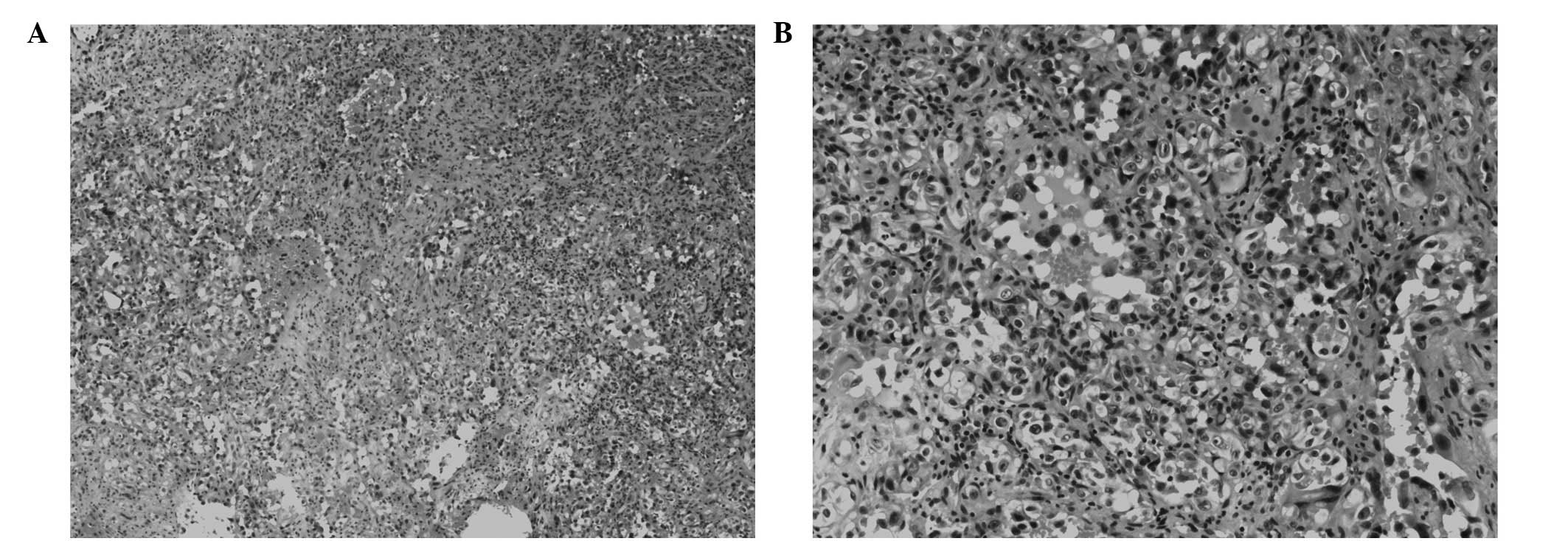
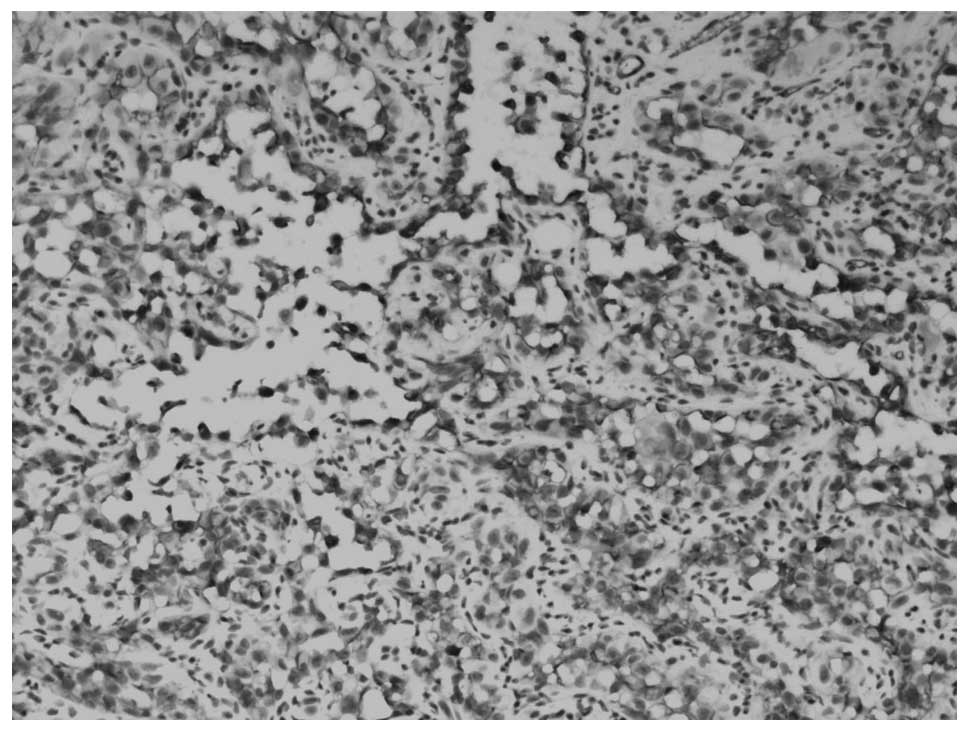
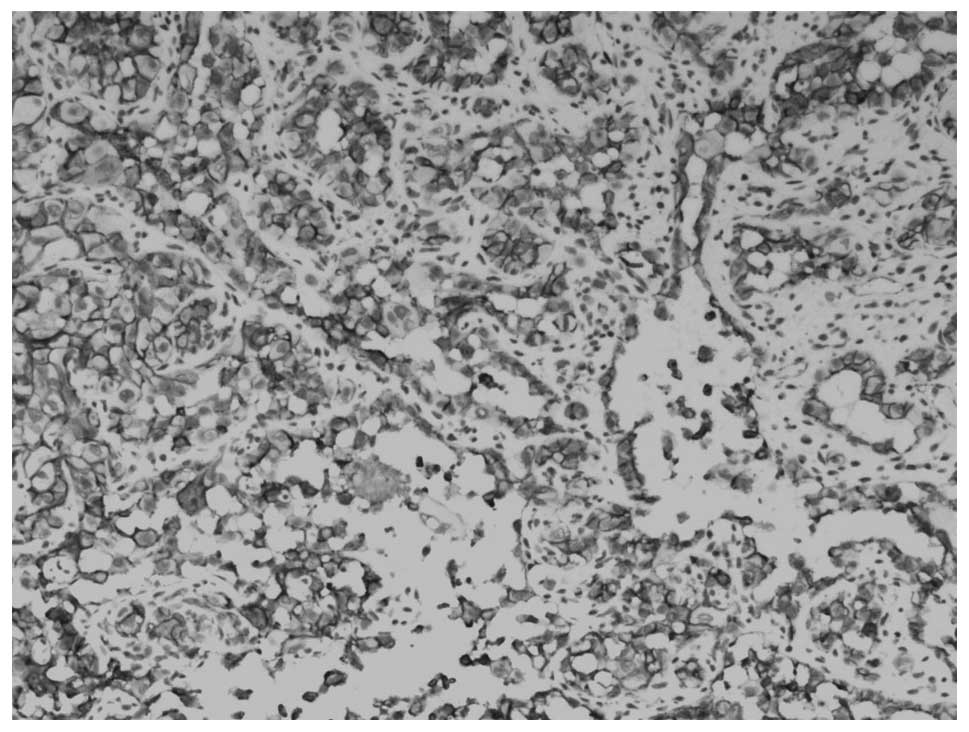
Hematoxylin-eosin staining was performed and sheets
and nests of large, pleomorphic, round-to-polygonal epithelioid
cells were observed. The cells exhibited abundant eosinophilic
cytoplasm, vesicular nuclei and prominent nucleoli. Numerous brisk
mitosis events exhibiting cellular pleomorphism were also observed
and in certain areas, irregularly dilated vascular formations
adjacent to the solid tissue were detected. Blood-filled channels
were also found to be lined with epithelioid tumor cells, which
provided a papillary appearance (Fig.
3). The stroma consisted predominantly of thin fibrovascular
connective tissue, as well as varying degrees of hemorrhage, cystic
changes and necrosis. Foci of prominent neutrophilic infiltrate
were also observed (Fig. 3).
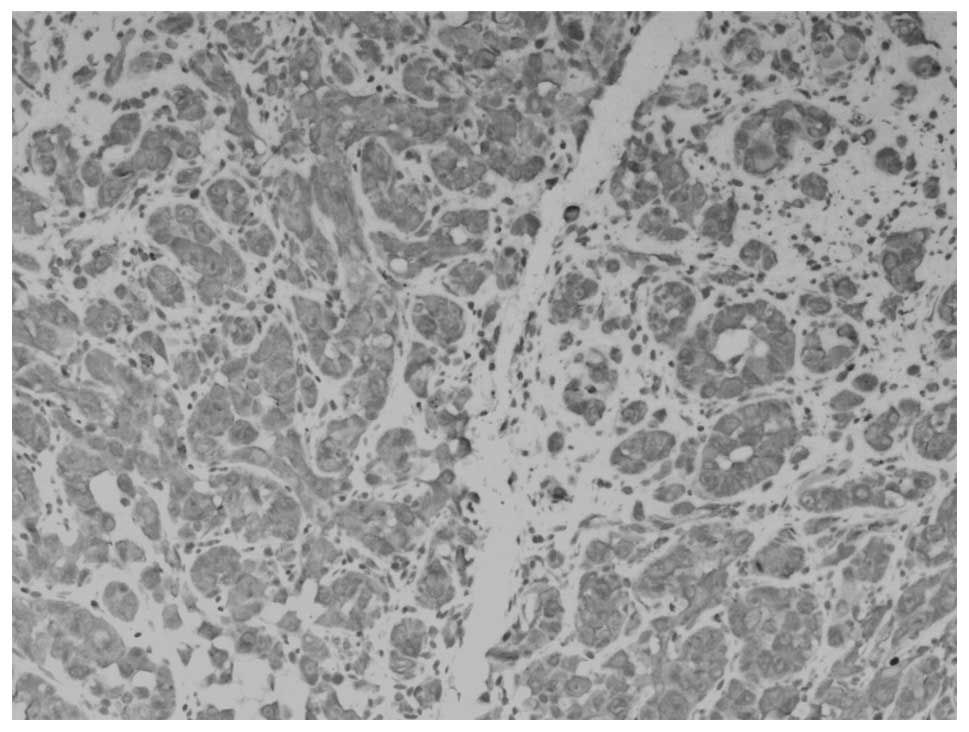
Furthermore, in the immunohistochemistry assays, tumor cells were
positive for vimentin (Fig. 4),
CD34 (Fig. 5) and CD31 (Fig. 6) expression and negative for the
epithelial membrane antigen (EMA). These results supported an
endothelioid-related origin of the tumor.
Postoperative course
The patient refused further therapy and was
monitored for six months. At the time of writing, no evidence of
tumor recurrence has been detected.
Discussion
EA is a rare epithelioid vascular tumor of the bone,
which accounts for <1% of all primary skeletal malignancies
(6,11). The term EA refers to a variant of
angiosarcoma which is characterized by tumor cells with an
epithelioid morphology and these cells occasionally exhibit a
pseudoglandular or alveolar arrangement (6,8). EA
has previously been recognized in extraosseous sites, however, only
a few cases of this rare variant have been documented in the bone
(5,10). In addition, skeletal angiosarcoma
tends to affect middle-aged and older individuals, has a marginal
predominance for males and tends to affect the long tubular bones
of the lower extremities, such as the femur and tibia (7,12).
Literature regarding EA of the bone is limited to only a few case
reports (6). Of these, Balicki
et al (5) reported a case of
multicentric EA in the two femurs of a 71-year-old patient and
Marthya et al (13) reported
a case of multicentric EA in the spine of a 65-year-old patient.
Multicentricity has been observed in 20–50% of EA cases and
consists of multiple lesions in a single bone, in the same
extremity or throughout the skeleton. In CT and MRI scans, osseous
destruction, central necrosis and marginal hyperperfusion of the
soft tissue masses indicate the presence of an aggressive,
high-grade bone tumor. However, the non-specific appearance of bone
tumors may lead to a misdiagnosis of metastasis or multiple
myeloma. Typically, EA positively stains for cytokeratins,
including EMA and a variable proportion of EAs are positive for
cytokeratin. In certain cases, a sheeted, epithelioid appearance is
accompanied by positive cytokeratin staining. EA also closely
mimics metastatic lesions and therefore, accurate diagnosis is
difficult. Thus, an immunohistochemical examination of
vasoformation may be informative and essential. In the present
study, the tumor examined exhibited epithelioid morphology, with
sheets and clusters of tumor cells characterized by prominent
nucleoli and abundant eosinophilic cytoplasm. In addition,
anastomosing vascular channels lined by layers of atypical
endothelial cells were observed, which exhibited an anaplastic,
immature appearance (8,10).
EA is associated with positive immunostaining for
endothelial markers, including CD34 and CD31. Furthermore, CD31 is
expressed by ~90% of angiosarcomas, but <1% of carcinomas and
thus, CD31 is considered to provide a relatively high index of
sensitivity and specificity (7,13).
CD34 is also reported to be expressed by >90% of vascular
tumors, however, this marker is much less specific and is expressed
by several other soft tissue tumors (7). The immunoreactivity of factor
VIII-related antigen can also be informative, although, it is
variable for the diagnosis of bone EA. For example, it is often
positive in epithelioid tumors, rather than conventional tumors. In
addition, vimentin is a marker that is non-specifically expressed
by all epithelioid vascular tumors (5). However, even in the absence of clear
vascular differentiation, abundant intratumoral hemorrhage and the
presence of intratumoral neutrophils are morphological changes that
suggest a vascular origin (6,13).
With regard to the clinical behavior and prognosis
of skeletal angiosarcoma, the majority of affected patients succumb
to the disease within one year of diagnosis (5,6,13).
Consistent with this poor prognosis, EA of bone is considered an
aggressive high-grade tumor. The main differential diagnosis of EA
of the bone includes the presence of other epithelioid vascular
tumors, including EH, EHE or metastatic carcinoma (13). In addition, angiosarcoma of the bone
usually presents with dull aching pain over the affected region
(13) and the clinical course may
progress to widespread and distant metastasis, which commonly
affects lung and lymph node tissue (6). Radiological detection of EA is
non-specific and typically includes an osteolytic lesion without
periosteal reaction and soft tissue masses with cortical permeation
(6). Furthermore, erosion of the
cortex with soft tissue involvement may also be observed.
The most important differential diagnosis of EA is
EHE, which is regarded as a vascular tumor of low-grade or
borderline malignancy (14,15). While EHE shares a number of
histopathological features with EA, EHE can be distinguished by the
presence of pronounced, bland-appearing atypical cells, fewer
cytoplasmic vacuoles, a lack of chondromyxoid and myxohyaline
matrix, as well as a scarcity of endothelioid cells exhibiting
cord-like growth and a less aggressive phenotype (12,13).
Distinguishing EA from EHE and metastasis is important due to the
significant differences in clinical treatment and prognosis of each
(16). While the standard treatment
for EA includes wide resection, chemotherapy and radiotherapy
(6), an accurate diagnosis is
required to avoid overtreatment.
EA and metastasis may involve multiple bone sites,
affect older individuals and involve sheets of epithelioid tumor
cells that tend to express keratin and EMA. As a result, a
diagnostic bias may exist among pathologists and clinicians
(17). Therefore, multicentric bone
EA is easily misdiagnosed as metastatic carcinoma (18). However, metastatic lesions are
almost always negative for the expression of CD34 and CD31, and
lesions of EA are usually >5 cm in size (18). The latter is also associated with a
significantly poorer prognosis. In the present study, the patient
was initially misdiagnosed with metastatic carcinoma, however,
vascular channels lined by atypical epithelioid cells and the
immunohistochemistry results suggested a vasoformative tumor. In
addition, the presence of an intratumoral neutrophilic infiltrate
combined with the endothelioid nature of the cells confirmed a
diagnosis of EA.
An additional differential diagnosis of EA is EH,
which typically affects patients between the second and eighth
decades of life, particularly those that are solitary. The long
tubular bones are also most commonly affected by well-circumscribed
lesions. Furthermore, well-formed vessels and a lobular growth
pattern are characteristic of this tumor, in addition to an absence
of severe nuclear atypia, which presents the benign nature of this
tumor (13,19). By contrast, EHE is characterized by
occasional grooves, fine chromatin, small nucleoli, mitotic counts
of <5/10 high power fields and nuclear atypia. However, the
latter presents to a lesser extent in EHE than compared with EA. An
inflammatory component in the stroma, which is abundant in
eosinophils and plasma cells also tends to accompany EHE (12,17).
Distinguishing EA from EHE, metastasis and EH is
important due to significant differences in clinical behavior,
treatment and prognosis for these conditions (13). In the English literature, no reports
of EA presentation in the L4 region of the spine have been found.
However, of the reported cases of EA, treatment usually includes
wide resection, chemotherapy and radiotherapy. In the present
study, treatment only included decompression of the L4 spine, as
the patient refused further therapy. However, at the time of
writing, six months following treatment, the tumor remains under
control and the patient is asymptomatic. Furthermore, no evidence
of tumor recurrence has been identified.
In conclusion, bone EA is rare and thus, the careful
determination from EHE, EH and metastatic carcinoma is required due
to differences in the management and clinical treatment for these
conditions. The present study provides additional characterization
of bone EA and emphasizes the utility of histopathological and
immunohistochemical evaluations for its correct diagnosis,
treatment and prognosis for individuals with this deceptive
disease.
Abbreviations:
|
EA
|
epithelioid angiosarcoma
|
|
EHE
|
epithelioid heamangioendothelioma
|
|
EH
|
epithelioid hemangioma
|
|
MRI
|
magnetic resonance imaging
|
|
CT
|
computed tomography
|
References
|
1
|
Errani C, Vanel D, Gambarotti M, et al:
Vascular bone tumors: a proposal of a classification based on
clinicopathological, radiographic and genetic features. Skeletal
Radiol. 41:1495–1507. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Hisaoka M, Okamoto S, Aoki T, Yokoyama K
and Hashimoto H: Spinal epithelioid hemangioendothelioma with
epithelioid angiosarcomatous areas. Skeletal Radiol. 34:745–749.
2005. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
O’Connell JX, Nielsen GP and Rosenberg AE:
Epithelioid vascular tumors of bone: a review and proposal of a
classification scheme. Adv Anat Pathol. 8:74–82. 2001.PubMed/NCBI
|
|
4
|
Skuletić V, Bokun R, Tatomirović Z and
Popović L: Epithelioid vascular tumor. Vojnosanit Pregl. 59(Suppl
6): S103–S107. 2002.(In Serbian).
|
|
5
|
Balicki D, Buhrmann R, Maclean J, et al:
Multicentric epithelioid angiosarcoma of the bone. Pitfalls in
clinical and morphological diagnosis. Blood Cells Mol Dis.
22:205–213. 1996. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Deshpande V, Rosenberg AE, O’Connell JX
and Nielsen GP: Epithelioid angiosarcoma of the bone: a series of
10 cases. Am J Surg Pathol. 27:709–716. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Yang Z, Tao H, Ye Z and Yang D:
Multicentric epithelioid angiosarcoma of bone. Orthopedics.
35:e1293–e1296. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Hart J and Mandavilli S: Epithelioid
angiosarcoma: a brief diagnostic review and differential diagnosis.
Arch Pathol Lab Med. 135:268–272. 2011.PubMed/NCBI
|
|
9
|
Lamovec J, Zidar A and Zidanik B:
Epithelioid angiosarcoma of the thyroid gland. Report of two cases.
Arch Pathol Lab Med. 118:642–646. 1994.PubMed/NCBI
|
|
10
|
Meis-Kindblom JM and Kindblom LG:
Angiosarcoma of soft tissue: a study of 80 cases. Am J Surg Pathol.
22:683–697. 1998. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Hasegawa T, Fujii Y, Seki K, et al:
Epithelioid angiosarcoma of bone. Hum Pathol. 28:985–989. 1997.
View Article : Google Scholar
|
|
12
|
Kudva R, Perveen S and Janardhana A:
Primary epithelioid angiosarcoma of bone: a case report with
immunohistochemical study. Indian J Pathol Microbiol. 53:811–813.
2010. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Marthya A, Patinharayil G, Puthezeth K,
Sreedharan S, Kumar A and Kumaran CM: Multicentric epithelioid
angiosarcoma of the spine: a case report of a rare bone tumor.
Spine J. 7:716–719. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Aquilina K, Lim C, Kamel MH, Marks CJ,
O’Sullivan MG and Keohane C: Epithelioid hemangioendothelioma of
the spine. Report of two cases. J Neurosurg Spine. 3:393–399. 2005.
View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Arena V, Pennacchia I, Carbone A and
Vecchio FM: Epithelioid hemangioendothelioma of the bone and
intestinal infarction: an unusual association. Colorectal Dis.
13:e69–e70. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Ledson MJ, Convery R, Carty A and Evans
CC: Epithelioid haemangioendothelioma. Thorax. 54:560–561. 1999.
View Article : Google Scholar
|
|
17
|
O’Connell JX, Kattapuram SV, Mankin HJ,
Bhan AK and Rosenberg AE: Epithelioid hemangioma of bone. A tumor
often mistaken for low-grade angiosarcoma or malignant
hemangioendothelioma. Am J Surg Pathol. 17:610–617. 1993.PubMed/NCBI
|
|
18
|
Santeusanio G, Bombonati A, Tarantino U,
et al: Multifocal epithelioid angiosarcoma of bone: a potential
pitfall in the differential diagnosis with metastatic carcinoma.
Appl Immunohistochem Mol Morphol. 11:359–363. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Sung MS, Kim YS and Resnick D: Epithelioid
hemangioma of bone. Skeletal Radiol. 29:530–534. 2000. View Article : Google Scholar
|