Introduction
Numerous cancer survivors are afflicted with
long-term complications of cytotoxic treatment (1), of which the most critical one is the
development of secondary neoplasia, including myelodysplastic
syndrome (MDS). However, cases of solid tumors subsequent to or
simultaneously with primary MDS have rarely been reported. A study
by Kondo and Shinbo (2) reported a
62-year-old male suffering from MDS and gastric cancer. A study by
Takahashi et al (3) reported
a 66-year-old male suffering from MDS associated with synchronous
double cancers of the stomach and the papilla of Vater. The current
study presents the case of cervical cancer with an 8-year history
of MDS. The study was approved by the ethics committee of The First
Affiliated Hospital of Xi’an Jiao Tong University (Xi’an, China),
and written informed consent was obtained from the husband of the
patient.
Case report
A 47-year-old female presented with a one-year
history of substantial pale and malodorous vaginal discharge,
occasional vaginal contact bleeding and contact pain. The patient
denied all urinary and digestive symptoms. The patient had a
previous MDS history for 8 years and was treated with multiple
blood transfusions and oral retinoids, stanozolol and α-D3.
The Karnofsky performance status (4) score of the patient was 50. On physical
examination, positive findings consisted of anemic appearance. A
gynecological examination showed a cervix that was cauliflower-like
with a diameter of 7 cm, covered with thick pus-moss. The tumor
extended to the pelvic wall and the bilateral parametrial ligaments
became thick and non-elastic. A IIIB stage was determined according
to the International Federation of Gynecology and Obstetrics
classification system (5).
The initial complete blood cell count was as
follows: White blood cell (WBC) count, 0.9×109 cells/l;
red blood cell (RBC) count, 0.78×1012 cells/l;
hemoglobin (HGB), 30 g/l; and platelet (PLT) count,
72×109 cells/l; indicating the failure of bone marrow
hematopoietic function. Laboratory studies revealed normal urine,
feces, blood coagulation and liver and kidney function.
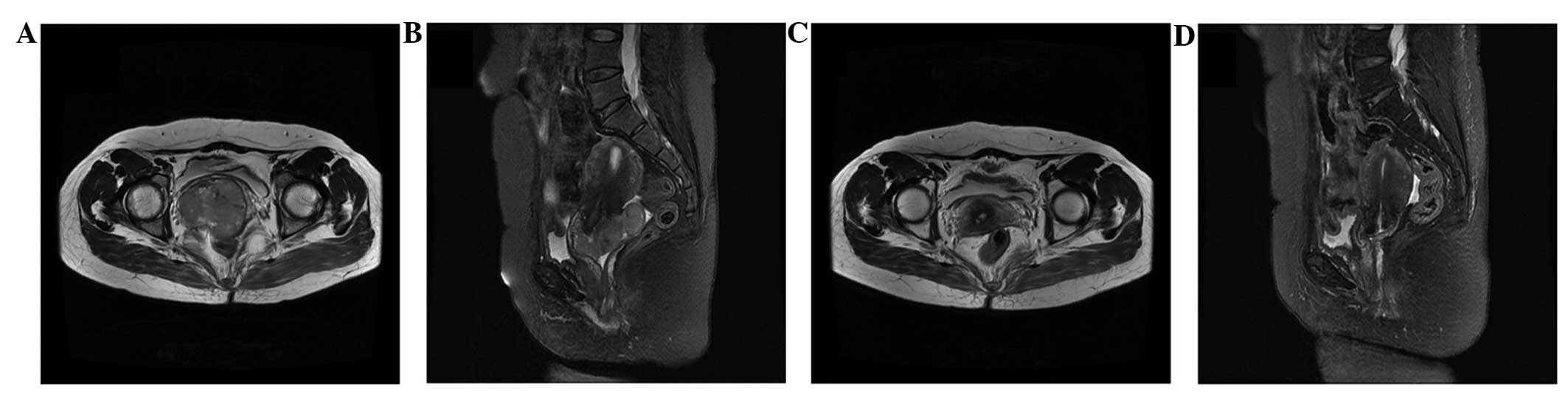
No abnormality was found on the computed tomography
scan of the chest and abdomen. Magnetic resonance imaging (MRI) of
the pelvis (Fig. 1A and B) showed a
soft-tissue mass on the cervix, which invaded the bilateral
parametrial ligaments and extended to the pelvic wall. The imaging
features supported the clinical diagnosis of cervical cancer stage
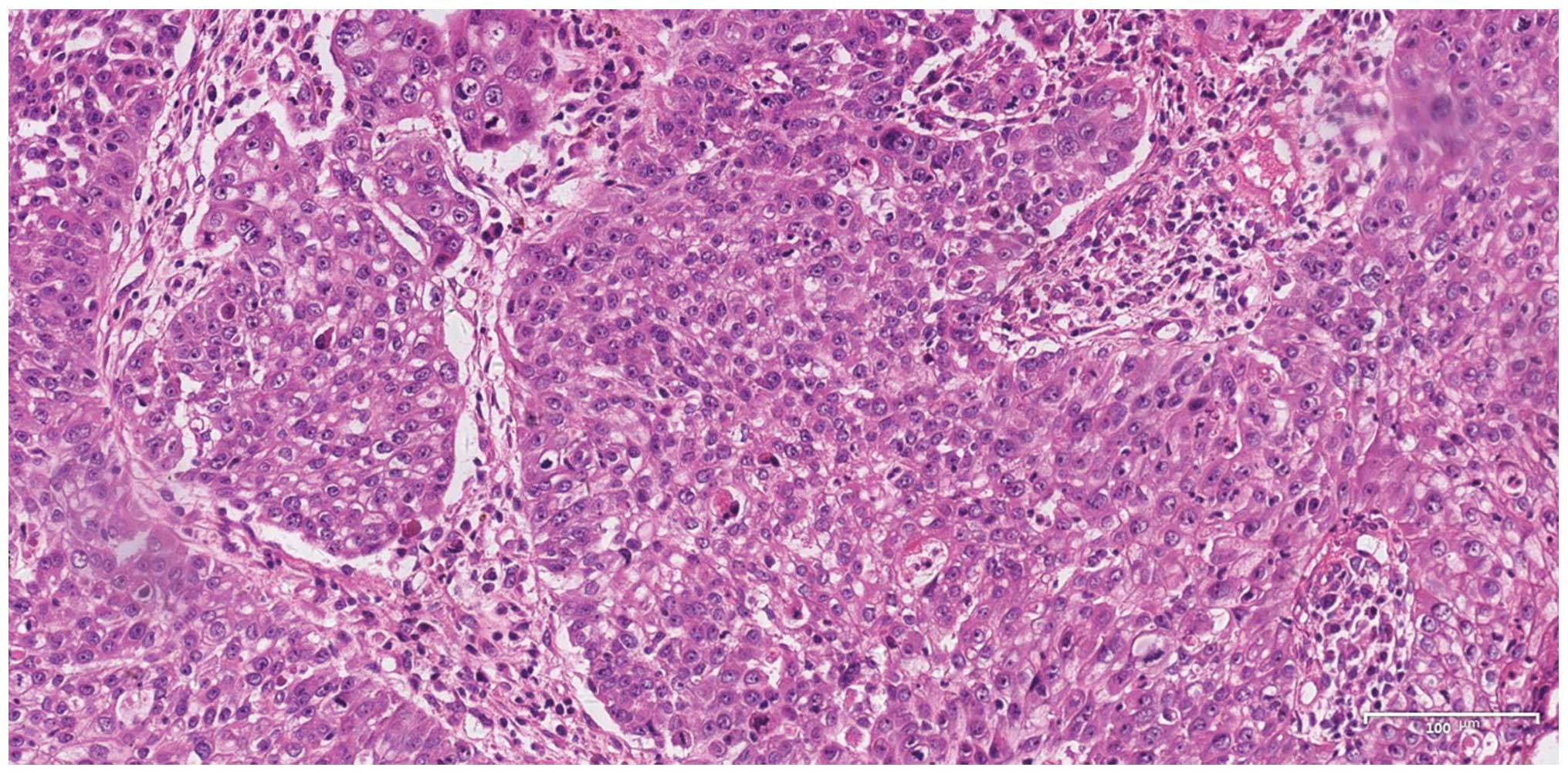
IIIB. A colposcopy cervical biopsy was performed. The histological
analysis revealed a low-grade (grade 3) cervical squamous-cell
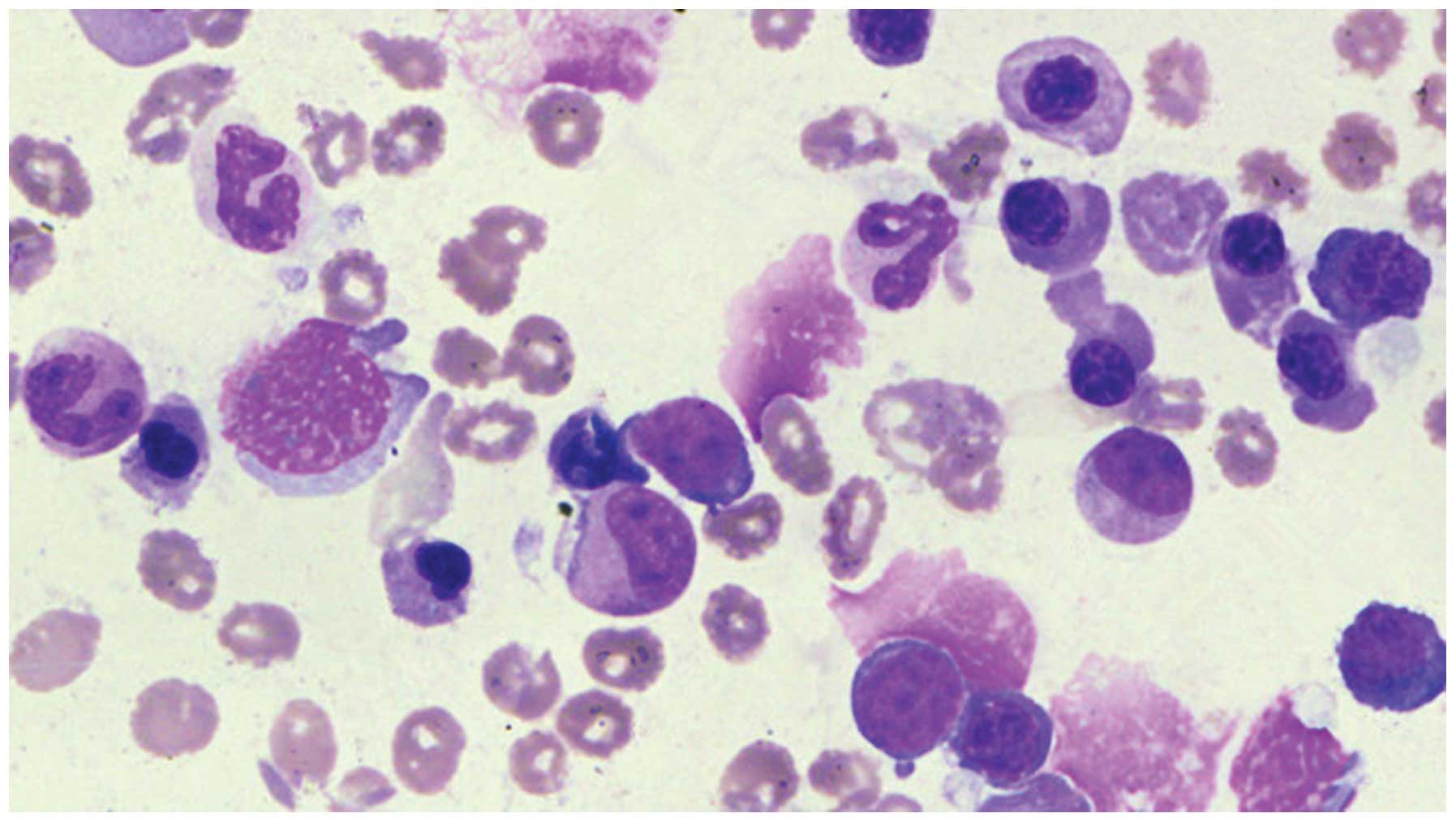
carcinoma (Fig. 2). A bone marrow
aspiration in the ilium showed trilineage dysplasia and an increase
in the original cells (Fig. 3).
A multidisciplinary treatment (MDT) discussion was
conducted and a rigorous treatment plan was created. The peripheral
blood count of the patient was improved. A total of 250 μg of
granulocyte colony-stimulating factor (G-CSF) and 2 mg of
interleukin-11 (IL-11) were subcutaneously injected twice a day to
stimulate granulocyte and megakaryocyte proliferation and
differentiation, respectively. RBC suspensions were transfused to
correct the anemia. Hematopoietic materials, including vitamin B12
and folic acid, were also supplied to correct the anemia. External
body radiation therapy (EBRT) was prescribed to the whole pelvic
region in 25 fractions totaling 50 Gy, followed by intracavitary
brachytherapy. The total dose of brachytherapy prescribed was 20
Gy/4 fractions [equivalent dose of 2 Gy/f (EQD2) = 25 Gy, α/β = 10]
to point A (2 cm above the cervical os marker and 2 cm
perpendicular to the uterine axis along the plane of the uterus).
In order to protect the bone marrow, the EBRT was applied through
intensity-modulated radiation therapy (IMRT) techniques and the
volume of the pelvic bone receiving 20 Gy (V20) was controlled to
<70% (6). Due to a recurrent
III-IV degree myelosuppression, the chemotherapy was not included
in the treatment regimen.
Radiation therapy was started when the WBC count,
PLT count and HGB were ≥4×109 cells/l,
≥50×109 cells/l and ≥50 g/l, respectively. During the
radiotherapy, the patient continued to have injections of G-CSF and
IL-11 along with the intermittent transfusion of the RBC
suspension. However, the patient experienced a IV degree
myelosuppression following 16 Gy/8 fractions of EBRT. The EBRT was
halted and brachytherapy, with a potential to produce weaker bone
marrow suppression, was initiated. Following 20 Gy/4f of
brachytherapy (EQD2 = 25 Gy, α/β = 10), the EBRT was continued.
Subsequently, the amount of EBRT was pushed to 26 Gy/13 fractions.
However, the WBC count, PLT count and HGB decreased to
0.35×109 cells/l, 17×109 cells/l and 29 g/l,
respectively. The radiotherapy was withheld due to the recurrent IV
degree myelosuppression and the failure of supportive care for the
bone marrow hematopoietic function. Therefore, the total dose of
point A was 51 Gy (EQD2, α/β = 10). The patient was then discharged
from the hospital, as no further treatment was accepted. One month
later, a gynecological examination and pelvic MRI (Fig. 1C and D) revealed the treatment
effect was complete remission (CR) (7).
Seven months later, however, lung and liver
metastasis occurred. The patient succumbed to an acute intracranial
hemorrhage due to thrombocytopenia (PLT count, 9×109
cells/l) 13 months after radiotherapy.
Discussion
According to the National Comprehensive Cancer
Network guidelines (8) for cervical
cancer, the standard therapeutic schedule of a IIIB stage cervical
cancer was concurrent chemoradiotherapy. However, the disease
management should always be tailored according to the circumstances
of the individual patient. For the present patient, a long-term
bone marrow suppression caused by the MDS already existed, which
excluded the standard chemoradiotherapy as a feasible choice.
Following an MDT discussion, a plan of palliative radiotherapy was
agreed upon. In order to protect the hematopoietic function of the
bone marrow, the IMRT technique was applied to minimize the
receiving dose of the pelvic bone marrow. A study by Rose et
al (6) demonstrated that the
hematological toxicity increased with an increasing pelvic bone
marrow irradiation volume. Therefore, efforts should be made to
maintain a V20 of >76%, which may reduce the hematological
toxicity (6). For the present
patient, the V20 was controlled to stay >70% to minimize the
receiving dose of the pelvic bone marrow. Nevertheless, recurrent
attacks of IV degree myelosuppression eventually led to the
termination of radiotherapy. However, the treatment effect still
achieved CR.
Using methods to control cancer (such as
chemotherapy and radiotherapy) is likely to cause bone marrow
damage, resulting in blood disease and a poor prognosis. However,
the patient in the present case would have had a poor prognosis if
the cancer was ignored. On the premise of elevating blood count and
protecting the bone marrow, the patient in the present study
accepted reduced-dose radiotherapy without chemotherapy. Finally,
the total dose accepted by point A was 51 Gy. The treatment effect
achieved CR. Therefore, for these patients to achieve the optimal
therapeutic effect and the longest survival time, the dose of
radiotherapy should be appropriately reduced on the premise of
elevating blood count and protecting the bone marrow.
Anemia has a negative impact on local control,
disease-free survival and overall survival rate of cervical cancer
(9,10). In the present study, anemia caused
by MDS persisted during the radiotherapy, which was a significant
factor for progression-free survival (PFS). Insufficient radiation
and chemotherapy, and low immunity caused by the long-term MDS were
also involved in the poor prognosis of the cervical cancer. By
contrast, the bone marrow cell loss induced by radiation was a poor
prognostic factor for the MDS. Overall, the interaction between the
two diseases eventually led to a shorter PFS and eventually a
fatality due to intracranial bleeding.
References
|
1
|
Misgeld E, Germing U, Aul C and Gattermann
N: Secondary myelodysplastic syndrome after fludarabine therapy of
a low-grade non-Hodgkin’s lymphoma. Leuk Res. 25:95–98. 2001.
|
|
2
|
Kondo H and Shinbo I: Myelodysplastic
syndrome associated with gastric cancer and colon polyp. Rinsho
Ketsueki. 38:1234–1237. 1997.(In Japanese).
|
|
3
|
Takahashi T, Kazama Y, Shimizu H, et al:
Myelodysplastic syndrome progresses rapidly into erythroleukemia
associated with synchronous double cancers of the stomach and the
papilla of Vater. Int J Hematol. 74:64–69. 2001.
|
|
4
|
Schaafsma J and Osoba D: The Karnofsky
Performance Status Scale re-examined: a cross-validation with the
EORTC-C30. Qual Life Res. 3:413–424. 1994.
|
|
5
|
Pecorelli S: Revised FIGO staging for
carcinoma of the vulva, cervix, and endometrium. Int J Gynaecol
Obstet. 105:103–104. 2009.
|
|
6
|
Rose BS, Aydogan B, Liang Y, et al: Normal
tissue complication probability modeling of acute hematologic
toxicity in cervical cancer patients treated with
chemoradiotherapy. Int J Radiat Oncol Biol Phys. 79:800–807.
2011.
|
|
7
|
Eisenhauer EA, Therasse P, Bogaerts J, et
al: New response evaluation criteria in solid tumors: revised
RECIST guideline (version 1.1). Eur J Cancer. 45:228–247. 2009.
|
|
8
|
National Comprehensive Cancer Network.
Practice Guidelines in Oncology. http://www.nccn.org/professionals/physician_gls/f_guidelines.asp.
Accessed May 30, 2013
|
|
9
|
Grogan M, Thomas GM, Melamed I, et al: The
importance of hemoglobin levels during radiotherapy for carcinoma
of the cervix. Cancer. 86:1528–1536. 1999.
|
|
10
|
Haensgen G, Krause U, Becker A, et al:
Tumor hypoxia, p53, and prognosis in cervical cancers. Int J Radiat
Oncol Biol Phys. 50:865–872. 2001.
|