Introduction
Meningioma is the most common type of benign
intracranial tumor and accounts for 20–25% of all central nervous
system neoplasms. Meningioma usually grows slowly and is frequently
found to compress the adjacent anatomical structures, which
subsequently leads to the onset of neurological symptoms and signs.
Skull hyperostosis is a well-known sign of meningioma and is
observed in 4.5% of all types (1).
Although bone invasion and hyperostosis are common phenomena in
patients with intracranial meningiomas, the basic pathomechanism is
not fully understood and tumor invasion appears to be generally
accepted. The current study presents a rare case of giant bilateral
calvarial hyperostosis across the superior sagittal sinus,
secondary to brain meningioma in a 43-year-old female. The patient
successfully underwent embolization of the tumor-supplying vessels,
total resection of the giant calvarial hyperostosis and
intracranial tumor and skull cranioplasty in one surgical
procedure. However, the management of such a case presents a
surgical challenge. The patient provided written informed
consent.
Case report
In July 2011, a 43-year-old female was admitted to
the Department of Neurosurgery, Clinical Medical College, Yangzhou
University (Yangzhou, China) due to the progressive enlargement of
a left frontoparietal mass for >30 years, with recurrent
headache and hyperspasmia. The patient underwent skull tumor
resection 30 years ago and the postoperative pathological diagnosis
was skull hyperostosis. Following this surgery, uplift of the left
frontoparietal region began gradually, which was accompanied by
clinical headache and progressive enlargement of the lesion in the
past two years. In addition, one week prior to admission, the
patient experienced one episode of grand mal epilepsy which lasted
for 15 min.
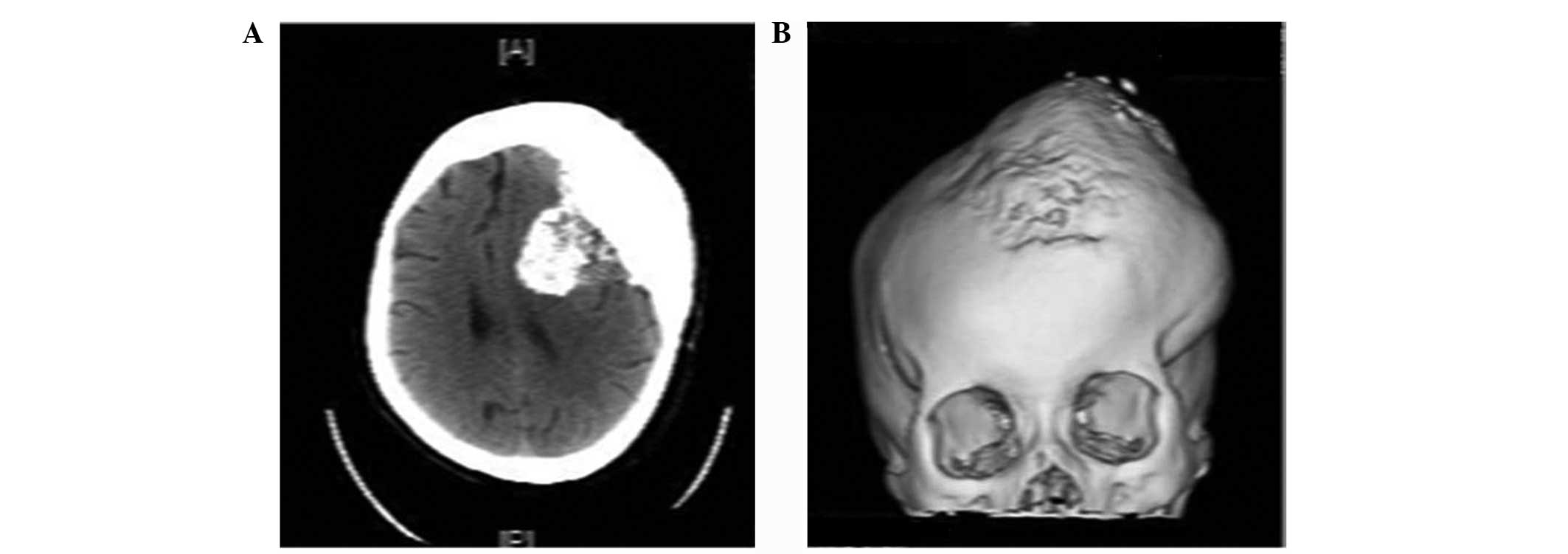
The palpable fixed subcutaneous mass was 16×15×5 cm
in size, with a hard texture, an unclear boundary and an uneven
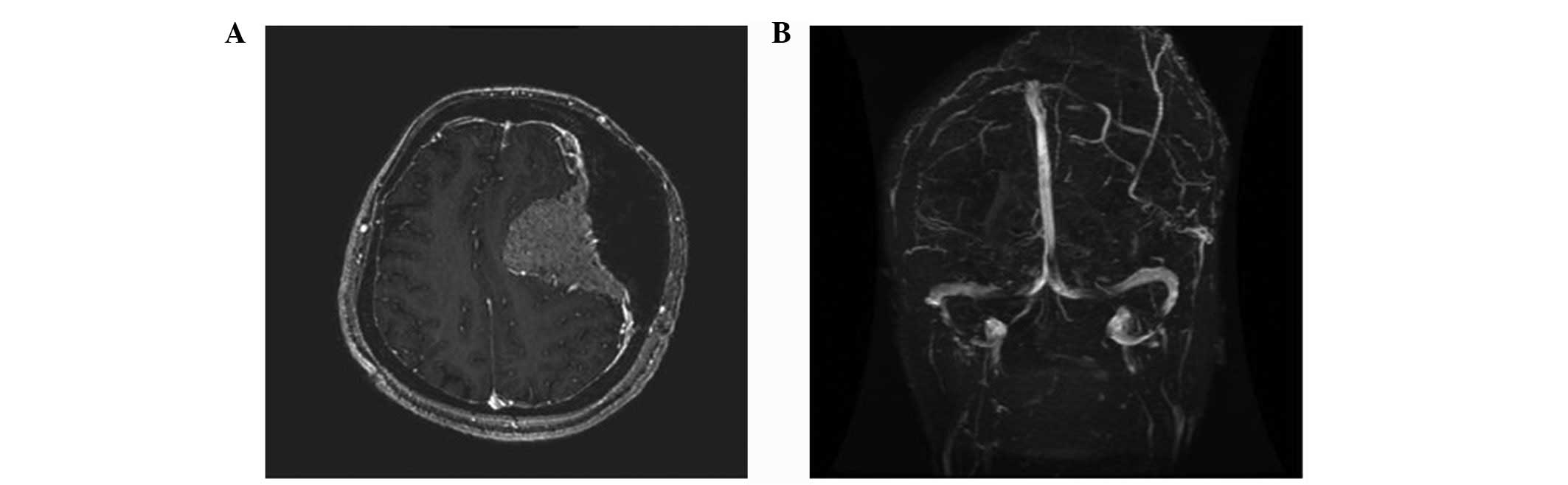
surface. The diagnoses of huge skull hyperplasia and meningioma
were determined by computed tomography and magnetic resonance
imaging examination (Figs. 1 and
2). In addition, digital
subtraction angiography demonstrated that the left middle meningeal
artery and branches of the left superficial temporal artery were
the major sources of blood supply to the tumor, with little
involvement of the right middle meningeal artery and branches of
the right superficial temporal artery. Following embolization of
the aforementioned arteries, the patient immediately underwent
total resection of the giant calvarial hyperostosis and
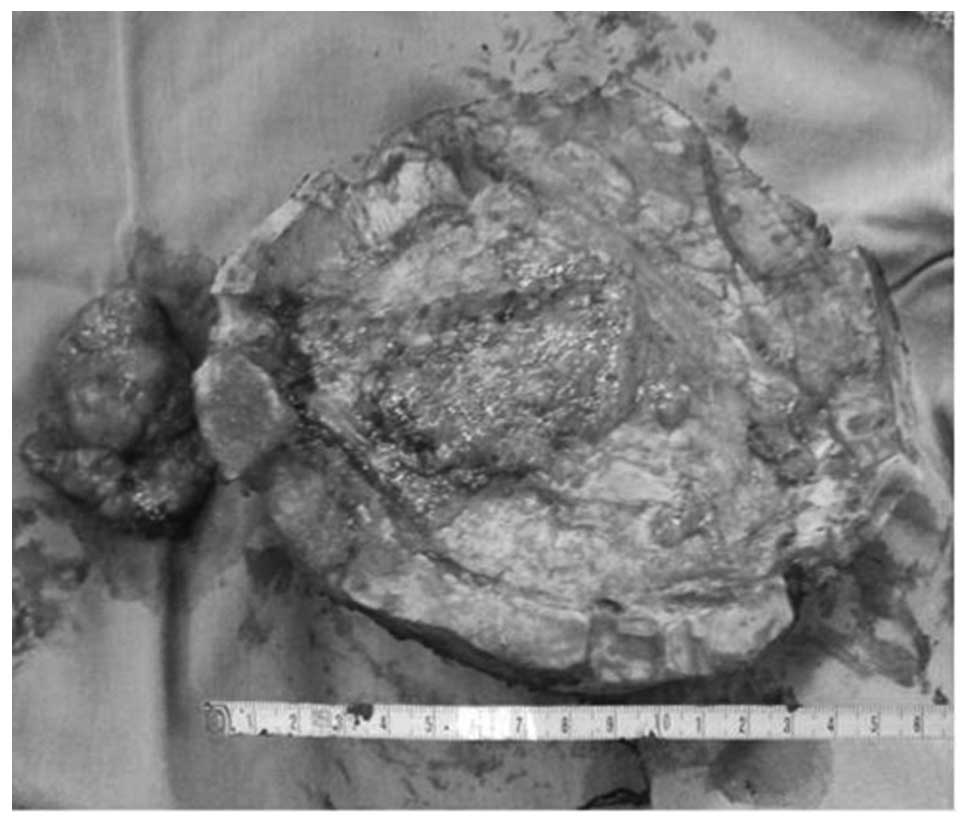
intracranial tumor, and skull cranioplasty. The tumor was removed
by bilateral frontoparietal craniotomy and, during surgery, the
abnormal mass, measuring 14×12×3–5 cm, exhibited a hard and uneven
surface extending 3 cm from the bone surface. Based on the surgical
observations, total resection of the hyperplastic skull was
performed at a distance of 1 cm from the parietal eminence. The
surgeons also observed that the neoplasm had invaded and destroyed
the inner table of the compact bone flaps without diploe. The mass
below the dura was 8×6×3 cm in size, with a soft texture and
abundant blood supply. Although incomplete capsular invasion of the
superior sagittal sinus was observed, the neoplasm was
well-circumscribed by the cortex (Fig.
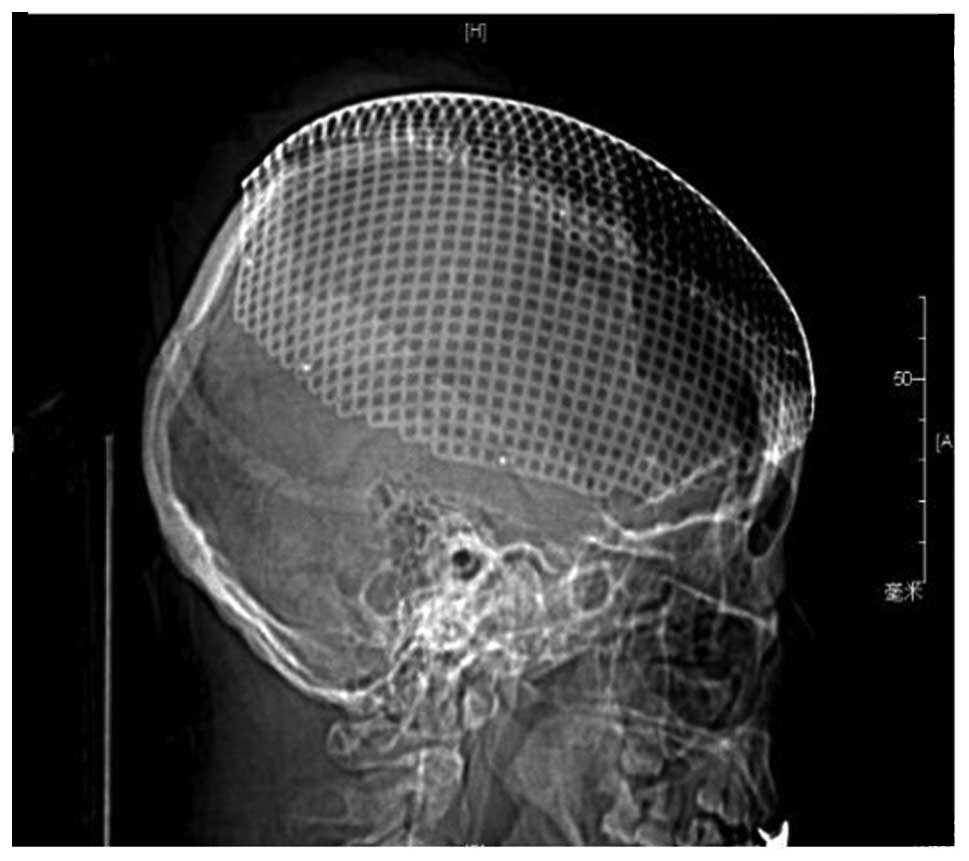
3). Following complete enucleation of the skull lesion and
tumor, a cranioplasty was performed with titanium mesh (Fig. 4).
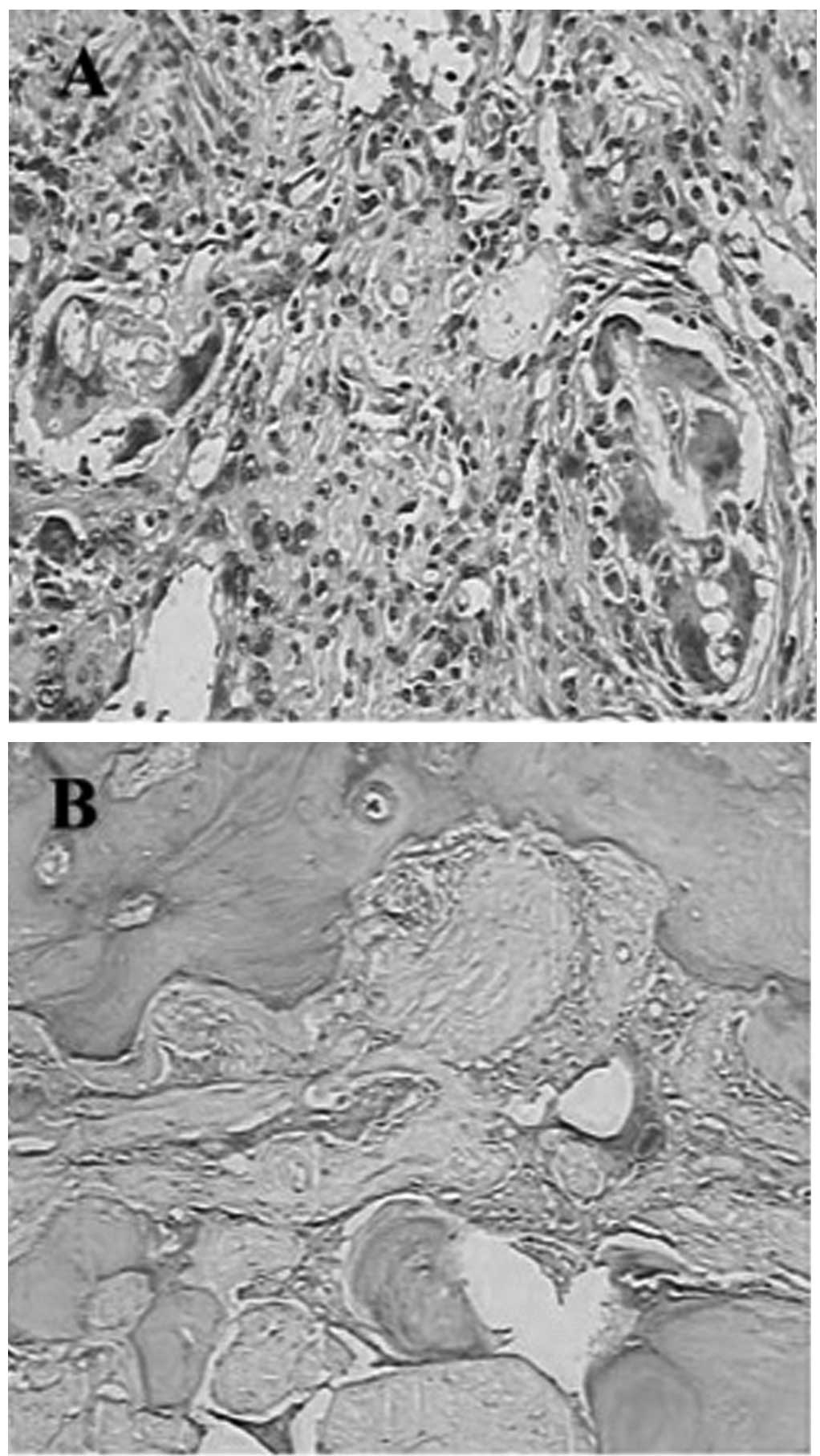
The surgical specimen was routinely fixed with 10%
formalin and paraffin-embedded, prior to staining with hematoxylin
and eosin (magnification, 10×10). Histologically, the intracranial
tumor was composed of a large number of meningothelial meningioma
cells [World Health Organization (WHO) grade I] in the majority of
areas and a few tumor cells exhibited severe atypism (anaplastic
meningioma; WHO grade III). The external section of the tumor that
involved the full thickness of the calvarial bone superiorly
extended to the extracranial soft tissue. Furthermore, the
gray-white tissue observed in the inner side of the examined
calvarial bone was resected and measured 15×14×7 cm in size.
Microscopically, the hyperostotic bone contained some meningioma
tissue (Fig. 5) and the
postoperative pathological diagnosis was determined as left
frontotemporal meningioma accompanying calvarial bone hyperostosis.
The patient was followed up for more than two years and showed no
evidence of tumor recurrence.
Discussion
The cause of associated hyperostosis in meningioma
remains a point of controversy, specifically in terms of whether it
presents a secondary change of the bone without tumor invasion
versus direct infiltration of the bone by tumor. However, tumor
invasion of the bone appears to be generally accepted, as a number
of cases with hyperostosis have revealed histological tumor cell
infiltration of the bone (2,3). In
the present case, the tumor cells were histologically found to
infiltrate from the full thickness of the skull bone to the
subcutaneous tissue, which confirms the theory of tumor invasion of
the bone.
However, in this case, a number of factors remain
unknown, which may imply that a number of factors or an alternative
pathogenesis are the cause of associated hyperostosis in
meningioma. The unknown factors are as follows: The manner in which
the patient’s bone hyperplasia, pathologically confirmed 30 years
ago, has recurred as intracranial meningioma; whether the formation
of the meningioma was caused by stimulation of the bone hyperplasia
to the meningeal; or the cause of a relatively small growth of the
recurrent meningioma over 30 years. Bony hyperostosis is a common
sign of meningioma, in which the hyperostotic bone is usually
smaller than that of the underlying tumor. However, in the present
case, the sizes of hyperostotic bone and the underlying tumor were
14×12 and 8×6 cm, respectively, which contradicts the
hyperostosis-associated tumor invasion theory. The following
hypotheses concerning the mechanism of hyperostosis associated with
meningioma may provide answers to the above questions: Preceding
trauma; vascular disturbances of the bone caused by the tumor;
irritation of the bone by the tumor without invasion; stimulation
of osteoblast cells in the normal bone via humoral factors secreted
by tumor cells; and formation of bone by the tumor itself (4). Furthermore, Pei et al (5) reported that the increased expression
of matrix metalloproteinases (MMP)-13 and membrane-type-1-MMP in
the tumor region of the hyperostosis of meningioma may contribute
to the initiation of osteolysis. In addition, activated MMP-2 in
hyperostotic lesions may change the physiological metabolism of the
skull bone and, thus, be important for the formation of
hyperostosis.
Marwah et al (6) termed meningioma occurring in the skull
as primary intraosseous meningioma and the diagnostic criteria
include the following conditions: i) Having the histological
features of meningioma; ii) lesions located in the epidural or
skull; and iii) no involvement of the brain tissue, arachnoid and
dura. In the present case, pathological examination of the skull
bone showed that the tumor cells had invaded all layers of the
skull bone up to the subcutaneous tissue. Surgery confirmed the
tumor to be located in the subdural space with invasion of the
superior sagittal sinus, which does not meet the diagnostic
criteria of the intraosseous meningiomas.
The wide extent of the tumor (bilateral extensive
calvarial hyperostosis with invasion of the superior sagittal sinus
and associated diffuse bilateral en plaque growth with compression
of the underlying brain on the two sides) posed a formidable
surgical challenge. In order to reduce bleeding during resection,
it is necessary to embolize the major arteries supplying blood to
the tumor, including the left middle meningeal artery and branches
of the left superficial temporal artery. In addition, wherever
possible, resection of the entire involved bone is recommended to
prevent recurrence. In the present study, the bilateral
frontoparietal flaps were extremely thick bone and, therefore, the
removal of the flaps would have left a huge bilateral cranial
defect involving the frontoparietal regions which may have required
a significant and difficult reconstruction. An additional
difficulty of the procedure is that following the removal of the
bone flaps and subsequent exposure of the superior sagittal sinus,
there is a risk of superior sagittal rupture, which often results
in a significant amount of bleeding, even when no tearing of the
superior sagittal sinus has occurred. Therefore, a large number of
gelatin sponges are often required to achieve a significant
hemostasis effect. Goel et al (7) also reported a case of extracranial
extension of a meningioma, whose loss of blood exceeded 2.5 liters
during the surgery. Additionally, in the postoperative phase, the
patient developed disseminated intravascular coagulation disorder
and suffered bleeding at multiple sites, including the surgical
area, and subsequently succumbed to the disease within 8 h of the
surgery. In the present case, the key to success was embolization
of the major arteries supplying blood to the tumor and the
tenacious protection of the superior sagittal sinus during
surgery.
References
|
1
|
Gupta SK, Mohindra S, Radotra BD and
Khosla VK: Giant calvarial hyperostosis with biparasagittal en
plague meningioma. Neurol India. 54:210–212. 2006.
|
|
2
|
Yilmaz A, Müslüman AM, Cavuşoğlu H, et al:
Meningioma causing hyperostosis of the cranial convexity in a
child. J Clin Neurosci. 17:926–929. 2010.
|
|
3
|
Min JH, Kang SH, Lee JB, et al:
Hyperostosis meningioma with minimal tumor invasion into the skull.
Neurol Med Chir (Tokyo). 45:480–483. 2005.
|
|
4
|
Pieper DR, Al-Mefty O, Hanada Y and
Buechner D: Hyperostosis associated with meningioma of the cranial
base: secondary changes or tumor invasion. Neurosurgery.
44:742–746. 2005.
|
|
5
|
Pei J, Jung S, Jin SG, et al: Possible
role of matrix metalloproteinases (MMPs) in hyperostosis of
intracranial meningiomas. Acta Neurochir (Wein). 154:611–620.
2012.
|
|
6
|
Marwah N, Gupta S, Marwah S, et al:
Primary intraosseous meningioma. Indian J Pathol Microbiol.
51:51–52. 2008.
|
|
7
|
Goel A, Mehta A and Gupta S: Unusual mode
of spread and presentation of meningioma: a case report. Neurol
India. 47:311–313. 1999.
|