Introduction
Male breast cancer (MBC) is a rare and special type
of breast cancer, which is rarely observed in clinical practice.
The incidence of MBC is ~1% among all breast cancer patients
(1), however, recent studies in the
USA have shown that the incidence of MBC is on the rise (2). Since MBC is rarely observed in
clinical practic, few prospective and randomized clinical studies
have analyzed the disease. In addition, due to the rarity of MBC,
patients and physicians are less suspicious of the disease, which
therefore, delays diagnosis to a great extent and leads to the
development of illness. Furthermore, the prognosis of such a
condition has not been significantly improved over the past 25
years (3). MBC with an unknown
primary lesion is even rarer and presents a special type of breast
cancer of which the initial symptom is axillary lymphatic
metastasis. However, the primary lesion within the breast can not
be detected during physical examination and imaging examination.
MBC was first described Halsted (4)
in 1907. The main treatment for MBC is extended resection of the
suspicious breast lesions in combination with axillary lymph node
dissection, which attack the root causes of the disease and improve
patients quality of life. In addition, the adjuvant chemotherapy
regimen is likely to be administered according to the standard used
for female breast cancer (5). MBC
with an unknown primary tumor is rare and therefore prone to
misdiagnosis, which results in treatment delay. Such cases are
extremely significant for clinical reference and the current study
presents a case of a clinically misdiagnosed MBC with an unknown
primary tumor.
Case report
The current study presents the case of a 58-year-old
male who developed a painless mass in the left armpit in May 2009.
The mass was hard and 0.8×0.6 cm in size. There was no obvious
discomfort and the mass was treated with drugs, including
amoxicillin capsules (500 mg, every 8 h for five days). In May
2011, the mass had become significantly larger and was accompanied
by pain. The patient received anti-infection treatment with
ceftriaxone sodium at the Fujian Union Hospital (Fuzhou, China) and
an armpit mass biopsy was obtained. The pathological examination
showed glandular cancer with a high possibility of a mammary
primary tumor. For further anticancer treatment, the patient was
moved to the larger and specialized Fujian Cancer Hospital (Fuzhou,
China), where a metastatic poorly-differentiated cancer was
considered following the pathology consultation, and the primary
tumor was unknown. It was recommended that the patient should have
a positron emission tomography/computed tomography (PET-CT) general
physical check-up, however, the primary tumor remained unknown. The
final diagnosis was of secondary lymph node cancer, with an unknown
primary tumor. The patient was empirically administered four cycles
of paclitaxel (200 mg) plus oxaliplatin (120 mg) chemotherapy
between June and October 2011 and subsequently the symptom was
eased. The curative effect was evaluated as a partial response, and
the patient was later discharged.
Three months after discharge, the patient found new
disseminated lymph nodes in the left armpit. On January 9, 2012,
the patient came to Fuzhou General Hospital of Nanjing Military
Command (Fuzhou, Fujian, China) and the admission examination
showed that changes to the mass in the left armpit were visible.
Several enlarged lymph nodes, ~1.2×0.5 cm in size, were palpable,
hard and fixed in position, with a complete surface. Pain was felt
upon the application of light pressure. The superficial lymph nodes
were not enlarged and the heart, lungs and abdomen showed no
obvious abnormalities. A PET-CT examination was also carried out
and the results revealed that higher metabolism occurred in the
lymph nodes in the left armpit. The malignant tumor, along with
tumor activity, was considered, and again the diagnosis was of
secondary lymph node cancer, with an unknown primary tumor. Between
March 26 and May 26, 2012, the patient was administered docetaxel
(100 mg) plus lobaplatin (80 mg) chemotherapy. The chemotherapy
continued smoothly and no obvious adverse reactions occurred.
Following three cycles of chemotherapy, the curative effect was
evaluated as progressive disease. On June 9, 2012, the patient
returned for treatment again. The disease had not been effectively
controlled by the two chemotherapy schemes (200 mg paclitaxel plus
120mg oxaliplatin) and therefore, a repeat analysis was performed
in terms of the patient’s condition. As the patient’s response to
chemotherapy was poor, the final consideration was that the
condition had not been diagnostically determined subsequent to the
multidisciplinary consultation.
Pathological examination is the most reliable
diagnostic method (5), therefore,
it was recommended that the patient return to the Fujian Union
Hospital in order to have the initial pathological section and
paraffin blocks sent to Fuzhou General Hospital of Nanjing Military
Command for the pathology consultation. The results indicated a
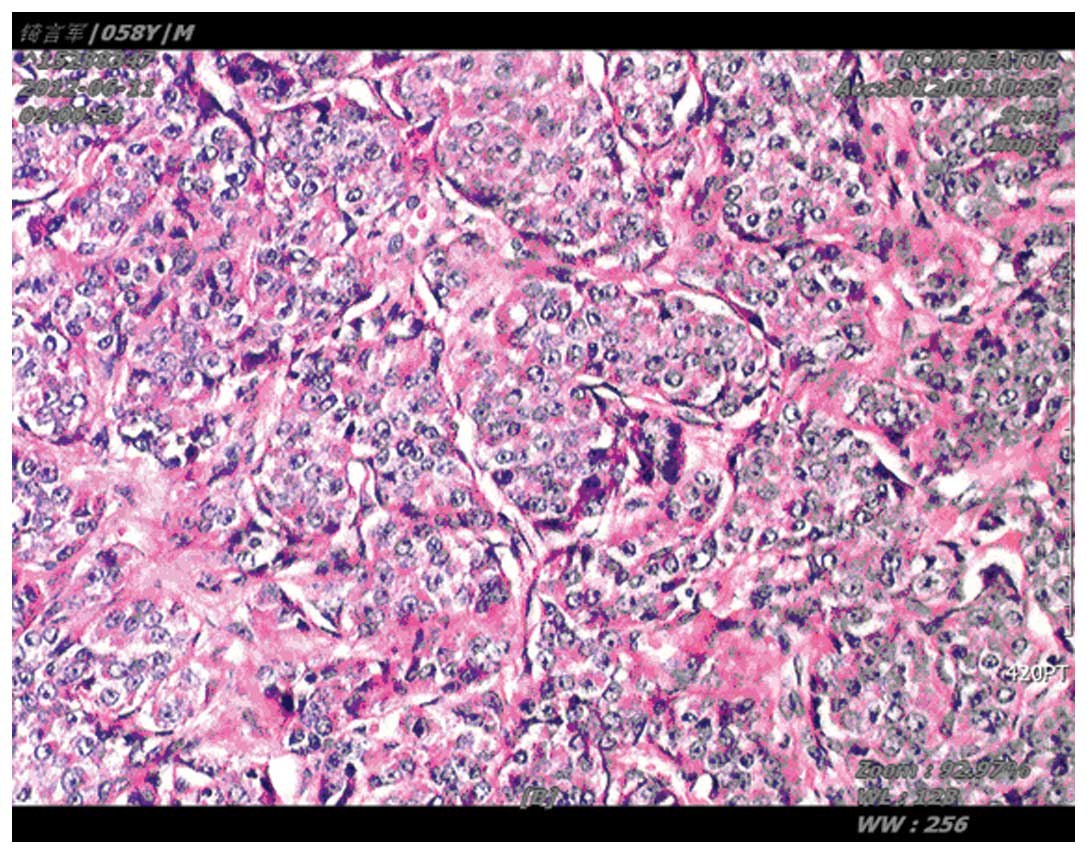
poorly-differentiated cancer. Immunohistochemistry analysis of the
biopsy revealed the following: Staining for epithelial membrane
antigen, E-cadherin, P120, cytokeratin (CK) pan and the estrogen
and progesterone receptors was strong (+++), with 90 and 85%
positive staining for ER and PR, respectively, while CK7 was weak
(+). A Ki-67 of 5% was detected. Thus, immunohistochemistry results
of the biopsy specimens of the mass in the left armpit revealed a
class I breast invasive ductal carcinoma (Fig. 1).
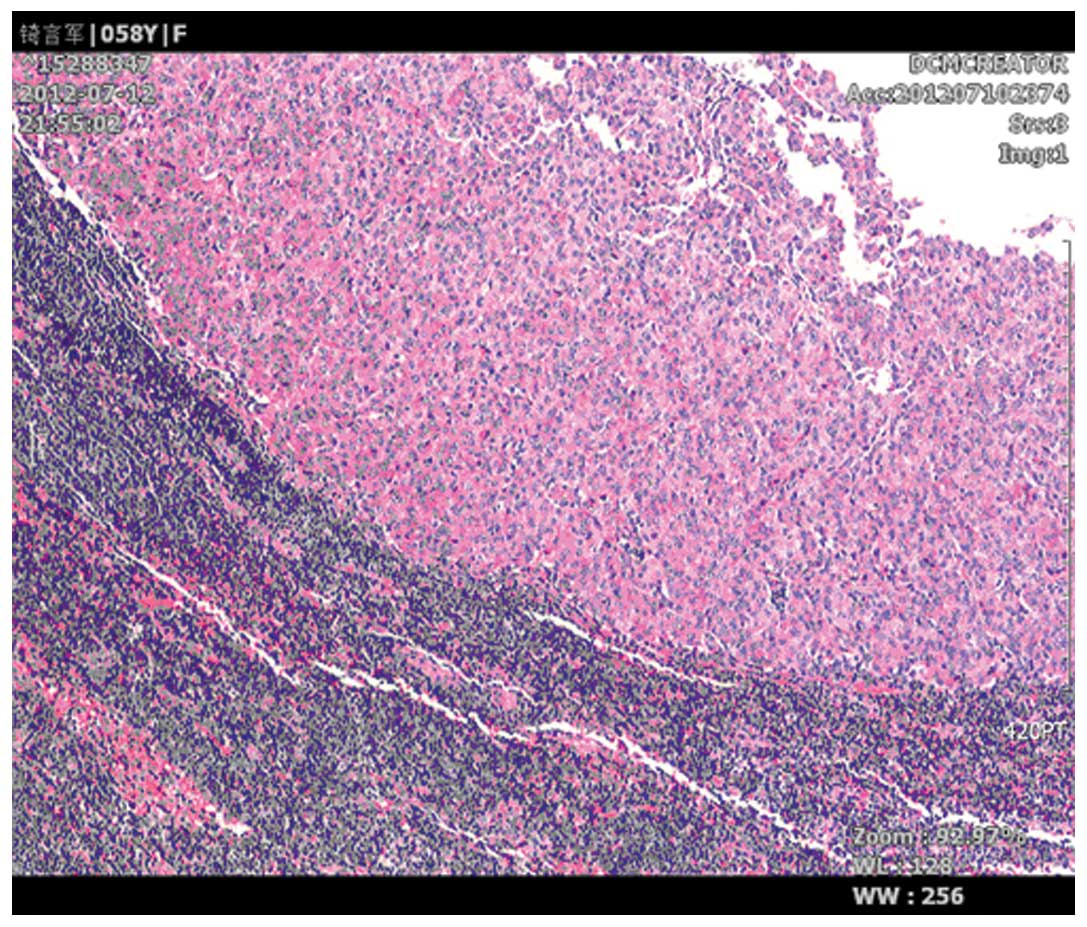
The initial diagnosis at the Fujian Union Hospital
was correct. Following the determination of the diagnosis as breast
cancer with lymph node metastasis, a treatment scheme was proposed.
The patient received a left breast cancer modified radical
mastectomy in Fuzhou General Hospital of Nanjing Military Command
on July 10, 2012. During the surgery, one 10×5×3-cm specimen was
resected. According to the pathological examination following the
surgery, neither cancer tissue residues nor cancer involving the
nipple, skin, breast, basal or skin resection margin were found. No
cancer tissue residues were found in the post-operative radical
cure specimen of the breast invasive ductal carcinoma. (Fig. 2). The cancer metastasis to the lymph
nodes in the armpit was detected. Subsequent to repeated
communication concerning the disease, the patient returned to the
hospital in September 2012 and received two cycles of doxorubicin
hydrochloride (80 mg every three weeks) single-agent post-operative
adjuvant chemotherapy and one course of radiotherapy (60 Gy in 30
fractions of 2 Gy per fraction of five fractions per week).
According to the follow-ups performed between December 2012 and
March 2013, the patient has been able to conduct normal activities,
with a markedly improved quality of life, and no further
abnormalities have been found.
Discussion
The cause of MBC is unclear, however, the main risk
factors include an increase in the level of estrogen, Klinefelter
syndrome along with chromosomal abnormality and gynecomastia
(6). The typical clinical
manifestation of MBC is a surrounding painless mass, the occurrence
rate of which is 75–95% (7). MBC
has its own characteristics with regard to onset, risk factors and
clinical manifestations, often leading to a delay in the diagnosis
and treatment.
No breast mass was found in the physical examination
of the patient in the current case. The tumor markers, cancer
antigen-125 and carcinoembryonic antigen, were normal. No primary
tumors were observed in the mammography and PET-CT, and the patient
was diagnosed with breast invasive ductal carcinoma based on the
metastases pathology and the immunohistochemical examination, while
the primary tumor could not be found following the left breast
modified radical mastectomy. However, primary tumors may disappear
subsequent to chemotherapy.
The symptoms of MBC are similar to those experiences
by females with breast cancer following the menopause. However, the
lack of awareness of MBC may delay the diagnosis and treatment,
which is likely to result in the progression of the illness. In
addition, the majority of cases present with axillary lymph node
metastases at diagnosis and are at a late clinical stage. A
previous study showed that, according to statistics in 1955, the
symptoms prior to diagnosis can be maintained for an average of 21
months (8), while other more recent
studies have confirmed that the average delay period for the
diagnosis of MBC is between six and 10 months (9). In addition, >40% of MBC are already
at phase III/IV at diagnosis (10).
Since male breast tissue does not grow, differentiation into a
lobule structure is rare, unless the endogenous or exogenous
estrogen concentration increases. Therefore, the vast majority of
histological MBC types are invasive ductal carcinoma, accounting
for >90% of all MBC (2). Due to
the late diagnosis and spread of the tumor, the prognosis of MBC is
generally worse than that of females with breast cancer. Therefore,
the early detection, diagnosis and treatment are key factors for
improving the prognosis of MBC. The present study demonstrated that
in addition to methods such as clinical features, imaging
observations and tumor marker examination, the collection of data
through fine-needle aspiration and lumpectomy biopsy in clinical
practice are required for evaluation.
Through the diagnosis and treatment of the patient
in the present case, the following were confirmed: i) MBC has a low
morbidity, often shows clinical manifestations or pathological
characteristics that are different compared with common breast
cancer, and the primary tumor may be unknown. Therefore a proper
analysis should be conducted, with more attention given to such
conditions. ii) The pathological report and immunohistochemistry
results are extremely important for guiding the diagnosis of
malignant tumors. Therefore, imaging diagnostics, such as PET-CT,
should not be solely depended on. If the treatment is not effective
then the initial diagnosis should be questioned, unless the
diagnostic results are absolutely clear. Clinicians should be aware
that pathology reports and clinical manifestations should be
consistent. iii) Currently, there remains a lack of prospective
randomized controlled clinical trial research with regard to MBC
treatment. The MBC treatment scheme may also be developed by
referencing the experience of female breast cancer treatment, and
clinicians should use sufficient medical evidence to prove the
scientific rationality of the MBC diagnosis and treatment
scheme.
The current study described an extremely rare case
of MBC with an unknown primary tumor and highlights a method of the
diagnosis and treatment of MBC.
References
|
1
|
Jemal A, Siegel R, Ward E, Murray T, Xu J
and Thun MJ: Cancer statistics, 2007. CA Cancer J Clin. 57:43–66.
2007.
|
|
2
|
Giordano SH, Cohen DS, Buzdar AU, Perkins
G and Hortobagyi GN: Breast carcinoma in men: a population-based
study. Cancer. 101:51–57. 2004.
|
|
3
|
O’Malley CD, Prehn AW, Shema SJ and Glaser
SL: Racial/ethnic differences in survival rates in a
population-based series of men with breast carcinoma. Cancer.
94:2836–2843. 2002.
|
|
4
|
Halsted WS: I. The results of radical
operations for the cure of carcinoma of the breast. Ann Surg.
46:1–19. 1907.
|
|
5
|
Fentiman IS, Fourquet A and Hortobagyi GN:
Male breast cancer. Lancet. 367:595–604. 2006.
|
|
6
|
Nahleh ZA, Srikantiah R, Safa M, Jazieh
AR, Muhleman A and Komrokji R: Male breast cancer in the veterans
affairs population: a comparative analysis. Cancer. 109:1471–1477.
2007.
|
|
7
|
Gennari R, Curigliano G, Jereczek-Fossa
BA, Zurrida S, Renne G, Intra M, Galimberti V, Luini A, Orecchia R,
Viale G, et al: Male breast cancer: a special therapeutic problem.
Anything new? (Review). Int J Oncol. 24:663–670. 2004.
|
|
8
|
Cutuli B: Strategies in treating male
breast cancer. Expert Opin Pharmacother. 8:193–202. 2007.
|
|
9
|
Avisar E, McParland E, Dicostanzo D and
Axelrod D: Prognostic factors in node-negative male breast cancer.
Clin Breast Cancer. 7:331–335. 2006.
|
|
10
|
Agrawal A, Ayantunde AA, Rampaul R and
Robertson JF: Male breast cancer: a review of clinical management.
Breast Cancer Res Treat. 103:11–21. 2007.
|