Introduction
Skin metastasis and tumor lysis syndrome (TLS)
represent independent prognostic factors of poor survival in
patients with malignant tumors. A typical cutaneous metastasis is
in the form of a firm, painless papule or nodule and is a sign of
underlying malignancy in 0.6–7.6% of cases (1–3).
Additional clinical presentations include sclerodermoid, vascular,
alopecic and erysipelas-like lesions (1). Delaying the progression of the
disease, controlling the symptoms and maintaining a high quality of
life for the patient are key to the successful treatment of the
disease (4). TLS, characterized by
severe hyperuricemia, hyperphosphatemia, hyperkalemia and
hypocalcemia, is an oncological emergency due to massive tumoral
cell lysis that usually presents following the initiation of
chemotherapy, and only in extremely rare occasions develops in a
spontaneous manner (5). However,
the precise incidence of TLS is undefined and the standard therapy
strategy for the treatment of TLS is based on volume expansion,
decreasing metabolic abnormalities, and in the majority of cases,
providing supportive treatment for renal failure (6,7).
There have been a few cases of spontaneous TLS
described in the literature, however, there have been no reported
cases of spontaneous TLS combined with multiple subcutaneous
metastases. The present study reports a case of cutaneous
metastatic adenocarcinoma with TLS that showed extremely rapid
progression. The patient suffered from life-threatening
complications, including TLS, liver failure and acute oliguria
renal failure during the supportive treatment. Patient provided
written informed consent.
Case report
A 71-year-old female was admitted to the First
Affiliated Hospital of Liaoning Medical University (Jinzhou, China)
with multiple, red-colored, firm, non-tender subcutaneous nodules
(0.5–6 cm in diameter) over the anterior chest wall, back, arms,
inguinal region, neck, tongue and upper eyelid that had been
present for 3 weeks. Upon examination the patient appeared
lethargic and weak. The patient presented with a 2-year history of
slight postmenopausal bleeding and an 11-month history of a mild
sensation of suppression in the chest. The latter two symptoms were
so mild that the patient had previously paid no attention to
them.
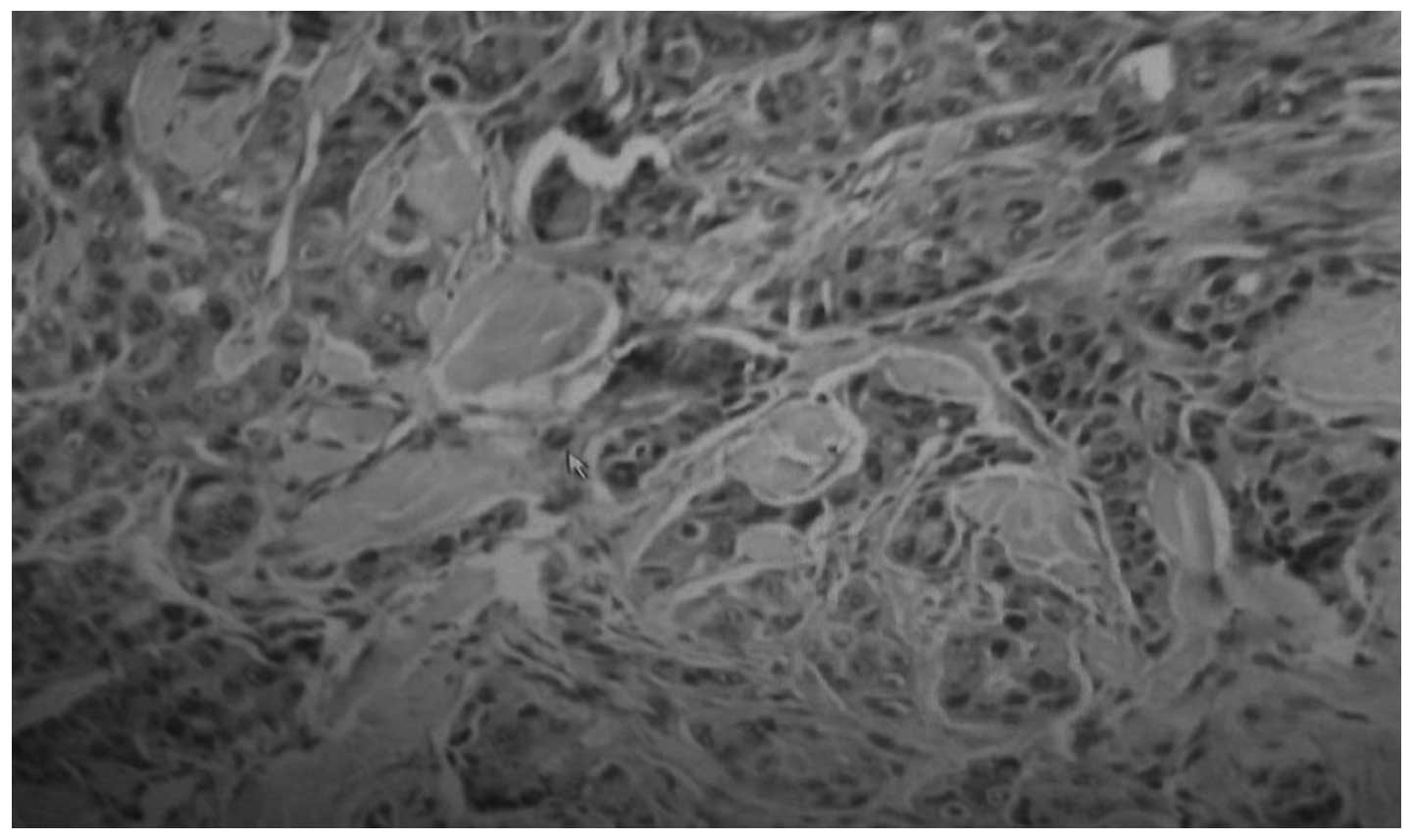
Biopsies of these nodules revealed metastatic
adenocarcinoma, and the immunohistochemical profile was consistent
with a digestive tract or ovarian origin, showing positive
expression results for cytokeratin (CK)8, CK18, CK7 and CK20, and
negative results for CK125, p63, gross cystic disease fluid
protein-15, thyroid transcription factor-1, synaptophysin,
chromogranin A and hepatocyte paraffin 1 (Fig. 1). An enhanced abdominal computed
tomography (CT) scan showed multiple subcutaneous metastases
(Fig. 2) in the left kidney, right
adrenal gland and liver. CT of the thorax revealed a solitary
tubercle-like mass, 1 cm in diameter, at the inferior lobe of the
right lung, and color doppler ultrasound of the pelvic cavity
depicted no abnormalities.
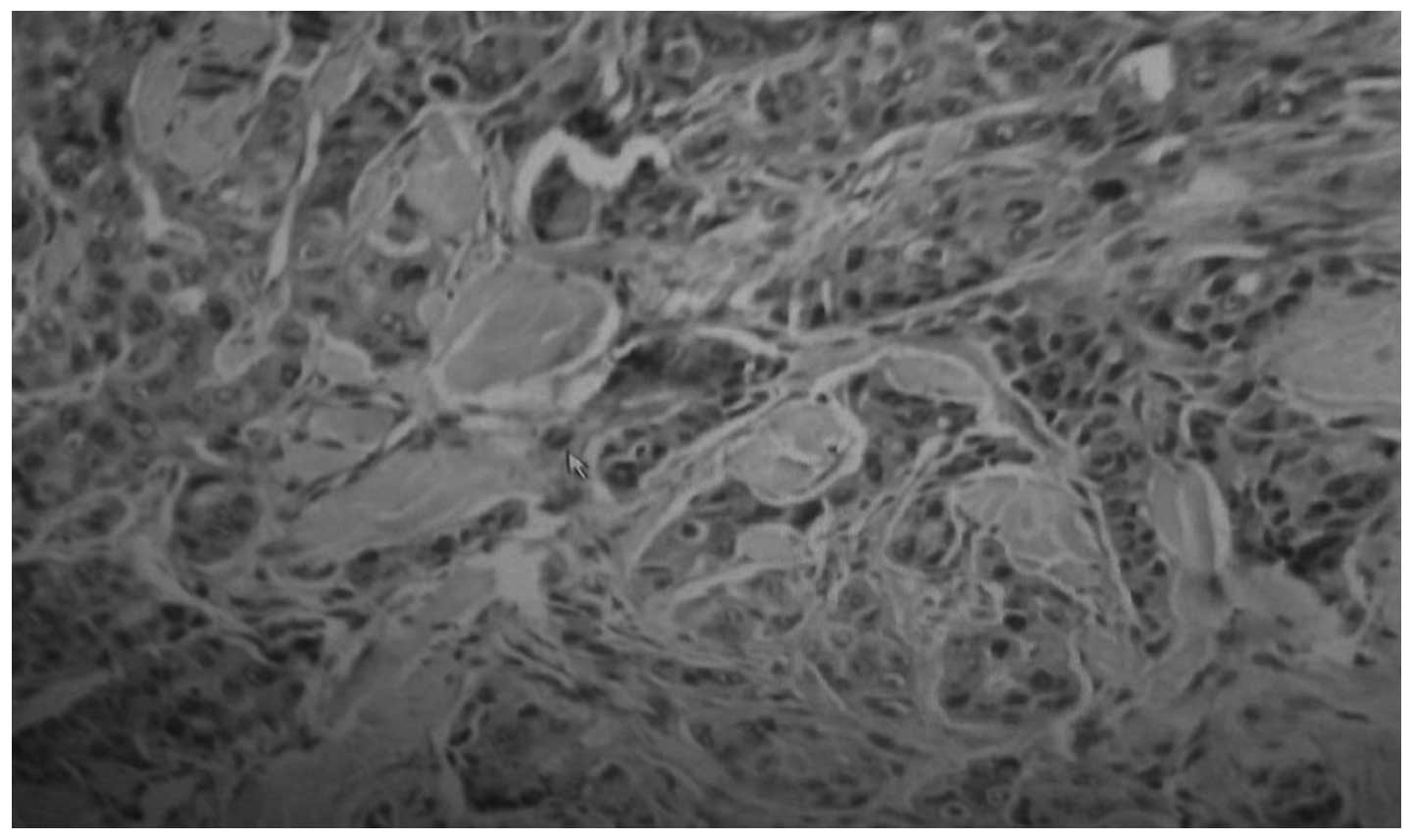 | Figure 1Biopsy of the nodules revealed
metastatic adenocarcinoma, and the immunohistochemical profile was
consistent with a digestive tract or ovary origin, showing the
following expression results: Cytokeratin (CK)8(+), CK18(+),
CK7(+), CK20(+), CK125(−), p63(−), gross cystic disease fluid
protein-15(−), thyroid transcription factor-1(−), synaptophysin(−),
chromogranin A(−) and hepatocyte paraffin 1(−). |
The patient was referred to the First Affiliated
Hospital of Liaoning Medical University for treatment of metastatic
disease and due to serious weakness. Upon admission, the laboratory
findings indicated leukocytosis (21.00×109/l), anemia
(113.00 g/l), thrombocytopenia (89.00×109/l),
hyperkalemia (5.78 mmol/l) and hyperphosphatemia (1.94 mmol/l),
while the calcemia level was 2.44 mmol/l. The renal parameters were
increased as follows: Creatinine, 112.87 μmol/l; urea, 21.22
mmol/l; uric acid, 616.00 μmol/l; and bicarbonate radical, 19.60
mmol/l. The liver parameters were: Alanine transaminase, 41.00
IU/l; aspartate transaminase, 65.00 IU/l; and alkaline phosphatase,
662.00 IU/l. The level of the majority of the tumor markers was
markedly increased: Carcinoembryonic antigen, 254.30 ng/ml; cancer
antigen (CA) 125, 3382.00 U/ml; CA72-4, 340.00 U/ml; CA19-9,
1480.00 U/ml; CA15-3, 94.30 U/ml; neuron-specific enolase, 66.05
ng/ml; and squamous cell carcinoma antigen, 345.70 ng/l. TLS was
diagnosed and chemotherapy was delayed. The patient was supervised
by cardiac monitor. Hemodialysis was not performed immediately as
the patient’s family refused to consent to the treatment. Due to
the change in electrolyte levels, a high level of uric acid and a
low lever of bicarbonate radical, high doses of allopurinol,
calcium and potassium-binders were administered intravenously.
Bicarbonate was administered to compensate for metabolic acidosis.
However, the patient became progressively more tachypneic. In the
second week of hospitalization, the patient developed tachycardia,
with a pulse rate of 130 beats/min, and hypotension, with a
systolic blood pressure of 70 mmHg and a diastolic blood pressure
of 50 mmHg. Despite cardiopulmonary support, the patient died of
acute anuria renal failure at the end of the second week, with
general edema occurring at the end.
Discussion
To the best of our knowledge, cutaneous metastases
as distant metastases, often appear subsequent to the original
symptoms. The present case proved to be an exception in several
ways. The patient had minimal original symptoms despite suffering
from metastatic skin disease, and the primary origin could not
conclusively be determined prior to mortality. The mechanism of
distant metastasis, including cutaneous metastasis, is not fully
understood. Cutaneous metastasis occurs mainly via the hematogenous
and lymphatic routes, and it is indicative of an extremely advanced
stage, with a poor prognosis. With regard to the patient, attempts
at treatment remain unsatisfactory and difficult (8,9).
Acute TLS is an life-threatening condition
characterized by severe hyperuricemia, hyperphosphatemia,
hyperkalemia, hypocalcemia, increased anion gap metabolic acidosis
and acute renal failure (10). TLS
has been described as a rare event, complicating the treatment of
aggressive hematological tumors (11). In solid tumors, TLS is even more
rare, and it has been reported to occur subsequent to therapy. Only
a few cases of spontaneous TLS in solid tumors have been described
(12–15). In the present patient, TLS appeared
at the time of admission, without any therapy having previously
been provided.
In the patient of the present study, the prognosis
was made worse by multiple general subcutaneous metastatic nodules,
with multiple organ metastases and high uric acid, serum potassium
ion and tumor marker levels, without serious original symptoms
prior to the evident weakness. Multiple metastases to the skin may
also be key for the early recognition of TLS, along with the
elevation of uric acid, serum potassium ion and phosphorus levels,
and acute oliguria renal failure. Renal impairment may have been
intensified by the nephrotoxic contrast material used during the
supportive treatment.
In conclusion, spontaneous TLS may develop during
the course of multiple cutaneous metastases as an atypical
presentation, and despite intensive treatment, the syndrome can
lead to fatality, particularly in elderly individuals. In a
previous study, all patients >60 years of age with acute
spontaneous TLS succumbed shortly after presentation (16). Oncologists should be aware of the
potential complications presented in the present study of multiple
subcutaneous metastases accompanied with TLS, for the treatment of
advanced tumors with rapidly progressive and high-volume
choriocarcinoma. Further studies are required to elucidate the
mechanisms behind cutaneous metastasis and spontaneous TLS at the
molecular level, and to analyze potential molecular biomarkers in
order to identify which patients are most likely to develop
spontaneous TLS. We believe that it is important to make such rare
cases known and also to identify a breakthrough therapy for
advanced malignant tumors.
References
|
1
|
Savk E, Kolay A, Meteoglu I, et al:
Cutaneous metastatic adenocarcinoma arising from a malignant
sacrococcygeal teratoma in an adult. Dermatol Online J.
14:32008.
|
|
2
|
Lookingbill DP, Spangler N and Sexton FM:
Skin involvement as the presenting sign of internal carcinoma. A
retrospective study of 7316 cancer patients. J Am Acad Dermatol.
22:19–26. 1990.
|
|
3
|
Lookingbill DP, Spangler N and Helm KF:
Cutaneous metastases in patients with metastatic carcinoma: a
retrospective study of 4020 patients. J Am Acad Dermatol.
29:228–236. 1993.
|
|
4
|
Kalmykow B and Walker S: Cutaneous
metastases in breast cancer. Clin J Oncol Nurs. 15:99–101.
2011.
|
|
5
|
Chapman-Fredricks J, Blieden C, Sandoval
JD, Ernani V and Ikpatt OF: Acute spontaneous tumor lysis syndrome
as the initial presentation of ALK-positive diffuse large B-cell
lymphoma. Appl Immunohistochem Mol Morphol. 22:317–321. 2014.
|
|
6
|
Locatelli F and Rossi F: Incidence and
pathogenesis of tumor lysis syndrome. Contrib Nephrol. 147:61–68.
2005.
|
|
7
|
Vodopivec DM, Rubio JE, Fornoni A and Lenz
O: An unusual presentation of tumor lysis syndrome in a patient
with advanced gastric adenocarcinoma: case report and literature
review. Case Rep Med. 2012:1–12. 2012.
|
|
8
|
Charalambous C, Zipitis CS and Midwinter
M: Gastric adenocarcinoma metastatic to the skin: a report. Eur J
Cancer Care (Engl). 11:143–144. 2002.
|
|
9
|
Sun J, Gao Q and Fan VT: Multifocal
cutaneous metastases from squamous cell carcinoma of hard palate.
Int J Oral Maxillofac Surg. 41:807–809. 2012.
|
|
10
|
Tufan A, Unal N, Koca E, Onal I, Aksu S
and Haznedaroglu I: Spontaneous tumor lysis syndrome in a patient
with diffuse large B cell lymphoma and Richter syndrome. Ann
Hematol. 85:183–184. 2006.
|
|
11
|
Altman A: Acute tumor lysis syndrome.
Semin Oncol. 28(2 Suppl 5): 3–8. 2001.
|
|
12
|
Sklarin NT and Markham M: Spontaneous
recurrent tumor lysis syndrome in breast cancer. Am J Clin Oncol.
18:71–73. 1995.
|
|
13
|
Woo IS, Kim JS, Park MJ, et al:
Spontaneous acute tumor lysis syndrome with advanced gastric
cancer. J Korean Med Sci. 16:115–118. 2001.
|
|
14
|
Feld J, Mehta H and Burkes RL: Acute
spontaneous tumor lysis syndrome in adenocarcinoma of the lung: a
case report. Am J Clin Oncol. 23:491–493. 2000.
|
|
15
|
Jasek AM and Day HJ: Acute spontaneous
tumor lysis syndrome. Am J Hematol. 47:129–131. 1994.
|
|
16
|
Hsu HH, Chan YL and Huang CC: Acute
spontaneous tumor lysis presenting with hyperuricemic acute renal
failure: clinical features and therapeutic approach. J Nephrol.
17:50–56. 2004.
|