Introduction
The main causes of mortality for patients with
hepatocellular carcinoma (HCC) are cancer progression, tumour
recurrence and metastasis. Emerging treatment options, such as
surgery, interventional radiology, ethanol injection and
radiofrequency ablation, have improved the prognosis of HCC
(1); however, there are few
treatment options for extrahepatic metastases, for which the
prognosis is poor. The incidence of extrahepatic metastasis among
all HCC patients is reported to be >25%, with the lungs,
diaphragm, abdominal lymph nodes and bone recognized as the most
frequently affected areas (2).
Current treatment options for metastases include surgical excision,
radiotherapy, and chemotherapy. Surgical excision may benefit
patients with single or regional lesions; however, it is unsuitable
for patients with multiple lesions. This report describes a patient
for whom a solitary lacrimal gland tumor was the first symptom of
HCC. A craniectomy was performed and the mass was totally removed.
The histological diagnosis was lacrimal gland metastasis from HCC.
The patient was subsequently treated by transcatheter arterial
chemoembolization (TACE). To the best of our knowledge, there have
been no previoulsy reported cases of lacrimal gland metastases from
HCC. Only one case of metastasis to the lacrimal sac from a renal
cell carcinoma has been reported (3). The current study presents the first
case of this unusual metastatic spread of HCC.
Case report
A 56-year-old male was admitted to Shandong Cancer
Hospital and Institute (Jinan, China) due to a 15-day history of
epiphora associated with a non-tender 35×30-mm pulsatile mass in
the right lacrimal gland and the loss of 3 kg of weight in one
month. Upon physical examination, the patient was conscious with
normal vision, but exhibited optic nerve palsies and
hepatosplenomegaly, with no signs of ascites. The liver was
palpable ~5 cm below the right costal margin, with a hard and
irregular edge. The spleen was marginally enlarged. The superficial
lymph nodes were not enlarged. Furthermore, the complete blood
count, clotting profile, blood glucose level and liver and renal
function tests were normal. However, the serum α-fetoprotein level
was elevated to 2,420 ng/ml, and the hepatitis B virus surface
antigen status was positive. Chest X-ray results were normal,
however, the abdominal ultrasonography revealed a solid 7.5×5.5-cm
mass in the right hepatic lobe, while the remainder of the liver
was normal. Computed tomography (CT) images revealed a smooth
circular lesion in the right orbit and a mucosal cyst in the left
maxillary sinus, which required further examination. In addition,
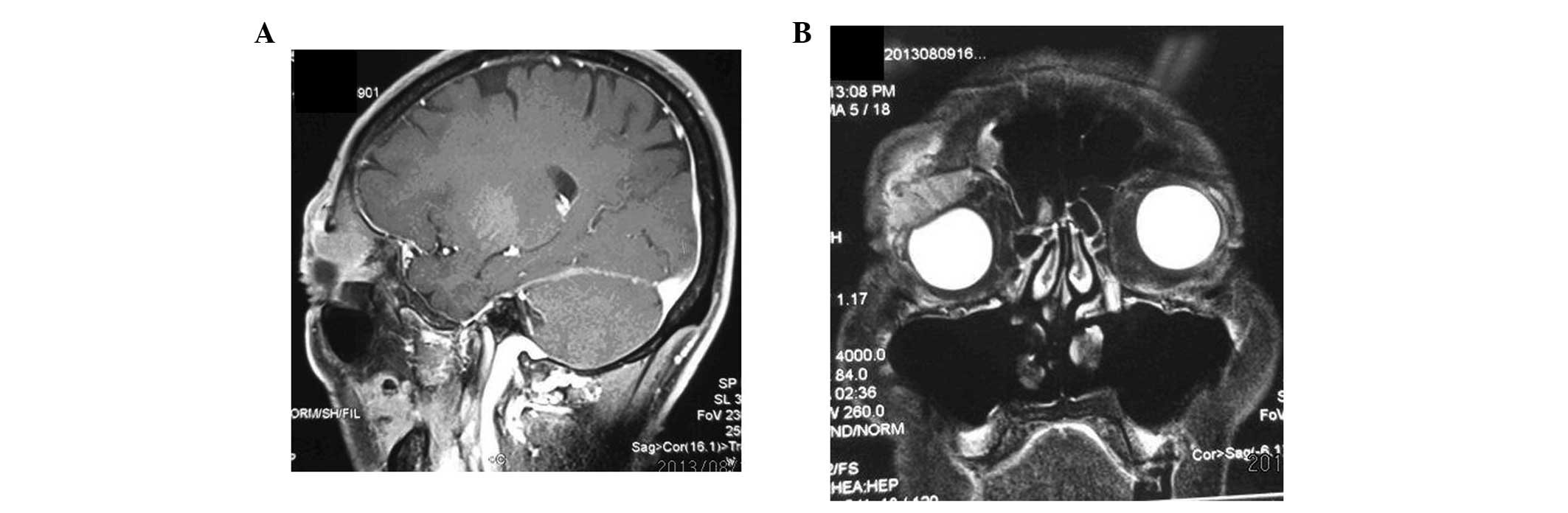
magnetic resonance imaging (MRI) scans revealed a smooth circular
lesion within the right lacrimal gland and right frontal plate
barrier, indicating the possibility of a metastatic tumor or
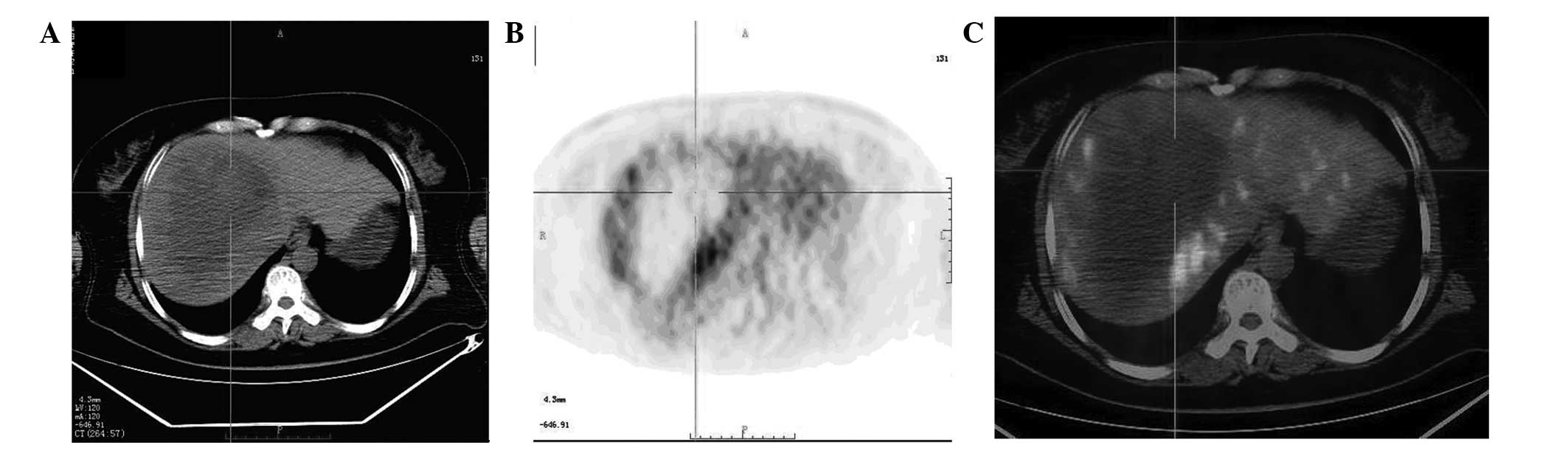
primary lacrimal migraine invasion (Fig. 1). 18F-fluorodeoxyglucose
positron emission tomography/CT revealed high uptake in the right
lacrimal gland and right orbital bone, and heterogeneous uptake in
the right lobe, indicating a puncture (Fig. 2). The tumor was excised and the
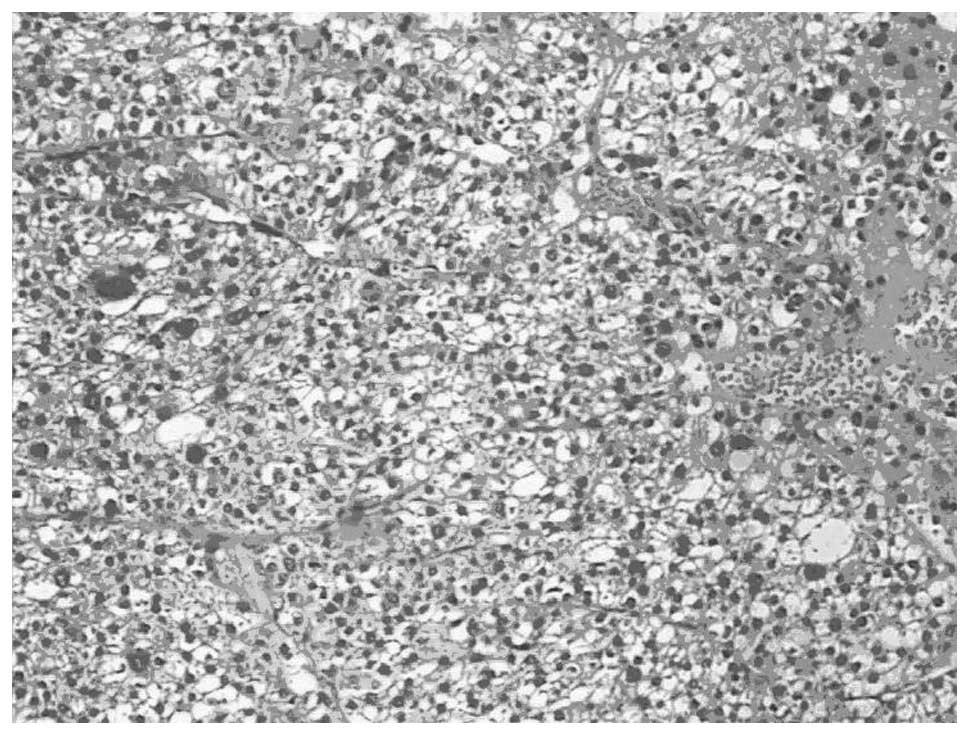
pathological analysis showed a poorly-differentiated clear cell
carcinoma. A histological review of the resected specimen revealed
a metastatic HCC (Fig. 3), with
broad-spectrum immunohistochemical staining for CK (+), GPC-3 (+),
HMB45 (−), CK7 (−) and CK8/18 (−).
The carcinoma was radically resected with the
surrounding normal tissue under general anesthesia.
Histopathological examination of the carcinoma revealed pleomorphic
tumor cells with eosinophilic cytoplasms and prominent nucleoli and
mitosis arranged in trabecular and solid pattern which confirmed
the diagnosis of metastasic HCC. Following seven days rest, the
patient was treated with TACE, consisting of 30 mg epirubicin, 50
mg cisplatin and 10 ml iodized oil and clinically monitored for
disease progression. Recent studies have demonstrated that TACE
effectively controls the symptoms of advanced HCC, even in patietns
with vascular invasion or metastases (4,5). Due
to the fact that there was only a single lacrimal tumor, the
patient did not undergo radiotherapy. Postoperative recovery was
satisfactory. The patient was discharged one month later. After six
months of follow-up the patient did not exhibit any evidence of
recurrence in the lacrimal gland. However, the patient exhibited
recurrence of the HCCs and succumbed to liver failure in the 12
months after receiving TACE.
Discussion
HCC exhibits a widely varying incidence in different
countries, however, its worldwide prevalence makes it one of the
most common malignancies. HCC occurs most frequently in elderly
males with alcoholic liver cirrhosis. In total, >50% of HCC
cases result in extrahepatic metastases (6,7), which
occur most frequently in the lungs, adrenal glands and regional
lymph nodes (8,9), but rarely in the lacrimal gland.
Metastases to the lacrimal gland are extremely rare, however, when
they do occur, they appear as exophytic tumors, and rarely with
bone changes. In the current study, the patient presented with a
non-tender pulsatile mass in the right lacrimal gland, and was
experiencing pain and an eye movement disorder. Besides the
non-typical clinical presentation, the MRI appearance of the
lacrimal gland may also aid in the differential diagnosis between
cystic carcinoma and metastases, however, the final diagnosis
relies on the histopathology or cytology. In the present case, the
patient was diagnosed with a metastatic HCC tumor of the lacrimal
gland, which was confirmed by biopsy. Thus far, no studies have
investigated therapeutic approaches for the treatment of lacrimal
gland metastatic disease. The current patient was treated with TACE
and clinically monitored for disease progression. Current treatment
options for lacrimal gland metastases of HCC or non-HCC include
surgical excision, radiotherapy and chemotherapy. Surgical excision
may benefit patients with single or regional lesions. However, for
HCC patients with >2 metastatic lesions surgery and radiotherapy
are unsuitable due to excessive radiation damage to the surrounding
tissue (10). Chemotherapy is
suitable for patients with multiple lesions, but it is not
particularly sensitive and has a poor prognosis (11,12).
In conclusion, the current study presents a case of
unusual HCC metastasis in the lacrimal gland. The clinical
diagnosis was difficult, however, metastasis must always be
considered in patients with a history of malignancy. Laboratory and
imaging studies do not aid the diagnosis and therefore, only
fine-needle aspiration and/or biopsy may confirm it. The
therapeutic options for this condition have not been well-studied
and the effects require further follow-up.
References
|
1
|
Gwak GY, Jung JO, Sung SW and Lee HS:
Long-term survival after pulmonary metastatectomy of hepatocellular
carcinoma; treatment outcome or natural history?
Hepatogastroenterology. 51:1428–1433. 2004.
|
|
2
|
Uchino K, Tateishi R, Shiina S, et al:
Hepatocellular carcinoma with extrahepatic metastasis: clinical
features and prognostic factors. Cancer. 117:4475–4483. 2011.
|
|
3
|
Vozmediano-Serrano MT, Toledano-Fernández
N, Fdez-Aceñero MJ, et al: Lacrimal sac metastases from renal cell
carcinoma. Orbit. 25:249–251. 2006.
|
|
4
|
Chung GE, Lee JH, Kim HY, et al:
Transarterial chemoembolization can be safely performed in patients
with hepatocellular carcinoma invading the main portal vein and may
improve the overall survival. Radiology. 258:627–634. 2011.
|
|
5
|
Takayasu K, Arii S, Ikai I, et al: Overall
survival after transarterial lipiodol infusion chemotherapy with or
without embolization for unresectable hepatocellular carcinoma:
propensity score analysis. Am J Roentgenol. 194:830–837. 2010.
|
|
6
|
Chang L, Chen YL and Kao MC: Intracranial
metastasis of hepatocellular carcinoma: review of 45 cases. Surg
Neurol. 62:172–177. 2004.
|
|
7
|
Li R, Walvekar RR, Nalesnik MA and Gamblin
TC: Unresectable hepatocellular carcinoma with a solitary
metastasis to the mandible. Am Surg. 74:346–349. 2008.
|
|
8
|
Fujihara H, Chikazu D, Saijo H, et al:
Metastasis of hepatocellular carcinoma into the mandible with
radiographic findings mimicking a radicular cyst: a case report. J
Endod. 36:1593–1596. 2010.
|
|
9
|
Karamouzis MV, Melachrinou M, Fratzoglou
M, et al: Hepatocellular carcinoma metastasis in the pituitary
gland: case report and review of the literature. J Neurooncol.
63:173–177. 2003.
|
|
10
|
Lambert B, Van Vlierberghe H, Troisi R and
Defreyne L: Radionuclide therapy for hepatocellular carcinoma. Acta
Gastroenterol Belg. 73:484–488. 2010.
|
|
11
|
Natsuizaka M, Omura T, Akaike T, et al:
Clinical features of hepatocellular carcinoma with extrahepatic
metastases. J Gastroenterol Hepatol. 20:1781–1787. 2005.
|
|
12
|
Bruix J and Sherman M; American
Association for the Study of Liver Diseases. Management of
hepatocellular carcinoma: an update. Hepatology. 53:1020–1022.
2011.
|