Introduction
Vascular neoplasms usually occur in the visceral
organs including the liver, spleen and gastrointestinal tract and
occsionaly in the pancreas. A pancreatic vascular neoplasm is an
uncommon type of the primary cystic neoplasm (1). The occurrence of pancreatic
hemangiomas in adults is extremely rare. Adult pancreatic
hemangiomas often manifest as large cystic lesions in middle-age
females and in many cases the patients exhibit abdominal pain but
no evidence of malignancy (2,3),
therefore, accurate diagnosis is essential for their surgical
management, using techniques such as pancreatectomy, partial
pancreatectomy or non-resection. However, it is often difficult to
produce a final differential diagnosis of intraductal papillary
mucinous neoplasms, mucinous cystic neoplasms and solid
pseudopapillary neoplasms of the pancreas using ultrasound,
angiography, computed tomography, or magnetic resonance imaging in
preoperative diagnosis due to their fluidity. The present study
reports the case of an adult patient with a giant pancreatic
hemangioma without recurrence 6 years following curative surgery.
Additionally the report discusses the clinicopathological and
immunohistochemical data used to distinguish pancreatic hemangiomas
from other cystic lesions of the pancreas.
Case history
Patient history
A 40-year-old female visited St. Mary’s Hospital
(Kurume, Japan) with a chief complaint of abdominal pain. The
results of the physical examination were within the normal limits,
as were the levels of the two tumor markers, serum CEA and CA19-9.
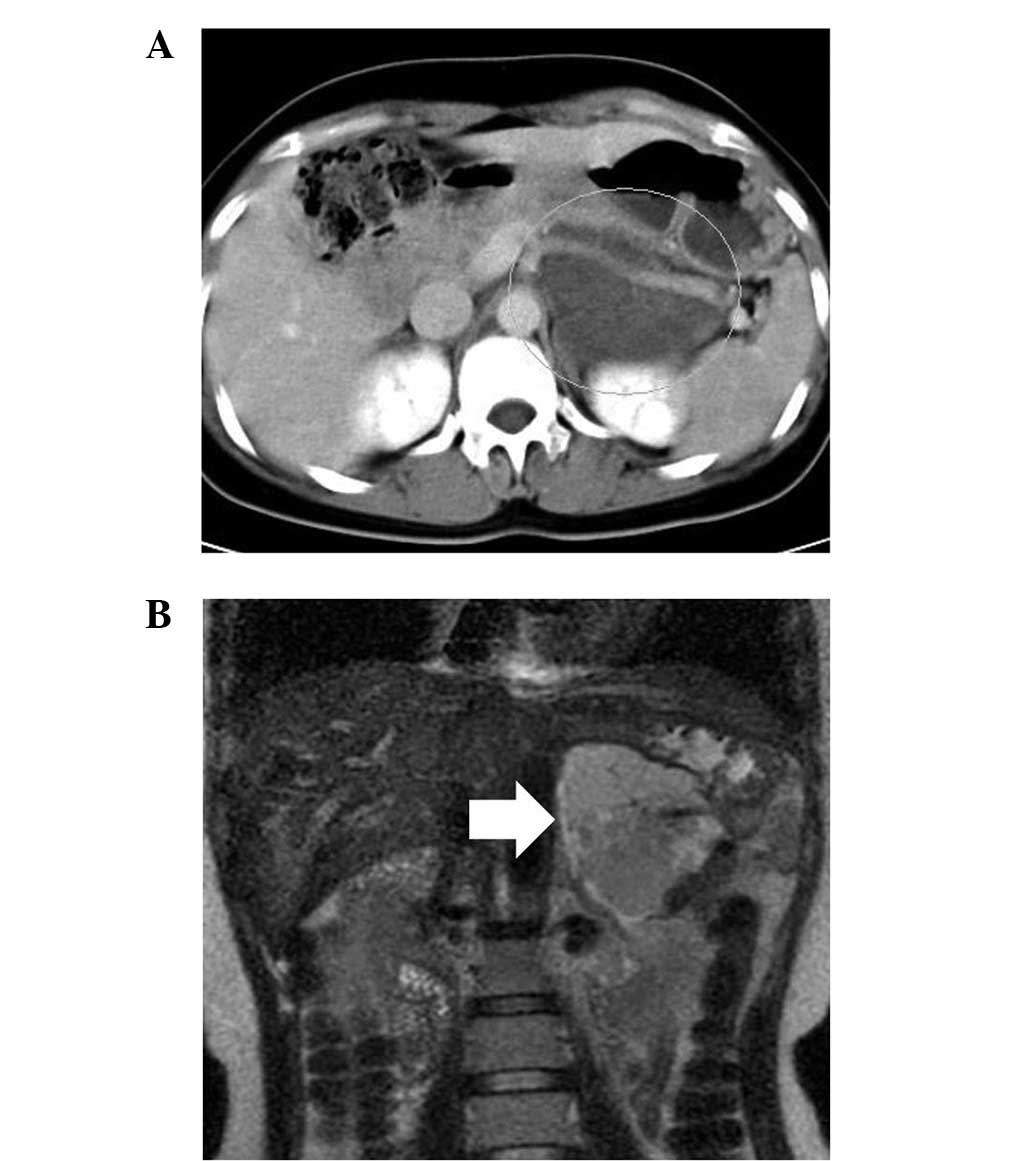
An abdominal computed tomography scan detected a well-defined
100-mm mass with low and high attenuation areas in the body and
tail of the pancreas. The tumor extended into the retroperitoneum
and surrounded the splenic vein (Fig.
1A). Magnetic resonance imaging showed a high-attenuation,
multilocular cystic mass with septa on T2-weighted imaging
(Fig. 1B). The case was reviewed in
a Multidisciplinary Surgery Conference at St. Mary’s Hospital, and
was diagnosed as a cystic neoplasm arising in the retroperitoneum
or pancreas.
Pathological findings
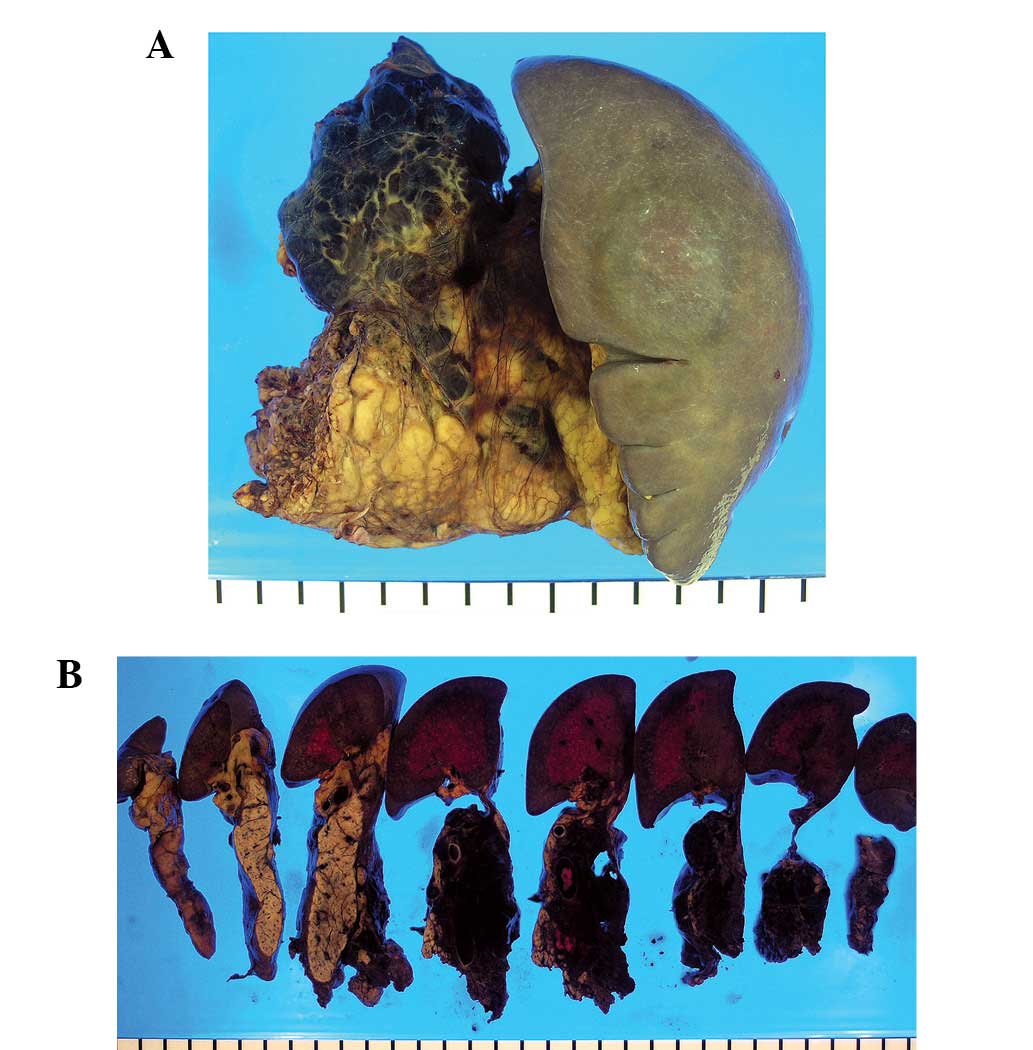
Macroscopically, the lesion was multiloculated with
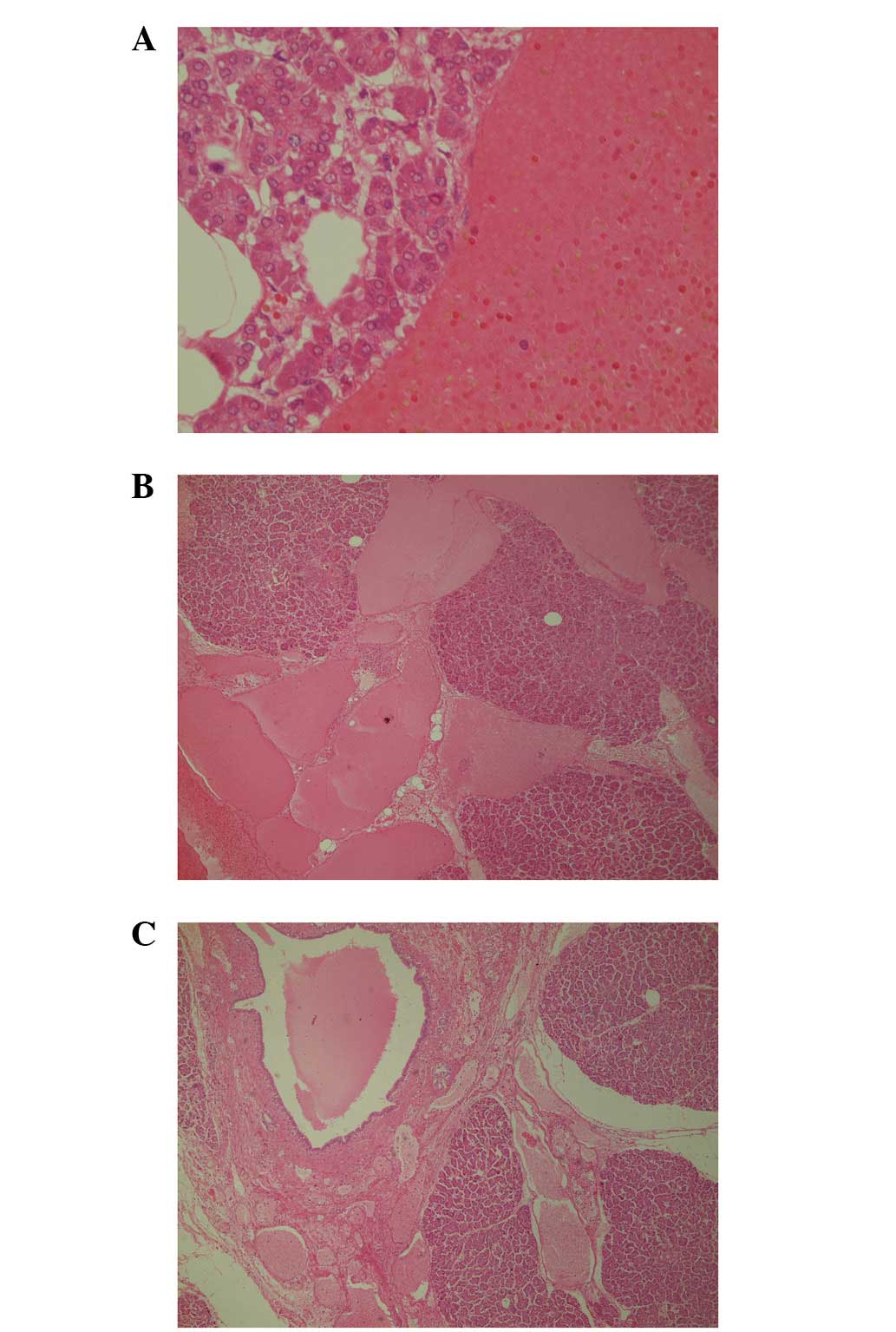
intracystic hemorrhage and no mucinous component (Fig. 2). Microscopically, the lesion was
composed of numerous and heterogeneous cysts lined by a flattened
single layer of cells without significant atypia (Fig. 3A). The cysts extended into the
interlobular septa of the pancreas and surrounded the main
pancreatic duct (Fig. 3B).
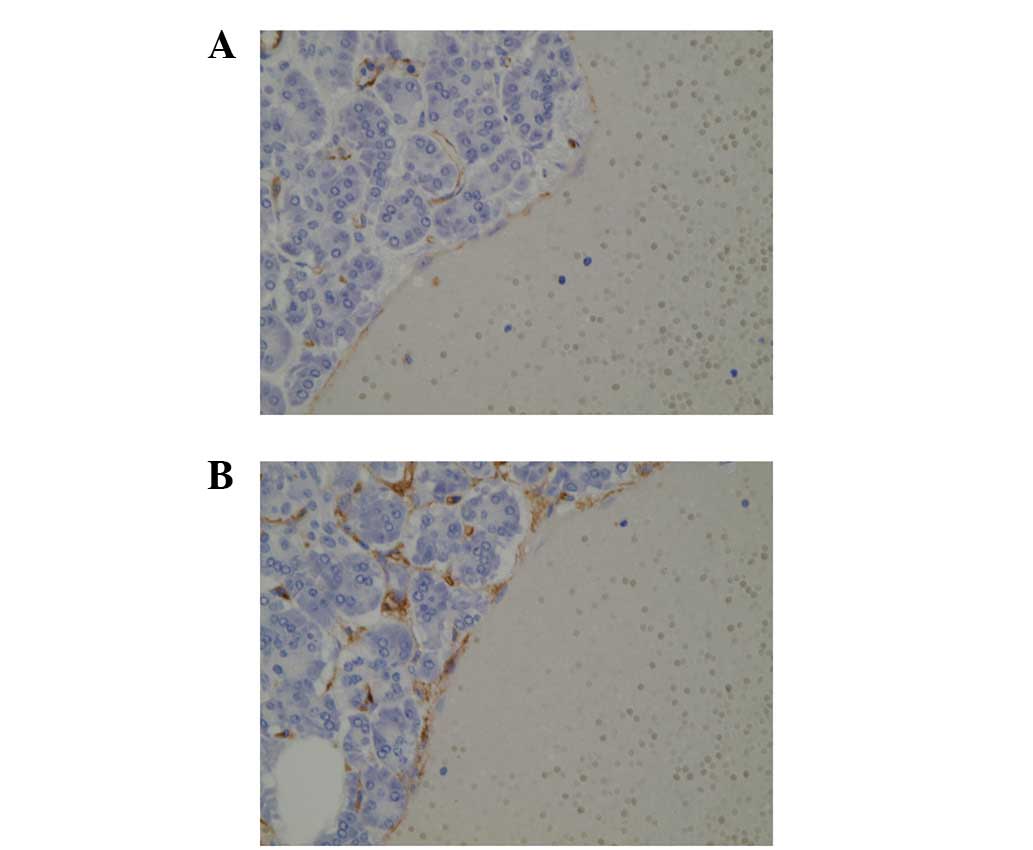
Immunohistochemical analysis showed that the cells lining the cysts
were expressing CD31 and CD34 (Fig.
4), but were negative for D2–40. Therefore, the lesion was
diagnosed as adult pancreatic hemangioma. The background pancreas
did not show changes associated with secondary pancreatitis, such
as active inflammation or severe atrophic changes of the pancreatic
lobules. In addition, the pancreas showed no pancreatic
intraepithelial neoplasia (PanIN) lesions. All nodes and margins
were negative for neoplasms.
Treatment and follow up
Following full explanation of the findings, the
patient accepted the proposed surgical removal of the tumor.
Surgical exploration revealed an 85-mm mass in the pancreatic body
and tail that was inseparable from the pancreas. Consequently, a
pancreatectomy was performed. The postoperative course was
uneventful and six years later, the patient had experienced no
recurrence. Patient provided written informed consent.
Discussion
Pancreatic vascular neoplasm is an uncommon type of
primary cystic neoplasm (1). Most
pancreatic hemangiomas arise in childhood. Vogel et al
(3) reported that all the patients
with lesions involving the pancreas were <3 years old in a set
of 5,051 patients with vascular anomalies. Hemangiomas are reported
to proceed in three steps in childhood (4): i) The proliferating phase, which
involves a rapid proliferation of the capillaries that lasts up
until the age of one year; ii) the involuting phase, in which
growth slows and shows inevitable regression until the child is one
to five years old; and iii) the involuted phase, whereby
improvement continues until the age of 6–12 years, and finally a
hemangioma may produce a fibro-fatty residuum by adulthood. Thus,
pancreatic hemangioma is a rare disease in adults.
A few adult pancreatic hemangiomas have been
reported. As reviewed by Mundinger et al in 2009 (2), only nine cases had been reported since
1939 (5–12) and five potential cases were reported
prior to 1939. Patients with adult pancreatic hemangiomas are
frequently females with a mean age of 55 years, and the hemangiomas
are generally large in size, ranging from 3 to 20 mm (2). Most patients with pancreatic
hemangioma have abdominal symptoms and a number are severe
(2,6–12).
Vascular neoplasms in this area are almost benign, even in patients
with severe clinical symptoms, and surgical removal of the lesion
may be necessary once diagnosed.
The two most common types of cystic neoplasm of the
pancreas are the intraductal papillary mucinous neoplasms and
mucinous cystic neoplasms of the pancreas, and these neoplasms have
malignant potential (1,13,14).
However, the adult pancreatic hemangiomas that have been reported
since 1939 have shown no malignant potential.
Generally, adult pancreatic hemangiomas are composed
of cysts lined by a single layer of uniform endothelial cells that
express CD31 and CD34 (2). The case
reported in the present study was also composed of numerous cysts
lined by neoplastic endothelial cells positive for CD31 and CD34.
Therefore, CD31 and CD34 may be useful markers to discriminate
between an adult pancreatic hemangioma and other types of cystic
neoplasm, particularly cystic lymphangiomas. Notably, in the
present case, the neoplastic vessels extended into the interlobular
septa of the pancreas and surrounded the main pancreatic duct;
however there was no invasion or obstruction of the major
pancreatic duct. No changes associated with pancreatitis or
precursor lesions of pancreatic cancer, the so-called PanIN
lesions, were observed. As an adult pancreatic hemangioma may
widely grow along the pancreatic interlobular septa, surgical
treatment may be required when imaging shows direct contact between
the lesion and the pancreatic tissue.
References
|
1
|
Le Borgne J, de Calan L and Partensky C:
Cystadenomas and cystadenocarcinomas of the pancreas: a
multiinstitutional retrospective study of 398 cases. French
Surgical Association. Ann Surg. 230:152–161. 1999.
|
|
2
|
Mundinger GS, Gust S, Micchelli ST,
Fishman EK, Hruban RH and Wolfgang CL: Adult pancreatic hemangioma:
case report and literature review. Gastroenterol Res Pract.
2009:8397302009.
|
|
3
|
Vogel AM, Alesbury JM, Fox VL and Fishman
SJ: Complex pancreatic vascular anomalies in children. J Pediatr
Surg. 41:473–478. 2006.
|
|
4
|
Takahashi K, Mulliken JB, Kozakewich HP,
Rogers RA, Folkman J and Ezekowitz RA: Cellular markers that
distinguish the phases of hemangioma during infancy and childhood.
J Clin Invest. 93:2357–2364. 1994.
|
|
5
|
Ranström V: Haemangioma cavernosum
pancreatis. Zentralbl Allg Pathol. 73:33–35. 1939.(In German).
|
|
6
|
Ringoir S, Derom F, Colle R and Mortier G:
Hemangioma of the pancreas. Report of a case. Gastroenterology.
41:43–45. 1961.
|
|
7
|
Colardyn F, Elewaut A, Van de Velde E and
Barbier F: Hemangioma of the pancreas. Tijdschr Gastroenterol.
15:260–267. 1972.
|
|
8
|
Mangin P, Perret M and Ronjon A:
Hemangioma of the pancreas. J Radiol. 66:381–384. 1985.(In
French).
|
|
9
|
Kobayashi H, Itoh T, Murata R and Tanabe
M: Pancreatic cavernous hemangioma: CT, MRI, US, and angiography
characteristics. Gastrointest Radiol. 16:307–310. 1991.
|
|
10
|
Dageförde J, Gmelin E and Otte M:
Hemangioma of the pancreas. Rofo. 154:332–333. 1991.(In
German).
|
|
11
|
Chang WT, Lee KT and Yang SF: Cavernous
hemangioma of the pancreas: report of a case. Pancreas. 26:310–312.
2003.
|
|
12
|
Plank C, Niederle B, Ba-Ssalamah A and
Schima W: Pancreatic hemangioma: Imaging features with
contrast-enhanced CT and with gadolinium- and mangafodipir-enhanced
MRI. Eur J Radiol Extra. 57:59–62. 2006.
|
|
13
|
Poultsides GA, Reddy S, Cameron JL, et al:
Histopathologic basis for the favorable survival after resection of
intraductal papillary mucinous neoplasm-associated invasive
adenocarcinoma of the pancreas. Ann Surg. 251:470–476. 2010.
|
|
14
|
Sohn TA, Yeo CJ, Cameron JL, et al:
Intraductal papillary mucinous neoplasms of the pancreas: an
updated experience. Ann Surg. 239:788–799. 2004.
|